Ebola Response 2014
advertisement

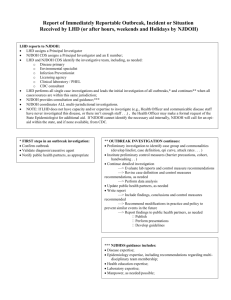
Ebola Response 2014 Nicole Mazur, MPH New Jersey Department of Health Communicable Disease Service Department of Health Structure DOH Public Health Services EEOHS CDS Epidemiology & Surveillance CDS ROLE • • • • • • • • • • Assist LHD with case investigations and contact tracing Guidance on disease epidemiology (transmission, incubation period, etc.) Clinical consultation on suspected cases Liaison with CDC and other states on inter-jurisdictional cases Provide technical guidance and resources for case evaluation & management Provide health education materials Coordination and consulting with other agencies Guidance on surveillance and monitoring Coordination of active monitoring of those with low but not no risk Monitoring persons with high, some, or low risk NJDOH CDS Ebola Response Team • Administration • Clinical • Epidemiology • Laboratory Testing • Communications • IT Support EVD Affected areas As of October 29th Widespread Transmission Guinea Sierra Leone Liberia Travel-associated Case(s) and Localized Transmission Nigeria* Spain^ United States^ Travel-associated Case(s) Only Mali Senegal*^ *No longer risk of transmission in these countries ^Persons traveling to these countries should not be considered to be at risk for exposure EVD Response and Preparedness • Airport Screening: • • • • • NYC- JFK Chicago- O’Hare Newark Atlanta Washington, DC- Dulles • 94% of flights from affected areas come through these airports • Nearly half come through JFK • Active Monitoring began at airports on October 16 (JFK earlier Oct 11) CDC Care kit Active Monitoring • New Jersey Department of Health, Communicable Disease Service • Recommendations for Follow‐Up of Ebola Virus Disease (EVD) • Low (but not zero) Exposure* • Reported from the CDC Division of Global Migration and Quarantine (DGMQ) • *Low (but not zero) exposure is defined as having been in a country in which an EVD outbreak occurred in the past 21 days and having had no exposure. LHD Responsibilities • LHD will provide a contact number for the person to report both daily temperature readings and possible symptoms • LHD will provide a 24/7 contact number to the person being monitored, should symptoms or questions arise. • The LHD should provide the name and location of hospital(s) near the person’s home or work. • Temperature reports will be entered into CDRSS, as well as any symptoms that arise Traveler Responsibilities • Individuals being monitored will need to consult with the LHD if there is any • planned travel out of the area for an extended period of time. • If symptoms arise or a recorded temperature of ≥100.4⁰F (38⁰C) is noted; individuals should: • Immediately isolate themselves (from people and pets), • CALL 9-1-1 to seek medical evaluation at a nearby hospital** • (persons should travel to the hospital via ambulance) • IMPORTANT!! • **Alert 911 to symptoms and recent travel to an Ebola‐affected area** Active monitoring Reporting Persons presenting to health care providers with fever or any other ebola symptoms AND travel to EVD-affected area within past 21 days should be IMMEDIATELY reported to the LOCAL HEALTH DEPARTMENT where the patient resides. If the local health department is unavailable please call New Jersey Department of Health- Communicable Disease Service. Contact Information • If you suspect EBOLA…. CALL PUBLIC HEALTH IMMEDIATELY! • How do you reach Local Health? • http://www.nj.gov/health/lh/documents/lhdirectory.pdf • Know your Local Public Health’s phone # and keep it on hand. • How do you reach State Health? 609-826-5964 Daily Monday - Friday 609-392-2020 Nights, Weekends and Holidays (Emergencies Only, Immediately Reportable Diseases) Outside of CDS • For questions pertaining to other issues not related to the Communicable Disease Service, Please call: • Office of Local Public Health • 609-292-4993 • dutyofficer@njlincs.net • Consumer, Environmental & Occupational • Health Service 609-826-4920 • EMS • 609-633-7777 • ems@doh.state.nj.us Resources • CDC website • http://www.cdc.gov/vhf/ebola/ • NJDOH website http://www.state.nj.us/health/cd/vhf/index.shtml Public Health Response to Ebola • • • • Surveillance Follow up for possible exposures Public Information Quarantine: Restriction of activities of well persons who have been exposed to a case of a communicable disease during its period of communicability • Isolation: The separation and confinement of individuals known or suspected to be infected with an infectious disease to