OCCUPATIONAL HEALTH NOTES (Helen)
OCCUPATIONAL HEALTH
Session 1
Exposure: physical, chemical and biological hazards such as dusts, airborne toxins, radiation and noise
Immunisation:
Health workers: Hep B, influenza, and triple of diptheria, tetanus & pertussis
Health workers caring for children: measles, mumps, rubella, varicalla & Hep A
Workers in contact with farm animals- Q-fever
Contraindications to Fluvax: o Allergic to eggs, antibiotics neomycin/polymyxin o SOB, wheezing/difficulty breathing o Swelling of face, lips, tongue/other parts of body o Skin rash, itching/hives o Temperature> 38.5 degrees, Children < 6 months
Stress in the workplace: o Workload, Work environment o Secondments: home life o Vocational training requirements o Family problems o Coping with dying pts/distressed & angry relatives
Bullying in the workplace: o Repeated, unreasonable behaviour towards an employee/s o Victimises, humiliates, undermines or threatens
Violence in the workplace:
1 in 12 GPs physically attacked by a patient
Factors for violence: drugs, alcohol, refusal to give pts scripts they sought, long waiting times
Violence most likely to occur: o Working with pts/clients who are in distress, intoxicated, disturbed/violent o Cash or drugs are kept/handled o denying someone a service o working alone/in isolation, working at night
Controlling risks: o Change physical characteristics of workplace
Install barriers, secure retreat, security devices etc o Change the systems of work
Limit cash/drug storage, always have staff available, ‘flag’ aggressive pts, train in aggression mngement o Personal/protective measures
Personal alarms, mobiles, protective equipment
Occupational Hx
Need to assess: o Fitness for work: assess abilities of pt and how this matches the requirements of the pt’s job o Aetiology ascertain whether job has anything to do with cause of pt problem
Components of an Occ Hx (see pp 50-51)
Present clinical condition
Relevant past history
Nature of jobs/duration of time in jobs
Physical/mental demands of job
Other issues that may cause harm/difficulty including extent of exposure
Activities at home
Financial aspects incl getting to work
Contacting employer
Return to work
- 20 days off, chance of going back is 70%
45 days off, 50%
70 days off, 35%
Suicide rate x^ in long-term worklessness
Session 2: Judging fitness for work
Q1: What are 2 things of central importance for you to know in order to assess a person’s fitness for work?
always ask- fit for what?
Must know o 1) Person’s abilities o 2) Have a clear idea of the role to be filled
Actively find out what it involves
In assessing a person’s fitness for work, must take fair account of the short term requirements of that role. o Must have reasonable justification for recommending exclusion of a person from a role
Factors that diminish a person’s fitness for work: o Reduced ability to perceive/judge o Loss of bodily function o Lack of stamina o Infectiousness
Assessing fitness of a person to undertake a particular role on behalf of an employer o Dr must:
1) Assess the person
2) Know the working conditions (may need to visit workplace)
3) Give recommendations & advice to the employer o Need to explain to person issues relating to confidentiality
You aren’t able to discuss your findings directly with them
Not involved in treating them
Pt must give informed consent to your contacting employer
Q2: What is the Austroads guide to assessing fitness to drive? How do you access it electronically? To what two major gps of drivers does it apply?
Medical conditions that affect ability to drive: o Momentary loss of consciousness- epilepsy/insulin-induced hypoglycaemia o Lapse of attentiveness: sleep disoder/medication for mental illness o Visual distortion: glaucoma/cataract
Private driving/commercial driving
Q3: Name three substance (or substance gps) for which occupational exposure may bring the need for periodical medical assessment
If exposed, require periodical checks of absorption/relevant bodily function o Lead o Asbestos o Isocyanates o Insecticides that inhibit cholinesterase
Workers exposed to loud noise must have periodical audiometric screening
Q4: What problem is likely to occur when a scanning test with a specificity of 0.9 is applied to a gp where the probability of finding a person with the screened-for condition is less than 1%. Why does this problem occur?
For any screening test to be valid, it must nearly-always show positive when the person being tested has the condition that is being sought
Following a chemical spill at a factory, management requests the screening of all 65 employees to ascertain whether anyone has had excessive absorption. However, the number of employees with excessive absorption is confidently expected to be fewer than five. For the purpose that it will be used, the chosen screening test has a sensitivity of
97% and specificity of only 80%.
What two factors in this scenario predict that a positive test result will more likely be false than true?
Your students should say:
The low prevalence (fewer than 5/65) that are likely to be affected;
The relatively low specificity of the test.
Your students have already covered this issue in the program that preceded occupational medicine in this semester on Evidence-based clinical practice
“Probability, odds and likelihood ratio” in the notes.
