PSYCHOSIS SCHIZOPHRENIA ORGANIC PSYCHOTIC OTHER
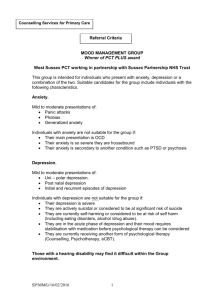
advertisement

PSYCHOSIS SCHIZOPHRENIA Positive: Delusions Hallucinations Disorganised speech Disorganised behaviour Negative: Affective blunting Aolgia: speech Avolition: motivation Asocial ORGANIC MEDICAL Hthyroid TBI Delirium Tumour Dementia PSYCHOTIC 1-6/12 = Schizophrenifor m Drugs: Amphetamines Pred Alcohol – Korsakoff Mood = Schizoaffective mood >1/12 each >6/12 Overall NEVER FORGET <1/12 = brief psychotic Delusional = less impact + no other symptoms OTHER MOOD Depression with psychosis = delusions of nilism (rotting), poverty (negative) Bipolar = grandiose delusions Post partum psychosis Anxiety Shared psychotic disorder = one dominant CLUES: 2+ voices Running commentary Bizarre delusions PD Schizotypal Schizoid Paranoid Borderline OCPD Factitious = have conversations Malingering ACUTE PSYCHOSIS Hx/Ex = Substance abuse, Thyroid, IVDU Bloods = FBE, UEC, BGL, LFT, TASH, B12 UDS, ECG Comorbid = D&A, Anxiety, Mania Social = occupation, financial, residential, relationship CHRONIC Hx/Ex = Compliance, SE, Substance abuse Ix= FBE, UEC, BGL, LFT, TSH, Vit D ECG Confirm Dx = reassess symptoms/risk/current MX Comorbid = Depression Social = carer burnout, home help Septic screen AFFECTIVE DSM DDX DEPRESSION >2/52 MANIA >1/52 or hospital SAD A FACES ORGANIC Metabolic = hThyroid Chronic condition Dementia Drugs = illicit, pred, alcohol GRANDIOSE ORGANIC Metabolic = HThyroid Drugs = illicit, prednisolone, dex, alcohol Delirium PSYCHOSIS = Schizoaffective (previous psychosis w/o mood) MOOD Depression with psychosis = guilt delusions Bipolar in depression phase = previous high Postpartum Premenstrual dysphoric disorder ANXIETY Comorbid Constant worrying Obsessions, compulsions Panic attacks Agoraphobia ADJUSTMENT = precipitating BEREAVEMENT PERSONALITY = just differential PSYCHOSIS Schizophrenia, schizophreniform, brief psychotic disorder Schizoaffective = previous w/o mood Shared psychotic MOOD Mixed = mania with depressive content Hypomanic = >4d but less social effect Post partum PERSONALITY Schiotypal Borderline Narcisstic Histrionic ADHD BIPOLAR DEPRESSION ACUTE MANIA = emergency – risk to reputation, relationship, finances – involuntary admission Identify organic cause Hx/Ex = compliance, substance use, thyroid Ix = FBE, UEC, LFT, ESR, Glucose, Urinalysis DDX = TFT, UDS, Serum Li/Valproate Assess = MSE, Risk, Alcohol/Drugs Acute Mania First-line: Olanzapine: 5mg PO → 10mg, max 30mg Risperidone: 0.5-1mg PO → 2mg, max 6mg Second-line: Haloperidol 1.5mg PO, max 10mg Other 2nd generation antipsychotics Lithium 750-1000mg PO Sodium valproate 200-400mg PO bd Carbamazepine 100-200mg PO bd Psychoeducation = Mania, Compliance, Substance abuse, Underlying medical condition CBT, Social rhythms therapy, Compliance therapy Social = Psychologist, Social work, D&A rehab Prophylaxis = 2+ episodes of mania or depression/ First episode severe Lifestyle= sleep, routine, food First-line prominent mania: Lithium 125-500mg PO bd for 2/52 then adjust based on serum Li First-line prominent depression: Lamotrigine 25mg PO nocte for 2/52 → 50g 2/52 → 100mg 1/52 → 200mg (half if combine with sodium valproate) First-line mania and depression: Olanzapine (5-30mg) Quetiapine (50-400mg bd) Second-line: Carbamazepine 200-400mg to 400-800mg Sodium valproate 400-500mg to 1.5-3g daily Monitor compliance: serum Li, valproate Monitor SE: kidneys, thyroid, Ca2+ Psychoeducation = mania, compliance, substance use, underlying medical condition CBT Social rhythms therapy Compliance