Informed Consent: Process, Documentation, Alteration and Waivers
advertisement

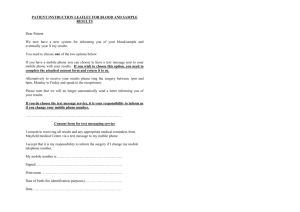
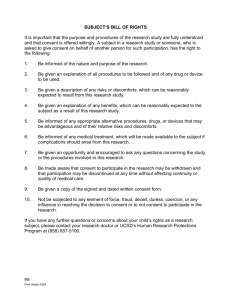
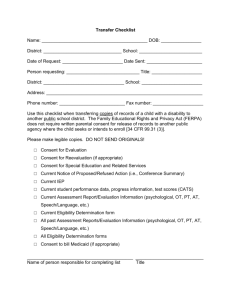
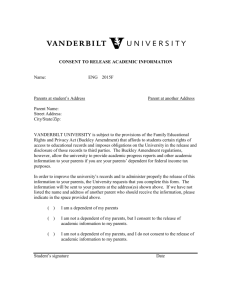
INFORMED CONSENT: PROCESS, DOCUMENTATION, ALTERATION AND WAIVERS Suzanne Sparrow Objectives Significance & History Regulations (DHHS/FDA) Elements of Consent Waiving/altering consent Waiving documentation of consent Process of consent Consent for Non-English speaking participants/ English speaking participants with low literacy Document Management/Tips Why is consent important? Nazi War Crimes (1940’s) Freezing Tuskegee (1932-1972) Withheld information/treatment Belmont Report (1979) Respect experiments, sea water experiments for Persons, Beneficence and Justice Havasupai Indian Tribe/Arizona State University (1990-1992) Use of samples not specified in informed consent. What regulations must be adhered to regarding informed consent? Studies subject to DHHS requirements (45 CFR 46.116) Obtain the legally effective informed consent of the subject or the subject's legally authorized representative prior to involvement in research. Provide the prospective subject or the representative sufficient opportunity to consider whether or not to participate and minimize the possibility of coercion or undue influence. Information shall be in language understandable to the subject or the representative. No informed consent, whether oral or written, may include any exculpatory language. contain the information required by each of the eight basic elements of 45 CFR 46.116(a), and each of the six elements of 45 CFR 46.116(b) that is appropriate to the study. What regulations must be adhered to regarding informed consent (cont.)? Studies subject to FDA requirements (21 CFR 50.20) Almost identical requirements as DHHS except the confidentiality statement for FDA trials must include a statement that the FDA may inspect research records Provisions for altering or waiving consent within DHHS regulations but not FDA Provisions for waiving documentation of consent found in both DHHS and FDA regulations with only slight differences FDA requires a specific statement if a clinical trial--21 CFR 50.25(c) 8 Essential Elements of Consent (1) A statement that the study involves research, an explanation of the purposes of the research and the expected duration of the subject's participation, a description of the procedures to be followed, and identification of any procedures which are experimental. (2) A description of any reasonably foreseeable risks or discomforts to the subject. (3) A description of any benefits to the subject or to others which may reasonably be expected from the research. (4) A disclosure of appropriate alternative procedures or courses of treatment, if any, that might be advantageous to the subject. (5) A statement describing the extent, if any, to which confidentiality of records identifying the subject will be maintained [and that notes the possibility that the FDA may inspect the records]. (6) For research involving more than minimal risk, an explanation as to whether any compensation and an explanation as to whether any medical treatments are available if injury occurs and, if so, what they consist of, or where further information may be obtained. (7) An explanation of whom to contact for answers to pertinent questions about the research and research subjects' rights, and whom to contact in the event of a research-related injury to the subject. (8) A statement that participation is voluntary, that refusal to participate will involve no penalty or loss of benefits to which the subject is otherwise entitled, and that the subject may discontinue participation at any time without penalty or loss of benefits to which the subject is otherwise entitled. 6 Additional Elements of Consent (1) A statement that the particular treatment or procedure may involve risks to the subject (or to the embryo or fetus, if the subject is or may become pregnant) which are currently unforeseeable. (2) Anticipated circumstances under which the subject's participation may be terminated by the investigator without regard to the subject's consent. (3) Any additional costs to the subject that may result from participation in the research. (4) The consequences of a subject's decision to withdraw from the research and procedures for orderly termination of participation by the subject. (5) A statement that significant new findings developed during the course of the research which may relate to the subject's willingness to continue participation will be provided to the subject. (6) The approximate number of subjects involved in the study. Consent Element for Clinical Trials When seeking informed consent for applicable clinical trials, the following statement shall be provided to each clinical trial subject in informed consent documents and processes. This will notify the clinical trial subject that clinical trial information has been or will be submitted for inclusion in the clinical trial registry databank. The statement is: "A description of this clinical trial will be available on http://www.ClinicalTrials.gov, as required by U.S. Law. This Web site will not include information that can identify you. At most, the Web site will include a summary of the results. You can search this Web site at any time." Waiving/Altering Consent (only for nonFDA regulated research) An IRB may approve a consent procedure which does not include, or which alters, some or all of the elements of informed consent, or waive the requirements to obtain informed consent provided the IRB finds and documents that: (1) The research involves no more than minimal risk to the subjects; (2) The waiver or alteration will not adversely affect the rights and welfare of the subjects; (3) The research could not practicably be carried out without the waiver or alteration; and (4) Whenever appropriate, the subjects will be provided with additional pertinent information after participation. Waiving Documentation of Consent An IRB may waive the requirement for the investigator to obtain a signed consent form for some or all subjects if it finds either: (1) That the only record linking the subject and the research would be the consent document and the principal risk would be potential harm resulting from a breach of confidentiality. Each subject will be asked whether the subject wants documentation linking the subject with the research, and the subject's wishes will govern (not found in FDA regulations); or (2) That the research presents no more than minimal risk of harm to subjects and involves no procedures for which written consent is normally required outside of the research context. In cases in which the documentation requirement is waived, the IRB may require the investigator to provide subjects with a written statement regarding the research. Consent Process Informed consent is more than just a signature on a form, it is a process of information exchange—not a means to an end. Institutional Review Boards (IRBs), clinical investigators, and research sponsors all share responsibility for ensuring that