, however some may seek an explanation. Refer them to the heading
Prior Learning
In short, the odds that a screened person has the disease
section on pages 26 to 29 of their occupational medicine if their test is positive is odds of disease in the group to be tested × likelihood ratio of a positive test result.
The odds of disease in the group to be tested = 5/65
60/65 = 5/60 = 1/12.
The likelihood ratio of a positive test result = sensitivity/(1 – specificity) = 0.97/(1 – 0.80) = 4.9.
Therefore, the odds that a screened person has the disease = 1/12 × 4.9 = approx. 0.40
these odds could be expressed as 1 : 2.5 or, in whole numbers, 2 :
: 1. By multiplying by 2.5,
5. Simply expressed, this means that for every two positive test results that truly indicate abnormality, there will be five where the positive test result is misleading.
Q5: In regard to discrimination against a person seeking employment, when is it unfair? When is it fair?
Tests used to assess a person’s fitness for work must be appropriate to demands of the job o If standard is too rigorous, then could be unfair discrimination
To assess and not discriminate unfairly: o Be fully informed about the genuine & reasonable job requirements for the job applied for, and the abilities req to peform them o Outline what you intend to do, abilities/aspects of their health that will be tested, and how they relate to the req of their job
Say how only relevant aspects of applicant’s health will be relayed to emplyer o Ask about and test only aspects of applicant’s health that are strictly job-related/relate o to his/her ability to perform the requirements of their job
Outline the kinds of duties they would be expected to perform in their job and test for any conditions that would affect ability to perform these o Be aware employers are obliged to make reasonable accommodation for person with disabilities/impairments
o But not obliged to provide services/facilites that would impose an unjustifiable hardship on them
To enable assessment of what services & facilites can be provided, need to tell employer what services & facilities are required
Ask applicant if they req any assistance, services/facilities in order to perform requirements of job o Assess pt with disbilities using any service (i.e. prosthesis) they would routinely use to perform duties of their job o No tests to screen for injuries/disabilities/FHx that don’t affect ability of job o Supply only job-related health info to the employer o Keep all medical records confidential
Q6: What extent of medical information may be sent to the employer after an employer-requested medical assessment of a person’s fitness for work?
Q7: Why is it generally not appropriate to combine a medical examination for superannuation with a med exam for fitness for work?
Because fitness for employment differs from fitness to insure
- Fitness for employement: looks at present & short-term future & specific requirements of the job
- Fitness to insure: takes account risk factors that could exert their influence more slowly
Q8: What caution would you give to a teenager with a long Hx of atopic eczema who wants to be a hairdresser? Why?
Use moisturising cream regularly
Use a soap substitute
Limit the amount of wet work and hand washing performed
If possible, wash your hands in cool not hot water
Wear appropriate gloves to protect yourself from skin irritants. However, beware that occlusive gloves (tight-fitting, waterproof type gloves) may cause heat and sweating. Cotton gloves underneath are helpful. Also, change your gloves regularly.
Session 3
Compensation is separate from breach of safety rule. Therefore, given compensation regardless of fault.
Diseases typically classified as being occupational:
poisonings
zoonoses
pneumoconioses (dust diseases)
3 characteristics of an occupational disease:
1) a strong causal link b/w people with the disease & occupational exposure
2) clear diagnostic criteria for the disease
3) Majority of cases of the disease in a community may be attributed to occ exposure
Diseases covered:
ID: Anthrax, Hep A, Orf, Q fever, Leptospirosis
Toxic effects: Farms, underwater
Pneumoconioses: asbestosis, hypersensitivity pneumonitis, silicosis
Neoplasia: angiosarcoma of liver- vinyl chloride, leukaemia -ethylene oxide, malignant mesothelioma- asbestos
Dermatitis: occupational allergic contact dermatitis
Ambient pressure: underground/underwater avascular necrosis
Majority of long-incapacitated claims because of pain in back, neck, shoulder knee and hands
Employer obligations:
1) provide suitable or pre-injury employment for 12 months
2) plan a worker’s retuen to work
3) consult about return to work
4) co-operate with a labour hire firm if the employer is hosting a hired worker
1/ Differentiate impairment, disability & handicap. How can a severe impairment translate to a relatively minor handicap & vice versa?
Impairment: refers to a body part or organ system o i.e. decreased function of an organ/body part:
i.e. decreased range of movement of elbow
Disability: about what a person does o Lessened ability to do something i.e. reach or lift
Handicap assesses the person against what society expects of them o Incapacity for a role in society- i.e. unfit as a train driver
3 things when deciding about a patient’s return to work
1) Risk: chance of harm to patient/general public
2) Capacity- strength, flexibility, endurance
3) Tolerance- a pt’s ability to tolerate sustained work/activity at a given level which may be limited by injury
2/ Define the term ‘certificate’
A written declaration of the truth of a certain matter
3/ In response to your question, ‘What is your occupation?’ a patient replies, ‘I’m a research assistant.’ What is your next question?