prevent them from transmitting the disease to others • Contact Tracing The CDC “CARE” Kit—Check and Report Ebola--distributed to arriving air passengers Public Health Response Layered, Graduated, Risk-based • “Active Monitoring”—Local Health Departments will be checking in with people who have arrived from West Africa (usually by phone) for 21 days after arrival to see whether they develop symptoms (low risk travelers) • “Direct Active Monitoring” LHD visits or Skypes traveler to monitor for symptoms for 21 days (“some risk”) travelers. There MAY be restrictions on travel or public activities for that person. (partial quarantine) • “Direct Active Monitoring with Activity Restrictions and Travel Restrictions” LHD visits or Skypes traveler with high risk exposure for 21 days (Quarantine) Law Enforcement support of Public Health • NJSA 26: 4-2 and NJAC 8:57-1.1 give the Local Board of Health and the Health Officer the power to enforce these restrictions, and specify that they can call on local law enforcement to assist. • We may ask your assistance in locating and observing the location of a person under quarantine. • We are not asking you to arrest them. • We are not asking you to do anything that will expose you to the virus • Remember, a person under quarantine is not contagious (We are watching them to make sure they don’t become contagious– the firewall between those who are sick and the general public) “But what if they don’t cooperate?” • Inform the person they may be in violation • Document the action that the subject is taking • This is a civil court case, not an arrest • Call your Local Health Officer right away for additional guidance • Reality Check: a person who has a contagious case of Ebola is not going anywhere • Side note: Make our job easier--minimize the number of people who have contact with the person under quarantine Note: • This guidance will evolve as we learn more about this disease • Different diseases (i.e. TB) have different thresholds for Quarantine, depending on how it is spread • It’s the Health Officer’s statutory responsibility to take appropriate steps to stop the spread of communicable disease in the community • A historic and recognized power, with due process and right of appeal DOUGLAS J. VORNLOCKER DIRECTOR SOMERSET COUNTY OFFICE OF EMERGENCY MANAGEMENT OSHA 1910.132 – Personal Protective Equipment 1910.1020 – Bloodborne Pathogens Exposure Control Plan 1910.134 – Respiratory Protection RECOMMENDED PPE NJDOH PPE Recommendations for EVD 3 Levels: Basic – Middle – High Buddy System for Donning & Doffing – Trained Observer Develop Checklists that are specific to your needs and PPE Rigorous and Repeated Training No skin exposure when PPE is worn Availability is currently a limiting factor BASIC LEVEL Minimum PPE when providing direct care to sick traveler who came from a country with an Ebola outbreak Gloves Full face shield or goggles Surgical mask Long sleeve waterproof gown Shoe covers or waterproof boots MIDDLE LEVEL Healthcare Workers caring for EHF patients with potential contact with infected fluids and/or workers who can be splashed with blood/body fluids Full face shield with N-95 NIOSH approved respirator or higher Long sleeve waterproof gown or coveralls with integrated hood Impermeable shoe covers Waterproof boots 2 pair of disposable nitrile gloves – extended cuffs Single use impermeable apron covering torso to mid calf HIGH LEVEL Healthcare workers caring for EHF patients with severe respiratory involvement or undergoing aerosolgenerating procedures (includes EMS workers if intubation is a possibility) Powered Air Purifying Respirator with P-100 cartridges and hood Long sleeve waterproof gown or coveralls (with integrated hood if using N-95 APR) Impermeable shoe covers or waterproof boots 2 pair of disposable nitrile gloves – extended cuffs Single use impermeable apron covering torso to mid calf PREPAREDNESS Review OSHA Regulations and Achieve Compliance Determine Response Protocols and Procedures Based on Your Level of Potential Exposure Compare Your Inventory Against NJDOH & CDC Recommendations Acquire (at least order) PPE Train Train Train These are perishable skills that you will lose if you don’t practice Revise Your Response Protocols and Procedures TRAINING The Somerset County Emergency Services Training Academy is developing a PPE Considerations for Medical First Responders course. This course will include a section on the Rutgers School of Public Health’s Ebola PPE Training Courses will begin running during the week of 11/9/14