therapy Social = Psychologist, Social work, D&A rehab DEPRESSION MANAGEMENT Identify organic causes Physical assessment: ● Comorbid medical conditions, e.g. HIV ● Cerebrovascular disease ● Thyroid Bloods: ● FBE, U&Es, LFTs, Cr, ESR, glucose, urinalysis DDx: TFTs, coeliac screen Assess: ● Premorbid personality ● Coping skills ● Risk: suicidality, homicidal, psychotic Comorbid: ● Alcohol and drugs: treat first ● Anxiety: treat with depression ● PD: treat parallel or w/ depression ● Insomnia MILD- MOD = GP managed – refer if inadequate response by 12wk/psychotic/suicidal/homicidal Treat and educate = Substance abuse ● Underlying medical condition Lifestyle =Good sleep, routine, food Medications = First-line (50% respond): ● SSRI, SNRI, mirtazapine Psychotherapy: ● CBT + ACT ● IPT ● Challenge negative thoughts Treat comorbid: ● OCD: desensitisation ● PTSD: eye movement desensitization ● Anxiety: CBT SEVERE = admit for high risk Same +/- ECT and bigger whammier drugs (diazepam, etc.) where they can be monitored Psychotic: trial of TCA + antipsychotic Right unilateral ECT with continuing or reinstating effective antidepressant May require lithium augmentation Experimental: DBS and TMS COGNITION DSM Onset Duration History LOC Attention Orientation Behaviour Psychomotor Sleep-Wake Mood/Affect Cognition Memory Language Delusions Hallucinations DEMENTIA Memory impairment Gradual Months to years Progressive, irreversible Normal Not initially affected Intact initially Disinhibited ImapiredADL Personality change Normal Fragmented Labile Decreased executive Paucity of thought Recent loss Agnosia, aphasia, decreased comprehension, repetition, speech echolalia Compensatory Variable Bland DELIRIUM Conscinsousness/Cognition change Acute Days to weeks Fluctuates, reversible PSEUDODEPRESSION Fluctuate Decreased Intact Difficulty concentrating Intact Self harm/sucidide Impaired, fluctuates Severe agitation/retardation Subacute Variable Recurrent, reversible Extremes/fluctuates Reversed Anxious, irritable, fluctuates Fluctuates Slowing EMW Depressed, stable Marked recent Dysnomia, dysgraphia, speech rambling, irrelevant, incoherent, subject change Recent Not affected Nightmarish Visual common Bizarre Nihilistic, somatic Less common Fluctuates ASSESS = identify organic cause Hx/Ex = underlying medical condition, chronic alcohol use Delirium bloods = FBE, UEC, CMP, Glucose, ESR, LFT, BUN, TSH, Vit B 12, Folate, Albumin, Urine MCS ECG, CXR, CT head, Tox screen, VDRL, HIV, LP, EEG, Blood cultures Dementia = FBE, UEC, LFT, TSH, Glucose, Lipids, VIt B12/D, VDRL, HIV, Hearing/vision CT = <60, rapid onset, recent head trauma, unexplained neuro sx DEMENTIA MX = Treat underlying medical cause Cholinesterase inhibitor = Donepezil Anorexia, NV, diarrhea, insomnia, cramp, dizzy, depression, lethargy, fatigue, tremor, incontinence, sweating Orientation cues + Education/Support Comorbid = depression, anxiety, psychosis Alzheimer’s Australia Vic Roads DELIRIUM = ABx Risperidone 0.5-2mg Assess 3-6/12 Carer help Olanzapien 2.5-10mg Low dose benzo = Lorazepam 0.5-1mg Withdrawal from alcohol = Diazepam Orientate = quiet, well lit, famililar face, room near nurse station CBT ANXIETY PANIC = recurrent unexpected panic attacks – reach peak within 1m Bio = autonomic (palpitations, sweating, trembling, shaking, SOB, dizzy), choking, chest pain, nausea, paraesthesia Psychological = impending doom, depersonalisation, derealisation, fear of losing control, fear of dying > 1/12 of = worry about attack/implication/behaviour change Agoraphobia = anxiety about being in