Occupational history-taking for return to work
What is your job?
In this job, what do you actually do?
How long have you done these things?
Do you want to go back to work?
Do you think you would cope? In what ways could return to this work be difficult?
Ask about o Getting to work o Work layout o Loads o Stamina required o Hot/cold o Things to learn o Quality and tolerance of supervision
Has your employer helped other injured workers to return? Does the organisation have a policy for this?
Do I have your permission to contact your employer about this? o If yes, who is the Return to Work Co-ordinator?
4/ In a workplace, what title is given to a person that assists a worker, disabled from work-related injury, back to work
Return-to-work coordinator. If payroll > $2 mill, must have one appointed at all times
5/ In assessing a person’s ability to return to work, give examples or when it is important to take account of the side of the body upon which the injury occurred
Handedness
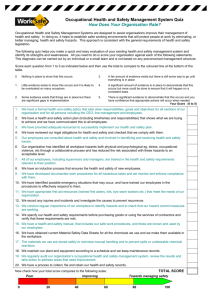
6/ What is a lost time injury?
An injury forcing an employee/contractor to remain away from his/her work beyond the day of the incident that caused the injury
Its rate: no. of injuries causing lost time for employees & contractors per million hours worked (i.e. 500 workers x 250 working days/yr x 8 hours/day= 1 mill)
Severity rate:
time (days) lost and time and days on alternative duties per million hours worked
Duration rate:
- average time (days) lost and the days on alternative duties for each LTI
7/ What statutory rules apply to pushing, pulling, lifting and lowering loads at work?
Employers must identify & control risk in hazardous manual handling: o Manual handling characterised by
Repetitive/sustained application of force
Repetitive/sustained awkward posture
Repetitive/sustained movement
Application of high force (trying to move things that are hard to move)
Exposure to sustained vibration o Manual handling of live persons/animals o Manual handling of unstable/unbalanced loads or loads that are difficult to grasp/hold
Must make every effort to: eliminate the risk or reduce as far as possible
8/ In Australian NH&MRC management plan for acute musculo-skeletal pain, what is the broad category covered by red flags? What is the broad category covered by yellow flags?
Red flags:
Alerting clinical features/risk factors: o Fractures/trauma
Cervical spine injury, osteoporosis, metabolic disease o Infection
Spinal joint, osteomyelitis, fever o Tumor o Crystal arthritis/septic arthritis o Aneurysm (aortic, vertebral) o Osteonecrosis
Yellow flags:
psychosocial & occupational factors that may influence treatment and recovery o Attitudes/beliefs about pain, behaviours, meoitions o Family o Work o Compensation issues o Diagnostic and treatment issues
Session 4
Q1: What is a confined space? What makes it dangerous?
A space with relatively narrow dimensions and poor natural ventilation
Q2: What is narcosis? Give some examples of substances that cause narcosis. What does narcosis have to do with volatility
Narcosis is a reversible physical effect on cell membranes causing light-headedness.
Narcosis is caused by vapours of volatile oil-miscible liquids- i.e. solvents such as toluene
Common effect from vapours of substances known as organic solvents used to dissolve/suspend oils, greases, glues & resins
Q3: What information is written on a material/clinical safety data sheet (MSDS/CSDS)?
How do you find out what you need to know to care for someone that has been suddenly and adversely affected by a chemical with a long name?
Includes:
identification, composition and uses
physical & other properties
health hazard info
precautions for use
safe handling info incl storage, handling, spills & disposal
Q4: When a worker has been in an intensely frightening situation, what forms of reaction can occur?
- Shock
Q5: What is mass psychogenic illness. How do you recognise it and distinguish it from organic disease?
‘The rapid spread of illness signs and symptoms for which there is no plausible organic aetiology.
Episodes are typified by an anxiety-generating precipitant within the victims’ immediate environment
Symptoms occur within close temporal proximity of exposure to the stimulus
Charcteristics o Appearance of sx with no plausible organic basis o Transient & benign Sx o Rapid onset & recovery o Occureence in a segregated gp o Extraordinary anxiety o Sx spread by line-of-sight, sound, or oral contamination o Spread often occurs down the age-scale. Starts older younger o Preponderance of females o An identifiable index case
Q6: In regard to a person with an acute illness at work, what questions assist you to find out the size of the problem, the type of substance involved, and the protective measures already in place?
What is your job?
In this job, what do you actually do?
How long have you done these things?
Did your problem come on slowly or fast?
When did your problem start?
Did anything happen at work around this time?
Do you think that something at word has made you sick? (If so, describe)
… If there was an obvious sudden problem, then follow up questions include-
What does the process make or do?
What happened?
How many people were affected?
In what way were you affected? (i.e. weeping eyes, cough)
What action was taken by those in charge?