the informed consent process is adequate. The investigator is responsible for ensuring that informed consent is obtained from each research subject before that subject participates in the research study. While the investigator is not required to personally conduct the consent interview, the investigator remains ultimately responsible, even when delegating this task. In addition to signing the consent, the subject/representative should enter the date of signature on the consent document, to verify that consent was actually obtained before the subject began participation in the study. If consent is obtained the same day that the subject's involvement in the study begins, the subject's research record should document that consent was obtained prior to participation in the research (time). A copy of the consent document must be provided to the subject and the original signed consent document should be retained in the study records. The IRB should be aware of who will conduct the consent interview. Those conducting consent procedures should be adequately trained. The consent process begins when a potential research participant is initially contacted. Although an investigator may not recruit subjects to participate in a research study before the IRB reviews and approves the study, an investigator may determine if an adequate number of potentially eligible subjects is available. Non-English Speaking Participants When the study subject population includes non-English speaking people or the clinical investigator or the IRB anticipates that the consent interviews will be conducted in a language other than English, the IRB requires a translated consent document to be submitted. As required by both the FDA and DHHS regulations, a copy of the consent document must be given to each subject. In the case of nonEnglish speaking subjects, this would be the translated document. While a translator may be helpful in facilitating conversation with a non-English speaking subject, this should not be substituted for a written translation. If a non-English speaking subject is unexpectedly encountered, investigators will not have a written translation of the consent document and must rely on oral translation. If investigators enroll subjects without an IRB approved written translation, a "short form" written consent document, in a language the subject understands, should be used to document that the elements of informed consent were presented orally. The required signatures on a short form are stated in 21 CFR 50.27(b)(2) and 45CFR46.117(b)(2). Investigators should carefully consider the ethical/legal ramifications of enrolling subjects when a language barrier exists. If the subject does not clearly understand the information presented, the subject's consent will not truly be informed and may not be legally effective. ECU UMCIRB allows the short form to be used only once per study before expecting a fully translated consent to be submitted. English Speaking Subjects with Low Literacy A person who speaks and understands English, but does not read and write, can be enrolled in a study by "making their mark" on the consent document, when consistent with applicable state law. A person who can understand and comprehend spoken English, but is physically unable to talk or write, can be entered into a study if they are competent and able to indicate approval or disapproval by other means. If (1) the person retains the ability to understand the concepts of the study and evaluate the risk and benefit of being in the study when it is explained verbally (still competent) and (2) is able to indicate approval or disapproval to study entry, they may be entered into the study. The consent form should document the method used for communication with the prospective subject and the specific means by which they communicated agreement to participate in the study. An impartial third party should witness the entire consent process and sign the consent document. Video tape recording of the consent interview is recommended. http://www.fda.gov/RegulatoryInformation/Guidances/ucm126431.htm Minor Assent Assent means a child's affirmative agreement to participate in a clinical investigation. Mere failure to object should not, absent affirmative agreement, be construed as assent. In determining if children are capable of giving meaningful assent, the IRB will take into account the ages, maturity, and psychological state of the children, either individually or as a group, as it deems appropriate. The PI, in consultation with the UMCIRB, will decide if the protocol requires an assent document for the child in addition to a permission form for the parents or guardian. The decision will be based primarily on the expected level of comprehension of the proposed research participants. At ECU, unless otherwise determined by the IRB, documented assent is required for children 12 to 17 years of age. Children 7 to 11 years of age should be given the opportunity to give verbal assent, with the script to be used in these situations submitted for IRB review and approval. This verbal assent should be documented in the research record or on the parental permission form. For children under the age of 7 years, the research should be explained to the extent of the child’s understanding but no documentation is required. Parent/Guardian Signatures for Minor Assent Investigators must consider the number of parental signatures required according to 45 CFR 46 Subpart D and 21 CFR 50 Subpart D as follows: Research that does not involve more than minimal risk. Requires one parent’s signature. Research involving more than minimal risk but presents the prospect of direct benefit to the individual participants. Requires one parent’s signature. Research involving more than minimal risk and no prospect of direct benefit to individual participants, but likely to yield generalizable knowledge about the participant's disorder or condition. Requires both parents’ signatures, unless one parent is deceased, unknown, incompetent, or not reasonably available, or when only one parent has legal responsibility for the care and custody of the child. Research not otherwise approvable which presents an opportunity to understand, prevent, or alleviate a serious problem affecting the health or welfare of children. Requires both parents’ signatures, unless one parent is deceased, unknown, incompetent, or not reasonably available, or when only one parent has legal responsibility for the care and custody of the child. Document Management Ensure correct consent document is being utilized by those performing consent (check date stamps). Include new version number or date when making an Amendment to the consent. Track and document re-consent when necessary. Verify necessary signatures, initials and date. Tips Read the consent through in its entirety before submitting for approval. Lay language. Run spell check and investigate grammar issues (Microsoft Word can do this for you). Charts and tables. Send consents to potential participants ahead of time. Document consent conversation. Consent: Example http://www.carilionclinic.org/Carilion/Informed+Co nsent Questions/Comments?