places/situation where escape is difficult – avoid or endure panic ACUTE EPISODE ANXIETY RANDOMLY DISORDER WHEN WORRY ABOUT REPEAT AGORAPHOBIA = STAY INDOORS Psychosocial = supportive psychotherapy, relaxation techniques, CBT Biological = SSRI/SNRI start low, go slow GAD Blank mind Easy fatigue Sleep disturbance Keyed up Irritablility Muscle tension >3, more days than not 6/12 (1 in children) LONG TERM ANXIETY AND WORRY ABOUT VARIOUS THINGS DIFFICULT TO CONTROL BESKIM Lifestyle = caffeine and etOH avoidance, sleep hygiene Psychological = psychotherapy, relaxation, mindfulness, CBT Biological = BEnzo, SSRI/SNRI, TCA, Beta block Phobic Disorder = exposure to stimulus invariably provokes immediate anxiety response Recognises fear as excessive, unreasonable Situation avoided or endured Interfere with life Social phobia = fear of social or performance situation ACUTE EPISODIC ANXIETY ABOUT ONE THING RECOGNISES AS EXCESSIVE AND UNREASONABLE STAYS HOME TO AVOID SOCIAL Psychological = exposure therapy, desensitisation, insight orientation Bio = Beta block/Benzo in acute SSRI/MAOI/Clomipramie OCD Obsession= recurrent, excessive, intrusive, unwanted Compulsion = driven to perform, unrealistic, to neutralise, time consuming, not connected in realistic way >1 hour Interfere with life Psychological = CBT, desensitiation, flooding, thought stopping, implosion therapy Bio= SSRI higher and longer treatment, Risperidone/Haloperidol PTSD = exposed to traumatic event RE EXPERIENCE = dreams, flashbacks, feels realistic/reliving AVOIDING/NUMBING = avoid thoughts/feelings/conversations/activites/places - detached INCREASED AROUSAL = difficult falling/staying asleep, irritable, concentration, hypervigilance, startle >1/12 Psychological = CBT, systematic desensitisiation, relaxation, thought stopping Biological = SSRI, quetiapine/olanzapine, risperidone ASD = same as PTSD but 2d – 4w duration Initial state of daze = narrowing of attention, disorientation, in ability to comprehend PTSD but more acute ADJUSTMENT = emotional/behavioural sx in response to stressor within 3/12 of onset OUT OF PROPORTION DOES NOT PERSIST WHEN STRESSOR IS GONE - not >6/12 post stressor Rule out BPD ORGANIC ANXIETY CVS = Post MI, ARrhthmia, CHF, PE, MV prolapse Resp = Asthma, COPD, Pnemonia, Hyperventilation Endocrine = Hthyroid, Phaeo, hypoglycaemia, Hyperadrenalism, HParathyroid Metabolic = V B12, Porphyria Neuro – Neoplasm, vestibular dysfunction, encephalitis Intoxication = caffine, amphetamines, cocaine, thyroid drugs, decongestants Withdrawal = benzo, alcohol RULE OUT ORGANIC NEVER FORGET DRUG OTHER PSYCH CAUSES Psychotic = delusions causing anxiety Mood = comorbid depression – irritable mania Personality disorder = Avoidant, Dependent Somatoform disorder Factitious Malingering = want BENZO PERSONALITY = enduring pattern of inner experience and behaviour that deviates markedly from expectations of individual’s culture Two or more of: Cognition Affect Interpersonal functioning Impulse control Inflexible and pervasive across range of situations Distress or marked functioning for those around them Pattern is stable A – MAD = odd, eccentric, withdrawn Familial a/w psychotic disorder Defence = intellectualisation, projection, magical thinking Paranoid (0.5-3%) = distrustful Schizotypal (3-5%) = eccentric Schizoid = loner B – BAD = dramatic, emotional, inconsistent Familial a/w mood disorder Defence = denial, acting out, regression, splitting, projective identification, idealisation Borderline (2-4%) = ambivalent Narcissistic (2%) = grandiose Histrionic (1-3%) = dramatic