Was there an odour?
How big was the spill? (by tank volumes etc)
If there was a dust/gas- what colour was it? Did it sting your eyes?
What equipment was damaged?
How is the substance normally used?
Do you have an information about the chemical? (label) What does it say?
Did you wear any protective clothing? If so, does it seem effective?
What first aid or other treatment has already been given?
Q7: What is a solvent?
Q8: Distinguish the terms hazard and risk
Hazard- Something with the potential for harm (qualitative)
Risk- Probability that harm will occur and the severity of that harm (quantitative)
Types of hazard- emotional, physical, biological, substance-related
Q9: What is it about the word safe that gives potential for ambiguous communication? Why can you not prove something is safe?
Safe is a subjective judgement- controversial if something is safe.
Q10: In hot work, what are two common ways for heat to be gained by a worker’s body? What are three factors that notably affect the rate of heat loss from a worker’s body?
Heat is gained by the body from the use of muscles, by radiation of heat to people’s bodies from large hot surfaces, and from high air temps.
Heat can be lost by a cool breeze, evaporation of sweat. Indoor work with frozen
Risk of Raynaud’s increased by cold temp & vibration (i.e. outdoor drilling)
Hypothermia: hallucinations, confusion, VF.
Q11: Name three different ways of getting a work-related eye injury
Corneal foreign body
Keratoconjunctivitis from sudden UV glare (welding flash)
Splash of caustic liquid
If a high speed particle was felt to hit eye, but can’t be seen, must do X-Ray to see if there’s an intraocular foreign body.
Infrared lasers are invisible and provide the most damage.
Q12: When a worker says, ‘This chemical at work has made me ill’ why should you always consider a differential diagnosis?
Q13: Increasing the dose of a substance can affect the harm that it does in two fundamental ways. What are they?
Q14: What is ‘ALARA’? Why is it not appropriate to treat workplace exposure standards in the same way that most motorists treat speed limits, i.e. to go as close to the limit as you can?
As low as reasonably achievable
Changing the dose will change the severity of effects or the probability of their occurrence- or both
Q15: By what routes are workplace substances most likely to be absorbed into a worker’s body? Give examples of types of substances that enter the body in these different ways
Inhalation or absorption through intact skin
Or ingestion- i.e. biting dirty nails
Metals, pesticides
Q16: What are two important mechanisms of severe, rapid poisoning at work?
Exposure to gases or vapours in a space with relatively narrow dimensions and poor natural ventilation (confined space)
Acute bronchoconstriction from inhalation of isocyanates to which the patient has already been sensitised
isocyanates- used to make plastic foam- also in two pot paints
Q17: What is asphyxiation? What are two important mechanisms of asphyxiation brough about by gases in workplaces?
Asphyxiation may result from simple displacement of oxygen, or because of temporary change to a metabolically active protein (CO poisoning)
Any substance with a pH away from 7.4 and many volatile aldehydes will irritate
Q18: Why are gases such as hydrogen chloride and sulphur dioxide irritating?
Low pH
Q19: Nitrogen and oxygen co-exist in air and yet in certain circumstances can chemically combine to form nitric oxide and nitrogen dioxide. What makes that happen?
From heating of air to flame temperature
Q20: Hydrogen sulphide has a very strong and recognisable odour, yet it can be dangerous in a confined space such a sewer because workers do not realise that the concentration in air is gradually increasing. What causes this deception?
Can fatally depress respiratory drive when inhaled at high concentration- because can induce olfactory adaptation/fatigue
gradually-rising concentration goes unnoticed
Odour indicates the presence of a molecule of vapour/gas, but not a reliable guide to toxicity
CO poisoning
CO binds with Hb. This displaces O2 from Hb decreased oxygen-carrying capacity of blood
Build up causes poisoning- usually from inhalation of smoke in an indoor area/of engine exhaust. Can lead to irreversible oxidative damage to cells of the brain
Can be reversed by 10 mins of inhalation of 100% oxygen
Q21: Name five well-recognised causes of occupational asthma *
Volatile isocyanates (paints, plastic foam manufacture)
Western Red Cedar (resinous softwood- joineries)
Protien or related dusts (flour in bakeries, mites in stored products)
Some components of the mix of atnisogeruc cibtanubabts ub aluminium smelters
Epoxy resin hardeners
Sulphur dioxide (preservatives in white wine/dried fruit)
Q22: What is a pesticide? What broad categories of pesticide do you know?
Refers to the use to which some substances are put-
Incecticides- insects & spiders
Rodenticides- warm-blooded pests
Herbicides- kill pest plants, mainly weeds
Insecticides capable of passing readily through intact skin body. Even higher from very vascular areas.
Organophosophorous and carbamate insecticides- inhibit cholinesterase enzyme
Q23: What are the likely symptoms and signs presented by a person poisoned with an organophosophorus insecticide? What treatment would you give?
Causes over-stimulation then paralysis (antidote- pralidoxime)
Synthetic pyrethroids- to kill insects, and glyphosate to kill weeds
Q24: Distinguish the effects of skin exposure to hydrofluoric acid from those of skin exposure to hydrochloric acid
HF acid_ colourless liquid. Used as a catalyst in petrol refining & production of compounds of fluoride
used in computer chip manufacture & etching glass & removing rust spots from cars
Substances in molecular form penetrate membranes (skin) more readily than ions
Circulating soluble calcium and magnesium ions are important for muscle & nerve function
HF disossiates far less than HCl (considered weak acid in comparison)
HF passes through the skin
fluoride ions deplete Ca & Mg by reaction with them o If more than 1% of skin comes in contact with HF and isn’t immediately rinsed off, systemic loss of Ca & Mg ionswith rise in K from damaged cells increased risk of VF o If burns with HF, need thorough washing & application of Calcium gluconate gel
HF acid causes deep burns and systemic effects whereas HCl burns from outside in and effects are mainly local
Session 5
Occ History for a problem that is gradual in onset:
What is your job?
In this job, what do you actually do?
How long have you done these things?
When did your problem start?
Did anything happen at work around this time?
Do you think that something at work has made you sick? (If so, describe)
Does your (presenting symptom) get better or worse through the day? Does anything affect it
(heat, ventilation)? Is it there at night?
Does your (presenting symptom) change on weekends or holidays?
Are any other workers affected in a similar way?
Has anything like this happened before? Was anyone else affected then?
Have there been any changes to processes, maintenance or staffing while all this has gone on?
What ventilation or protective clothing is there? Has this changed?
Has anything changed at work that has made things better or worse?
Have any workers doing different work been affected like you?
Q1: What is an occupational disease?
Q2: What is the cochlea? How does it convert incident sound into electrical impulses?
From the eardrum, vibrations are transmitted across to the inner ear/cochlea
inside inner ear, are sterociliar that convert movement elextricitical messages that are relayed along neural pathways to the brain
External hair cells are the ones that selectively amplify soft sounds but not loud sounds o Damaged after years of exposure to loud noise.
Q3: Distinguish sound intensity level and decibels from frequency & hertz
Frequency- the number of vibrations/sec. Determines the pitch of a sound.
- measured in Hertz
Intensity- the amplitude of these vibrations. More related to the ‘loudness’ of the sound.
measured in decibels
Q4: Having double the intensity of sound simply adds three decibels. Why?
Q5: On an audiogram, what is the classical appearance of noise-induced hearing loss?
Consonants are quietest. 4000-6000 Hertz
ruined in noise-induced hearing loss
Q6: What potential harm(s) can occur to a person’s hand where a vibrating drill is used in a quarry on a cold, wet, Winter morning?
Raynaud’s disease risk increases (esp smokers)
Truck drivers- if whole body vibration can low back pain
Q7: How does ‘the bends’ occur as a result of too-rapid ascent from a deep dive?
Working in preassurised air can
acute: arterial gas embolism: ‘the bends’
Chronic: aseptic necrosis of the head of long bones
Happens b/c fast ascent makes gas (nitrogen) particles that are dissolved in blood at depth form bubbles.
Rx- recompress person in a compression chamber
Q8: What are six well-recognised causes of irritant contact dermatitis?
Dermatitis: inflammation of the skin. Can be irritant (75%) or allergic (25%)
Irritants: o Destroy the intercellular lipids of the stratum corneum its dissolution o Egs:
Water, frequent hand washing
Soap, detergents, cleansers, shampoos, disinfectants
Solvents, kerosene, thinners
Oils, esp mineral oils (soluble oils can allergies
Cement
Dust, hard particles, fibreglass
Low humidity
Heat & sweat o Hairdresser in early training- mainly irritants. Later on, mainly allergens (bleach, hair dyes, perming solutions)
Q9: What are six well-recognised causes of allergic contact dermatitis?
Allergic reaction: o Type IV immunological delayed hypersensitivity o Involves penetration of chemicals into skin o Test via patch testing o Allergens:
Nickel, cobalt, chrome in cement & leather
Frangrances, essential oils, solubule oils
Preservatives, formalin, Dowicill, Germall
Rubber, epoxy resins, nailpolish, clothing dyes
Hair dressing (dye, bleach)
Medicaments, glues, plants, wood dusts (esp pine)
Disinfectants
Other cosmetic ingredients- i.e. emulsifying agents
Q10: How do you distinguish irritant contact dermatitis from allergic contact dermatitis? Why is it very important to make this distinction?
Atopy more likely to get irritant.