Antisocia (3%) = remorseless C – SAD = anxious, fearful Familial a/w anxiety disorder Defence = isolation, avoidance, hypochondriasis Avoidant (0.5-1.5%) = ashamed Dependent (1.6-6.7%) = clingy Obsessive-Compulsive (3-10%) = perfectionist EATING DISORDER = 5 year duration Mortality = 20% after 20 years Natural = cardiac/infection 4 times Suicide = 32 times First degree female relative = 10 times 5 times general population ANOREXIA = refusal to maintain body weight Fear of gaining weight Disturbed body image Amenorrhoea 1% Restricting vs. Binge/Purge Patients near to death often look well: ● BMI: <13 high risk ● Weight loss: >1kg/w for a month Physical assessment: ● Height, weight, BMI ● Centile charts for <18y ● HR and BP ● Core temperature ● Peripheries (circulation, oedema) ● CVS including postural BP ● Muscle power (sit up, squat, stand) Investigate complications of: ● Starvation (AN) ● Purging behaviour (dental) ● Associated physical complications (DM, pregnancy) ● Excessive exercise ● Stunted/incomplete development (MSK, reproductive) ● Dietary imbalance (high fibre, low fat) Bloods: ● FBE, U&Es, LFTs, Cr, ESR, glucose, urinalysis ● Ca, Mg, PO4, serum proteins, CK ● DDx: TFTs, coeliac screen, FSH, LH, prolactin ● Nutrition: B12, folate, vitamin D, Zn, Fe ● Beware: K+ (<3 mmol), low P+, hypoglycaemia (<3 mmol), Na+ (<125 mmol) Imaging: ● ECG ● CXR (DDx for weight loss/TB) DEXA (12mth of amenorrhoea) BULIMIA = recurrent episode of binge – inappropriate compensatory behaviour 2-4% Purge vs. Non purge Admit to hospital for high risk where resuscitation required Outpatient: ● Psychological and physical assessment at least every 6mth ● If deteriorate or no significant improvement, up intensity (individual → individual + family → inpatient) Inpatient: ● Resuscitation ● Nutritional support ● Beware refeeding syndrome ● Structured symptom-focussed treatment regime expecting weight gain - explain and agree on target inhospital weight and promise not to go over Weight: ● 0.5-1kg/w inpatient ● 0.5kg/w outpatient ● 3500-7000 extra calories/w ● May multivitamins/mineral ● Total parenteral nutrition is no unless significant GIT dysfunction ● Feeding against will - last resort Medication: ● None - comorbid depression/OCD may resolve with weight gain ● Beware drugs that prolong QT: ○ Antipsychotics ○ TCAs ○ Macrolide abx ‘-mycin’ ○ Some antihistamines ● Beware drugs that compromise cardiac ○ ECG if needed ● Put alert in file for med SE ● No oestrogen in kids (premature fusion of epiphyses) General: ● No physical activity - # risk ● Paeds referral in <18 for growth Psychotherapy = Reduce risk ● Encourage weight gain, healthy eating ● Facilitate psychological/physical recovery Outpatient: ● At least every 6 months if not more ● For at least 1 year post-discharge Inpatient: ● Psychological treatment Psychotherapies ● Focus on eating behaviour and attitudes ● FAMILY THERAPY: ○ Include siblings ○ Share information ○ Advice on behavioural management/set boundaries ○ Facilitate communication ● CBT: ○ CBT-BN 16-20 sessions 4-5mth ● Psychoeducation, etc. ● Evidence for: supportive psychotherapy, interpersonal therapy Long term supportive therapy ADOLESCENTS = HEEADSSS Home = whats home like? Who? Where? Stable? Education/Employment? = performance? Behaviour? Financially secure? Eating = diet? Perception? Weight change? Activities = How do you spend time? Dangerous behaviour? Peers? Drugs = Energy drink? Smoke? Alcohol? Drugs? Sex = Active? Contraception? Partners? STIs? Sexuality? Suicidality = Mood? Thoughts? Attempts? Risk? Safety = drink driving