Usually, irritant is from extended exposure to commonplace things whereas allergic can be from a minor episode of contact
Irritant, once healed, doesn’t really matter so long as you protect against it next time
Allergic important because even minor contact in future can generate a rash which means worker mightn’t be able to continue that role.
If you suspect irritant- jobs include:
food handling, hairdressing, cleaning, health care worker
Frequent use of soap
Use of organic chemical liquids, particularly solvents
Use of acids/alkalis
Use of cement (alkaline substance)
Metal work using lathes/milling machines (GLOVE USE BAD)
Allergic jobs:
hairdressing,
cement
epoxy resins in construction
Repeated use of latex gloves (esp if powdered)
Rubber chemicals
Formaldehyde-based preservatives
Dyeing- textile manufacture
Fragrances- tea tree oil & essential oil used undiluted on skin
Use of photographic chemicals
Plant nursery
Q11: What is asbestos? What cancers are known to result from months or years of inhalation of asbestos dust?
Q12: What is mesothelioma? What is the outlook for a person with this disease?
Mesothelioma is an aggressive tumour of the serosal surfaces esp the pleura and sometimes the peritoneum & pericardium. Asbestos is the only known cause.
present with SOB, chest pain, pleural effusions
Weight loss & fatigue are late features
CT shows thick rind of tumor tumor around the pleural cavity.
From: construction/demolition, applying/removing insulation on steam pipes, manufacture/fitting of breakes/clutch facings, mining of asbestos
Q13: Why is epidemiology an ineffective tool to establish a level of exposure to asbestos below which there is no increased risk of mesothelioma?
Because it is impossible to show that minimal exposure differs in any health-related way from no exposure
Q14: How do asbestos-elated pleural plaques differ from mesothelioma?
Not all asbestos pleural pathology is mesothelioma. About half of people with prolonged exposure have a calcified thickening of the pleura.
‘pleural plaques’- incidental finding on x-ray and have no clinical consequence
but, MUST differentiate b/w the two
Q15: Apart from asbestos, name three other substances recognised to cause work-related cancer and the type of cancer they cause
Fine hardwood dust nasopharyngeal carcinoma
Benzene myeloid leukaemia
Vinyl chloride angiosarcoma of the liver
Silica human lung carcinogen
Other cancers:
SCC: skin- working outdoors
Lung cancer: smoky atmosphere, asbestos exposure, silica- work as a painter
Bladder cancer- ork with tar/pitch, work with dyes as a painter
Myeloid leukaemia- benzene, ionising radiation
Carcinoid of nasal cavity- hardwoord dust
Breast cancer- years of work involving circadian disruption (flight attendant/late shift workers)
Q16: What is meant by pneumoconiosis? Give an example
Any disease of the lung- but usually fibrosis- that results from months/years of fine, occupational dust inhalation (usually insoluble minerals)
i.e. silicosis, asbestosis, coal miners’ pneumoconiosis
Repeated inhalation of large molecular weight dusts in enclosed/semi-enclosed spaces
(bacterial/fungal proteins) can lead to chronic lung disease: hypersensitivity pneumonitis
uncommon in Aus
increasing breathlessness & mild fever
tends flocks of birds/crops like mushrooms in semi-enclosed space
Q17: A worker newly-diagnosed with mesothelioma states that he works in the control room of an oil refinery. What other items of occupational history may be relevant to est the cause of his condition?
Nanoparticles- smaller the particles, the more potential to cause inflammation, kill macrophages and
fibrosis
Session 6: Virtual Worksite Visit
Q1: In regard to machinery at work, what’s wrong with the expression, “if it ain’t broke, don’t fix it”?
Because they require maintenance
Types of prevention:
Primary: targets aetiologies/risk factors
Secondary: addresses progress
Tertiary: addresses consequences
Sensitive: reliably positive when the disease of interest is present
Specific: reliably negative when no disease is present
Q2: Where on the web do you find out about laws that apply to health in workplaces- in
Victoria, in Malaysia?
Victorian Legislation and Parliamentary Documents home page
Q3: We think it good for you to know one sentence of occupational health and safety law off by heart. It is called the employers’ general duty of care. Recite it for the jusidiction in which you are based- Victoria or Malaysia.
‘An employer must, so far as is reasonably practicable, provide and maintain for employees of the employer a working environment that is safe and without risks to health’
Workplace regulations refer commonly to the management of hazards such as hazardous substances
(and specifically asbestos and lead), noise, entry to confined spaces & manual handling.
Q4: What are HAZCHEM signs for?
2 physical hazards ever-present in workplaces: Fire & electric shock
HAZCHEM: guide firefighters to the broad qualities of chemicals stores, to any special agent required to extinguish the fire, and to the need for evacuation of nearby premises should a fire occur
their label and colour will delineate their purpose
Q5: How may the appearance of a patient who has suffered direct current electric shock differ from the appearance of a patient shocked by alternating current?
Electric shock: from AC (alternating current) causes tetany and sweating
Direct current causes electrolysis. Most tissue damage from the heat produced by the current as it passes through- can cause heat coagulation even charring.
Domestic electricity can depolarise heat & nervous tissue to the extent of causing VF
Lightning injuries (high voltage DC) cause asystole but also cause tearing of tissues due to shock wave ripple through the body
Electrocution: death caused by application of electric shock
Session 7: Your preventive role
Q1: What do the different levels of prevention address- 1, 2, 3? Why is secondary preventure better for lead exposure than asbestos dust? (see above)
Q2: Tertiary prevention can seem to be like ‘shutting the gate after the horse has bolted’. Why is it so important in occ medicine?
Esp in assessing return to work.
Q3: What is the hierarchy of control? Give examples
Algorithm of control of workplace risks:
Hazard Exposure (transmission of harm) worker
Removing the hazard:
elimination of the substance from the workplace
substituation by a less hazardous substance
Reducing the exposure:
isolation of the process to reduce number of people exposed
engineering control- local exhaust ventilation to remove contaminants
administrative control- keeping workplace clean, gentler handling of powders
Shielding the worker:
- only where other effective means of controlling the hazard aren’t practicable/insufficient should personal protective equip be used
Q4: What is local exhaust ventilation? When is it used? What is the physical reason why it must be close to the source of airborne contaminant?
2 types:
Dilution ventilation for rooms o Opening windows, air con
Local exhaust ventilation o Large vacuum cleaner- fan draws air and dust in o Draws contaminants away from individual workstation o Must be situated close to the source of contamination so can remove particles effectively.
Q5: Name some forms of personal protective equipment to protect skin & lungs
skin protection: gloves, boots, aprons, face shields
respiratory protection: gas masks, duct masks
Q6: Why do you think that a facial filtering device provides adequate protection for most dust or gas exposures but is not good enough for working in a confined space?
Because need some clean air- in confined space there is too much dust, vapour or gas & poor natural ventilation
In this case, use a special respirator that supplies clean air from outside source
‘Debits’ and ‘Credit’s of illness
Debit- what has the pt lost by having a condition at this time?
Credit- what has the pt gained by having a condition at this time?
Q7: Why do people nearly always disagree about what is safe in regard to, say, the sitting of a toxic waste facility?
Because there is disagreement about how much attenuation of exposure is related to make the probability of harm so small as to be immeasurable/unimportant
continuum of risk
Therapeutic agent vs industrial toxin- TA has a therapeutic range.
Both have a means of absorption, volume of distrubution, Phase I & II reactions & a clearance mech
Fibers are elongated particles. Their adverse effects are more related to the no of fibres than the mass of fibers.
Q8: The most common health-related finding for a worker exposed to lead is nowadays a mildly elevated blood level in a person without symptoms. Why do you think that full-blown occupational lead poisoning is now rare in Victoria?
Lead
causes internal poisoning that can cause abdo pain and/mild haemolytic anaemia
primary risk comes from inhalation of dust augmented by ingestion a/w poor personal hygiene
Carried on the RBC. Test is whole blood lead concentration corrected for haematocrit
Rarely req chelation therapy
Q9: What bodily organ is (more than any other) is likely to experience harm after years of poorly-controlled exposure to the vapour of mercury or the dust of cadmium or lead?
Renal damage.
Q10: Why are measurements made in tissues like hair or nails not appropriate to use as a guide to a person’s recent-past occ exposure to lead, mercury or arsenic?
Leads to falsely high levels because handling mercury estimates b/c handling mercury in a workplace contaminates external tissue
Q11: What guides your advice to a woman who is newly-diagnosed as pregnant in regard to substances that she uses at work?
Lead may cause cognitive defects in children. Pregnant lady shouldn’t work anywhere that will increase blood lead levels
Session 8:
Q1: What action is appropriate when a person you work with consistently: a) Makes sleazy remarks? b) Threatens violence?
Appear calm, respectful, self-controlled & confident
Put patient’s statements into your own words, check to see you’ve understood
Be clear, avoid jargon
Maintain physical space, avoid too much eye contact
Include some silence
Portray your actions as being in his/her best interests
Encourage the aggressive to address the issue by seeking as many options as he/she can think for the problem
Q2: What precautions are prudent when you identify a worker that pays obsessive attention to work?
Not to overload them with work as anxiety will build and may become so severe that the worker suddenly withdraws from work
Q3: What principles apply when you seek to explain to a patient a difficult concept such as ionising radiation?
Ionising radiation has enough energy to bring chemical change to tiny particles in its path as it passes through. This can cause chemical changes to cells that decreased apoptosis etc
- Ionising radiation: gamma rays, x-rays and high energy UV rays (UVB & UVC)
- Non-ionising radiation: lower-energy UV, visible light from violet to red, infra-red, radio-frequency
Ionising radiation includes atomic particles- i.e. alpha particles. These can be very damaging if brought into intimate contact with internal body tissue
•You should realise first that not all babies are born in perfect health – about 5% have some blemish such as a large brown spot on the skin; about 1 in 200 have a health problem serious enough to require early surgical intervention such as a ‘leaky’ heart, a spina bifida or a constricted gut.
•Where pregnant women have unfortunately had massive exposure to ionising radiation, such as with large-scale accidents, even warfare, then the risk (probability) of serious harm to their developing babies is increased.
•Although the general principle with ionising radiation is to keep exposure as low as reasonably achievable, there are levels below which the risk of harm is too small to be measurable, i.e. where the risk is regarded as negligible.
•The radiation physicist calculated the dose that you very likely received. He/she took account of the energy of the rays and the way that you handled the samples. He/she considers that the risk that harm will occur to your developing baby is within the range that radiation experts would generally call negligible. The dose received by your baby would have to be tens of times higher before we would consider you to be at measurable risk.
•Radiation is energy in transit from one location to another. Some radiation, called ionising radiation, has enough energy to bring a chemical change to the tiny particles in its path as it passes through.
•All our bodies are made of millions and millions of cells. Probably most cells simply reverse any change that the radiation has wrought. Others don’t; then, the chemical change within the cell may cause it to behave differently, even to die.
•In a developing baby, there are relatively few cells compared with someone that is full-grown, and these cells are very active. Changing what some cells do can be harmful.
Q4: A salesman tells you that he has a new blood test that is diagnostic for ‘sick building syndrome’. Why is this claim likely to be false?
Syndrome: a cluster of signs & symptoms arising from a common pathology
term can be used when there is a clear disease entity whose mechanism of devt is veiled
Some syndromes aren’t medical ones- link may social rather than science-based
In order for a test to be diagnostic, it must be highly specific, i.e. it shows positive for only a very small proportion of people without the disease. (The test should also reasonably recognise people with the disease, i.e. have adequate sensitivity.) So-called ‘sick building syndrome’ has a constellation of clinical manifestations, i.e. it has fuzzy boundaries, its boundaries fade off into shadows. When a disease is ill-defined, then no test that can ever reliably exclude people without the disease – if you can’t really tell what’s in, then you can’t really tell what’s out!
Q5: When a worker says, ‘This chemical at work has made me ill?’ why should you always consider a differential diagnosis?
The worker may have reached that conclusion because the occurrence of the exposure and symptoms were closely related in time (days or weeks) or because a particular hazard has a fearful reputation. Their conclusion may indeed be correct. However, Hazardous Substances Regulations have brought much control to the use of substances, so in any one individual doctor’s practice, the appearance of a person adversely affected by a substance at work will not occur commonly. An important principle of diagnosis is to always consider relevant common conditions or serious pathologies in a differential diagnosis. Never just assume that just because some substance has a long, weird name that it is necessarily the culprit. It may be; it may not.
Q6: Distinguish the qualities of a diagnosis that makes it useful for a medical purpose from the qualities of a diagnosis that makes it useful for a social purpose.
Medical purpose:
In a word, specificity.
•It refers to the bodily part or system that is affected.
•It refers to the pathological process occurring there.
•It offers a starting point to present evidence-based options for treatment.
Social purpose:
•It is inclusive; it captures everyone that seeks membership of this group.
•It has enough community acceptance to foster development of a support organisation, funding of research, rights of affected people including, perhaps, compensation.
•Its essence can be articulated well enough for a media ‘grab’.
Q7: How do you tell whether a patient’s illness is likely to be work-related?
Ask self questions like-
What state of mind did the pt have at the time? i.e. dazed, terrified?
What knowledge had he/she for comparison?
How much time has elapsed between the alleged causal exposure & time of report?
Is I likely that what is offered as facts is selectively amplified/not presented in full?
If likelihood ratio <1.5, very unlikely. LR: is it related/it isn’t related.
Q8: Who practises occupational medicine?
Occupational medicine has two major emphases:
•knowledge of causes of injury and disease which leads to preventive effort, and
•assessment of a person's capacity for work.
Knowledge of causation is used in two main ways – prevention and compensation. Government social policy usually makes the criteria of causation that are used for compensation wider than the criteria used to prioritise investment in prevention.
Occ Medicine:
•Any clinician
•Nurses often assist with screening work
•A specialty in RACP. About 330 Fellows across Australia and New Zealand.
Occ Health:
•Doctors, nurses
•Occupational hygienists – assess exposure
•Ergonomists – assess design of workstations and processes
•Risk engineers – assess equipment/plant, potential liability
Q10: What type of disease and exposure could you be asked about in an OSCE or written exam?