Medicolegal and Ethical Aspects of Prehospital Emergency
advertisement

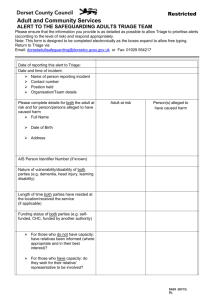
MEDICOLEGAL AND ETHICAL ASPECTS OF PREHOSPITAL EMERGENCY MEDICINE IN INTERNATIONAL CONTEXT Craig M. Klugman, Ph.D. UT Health Science Center San Antonio . . Jennifer Bard, JD, MPH Texas Tech School of Law CASE • You are a health care professional heading out on a well deserved holiday overseas. On your 10 hour flight, a flight attendant makes an announcement asking for anyone who may be a doctor to press the call button. As you are flying over international waters, there is no possibility for other outside assistance for many hours. • Are you ethically obligated to assist while on holiday? • Are you legally obligated to assist while on holiday? • Answer might be clearer in a single nation setting, but internationally, the answer becomes much more complicated. PRE-HOSPITAL VS. CLINICAL SETTING Pre-Hospital • You often go to patient (or patient is brought to ED) • Care occurs in ED, the field, long-term care facility Clinical • Patient comes to you • Care occurs in hospital, clinic, or office • Greater likelihood of patient capacity • Physician can choose patients; patients can choose physicians • Greater likelihood that provider is a physician • Patient more likely to lack capacity • Neither patient nor provider able to choose • Provider more likely to be non-physician (EMT, paramedic) • Patient more likely to be in emergent situation • Greater likelihood that some time is available for deliberation • Safety applies both to providers (first) and patients in terms of avoiding or dealing with existent physical harms • Safety usually refers to patients in terms of preventing harm LEGAL FRAMEWORK • Must know the laws of the jurisdiction in which one practices • Applicable Legal Areas • (1) Criminal Law • (2) Licenses • (3) Negligence ETHICAL FRAMEWORK Assist in the process of ethical decision-making by providing guidance in moral deliberation as to what questions to ask and what ideas are most important in a specific case. • (1) Safety or preventing harm to yourself or others; • (2) Virtue or goodness and excellence of character; • (3) Dignity or caring for all individuals with respect and • (4) Fairness or treating all people fairly and justly. SAFETY Preventing and limiting harm to oneself and others • What actions could minimize morbidity and mortality? • Does a proposed course of action keep you safe from harm? • Does a proposed course of action go outside accepted bounds of security? • Have you taken all safety precautions? • Has the patient’s privacy been respected and protected? • What actions will help protect your patient from harm? • Have you checked in with your partners? • Have you checked in with your chain of command? VIRTUE Goodness; excellence; character necessary for one to perform his/her duties • What is your desired outcome for this patient in this situation? • What are your options to lead to the desired outcome? • What option is most likely to be successful? • Does the choice or option fall within your scope of practice? • Do you have the skill or competency needed in this case? • If you do not, have you received instructions from medical command or the senior medical officer as to how to proceed? • Have you thoroughly documented the case and your actions? DIGNITY Treat all individuals with respect • Have you treated your patient as a as you would want to be treated? • Do your proposed choices acknowledge the individual human rights of all people? • Have you met the physical and emotional needs of the patient? • Does the patient have status and ability to make decisions? • If yes, did you request the patient’s consent? • If no, is someone with the legal authority to make a decision identified and available? • Is the patient at risk of death or serious harm if immediate action is not taken? FAIRNESS To treat all people justly and equally. To distribute scarce resources in a just manner • Have all patients been treated equally as human beings and not discriminated against by age, sex, race, religion, socioeconomic status, or other arbitrary category? • Have all co-workers been treated equally according to their ability and skill training? • Have you applied triage without bias, if necessary? • Have you followed all rules, laws, and policies? • Have you acted in good faith? DISCLOSURE • You are a the scene of a motor vehicle accident. A couple has been struck by a drunk driver. The driver of the struck vehicle, a female is in serious condition and the passenger, a male, has gone through the window and is dead. The female tells you that she is fine and that you should spend your time working on her husband. She demands that you treat him first? • Do you tell her that her husband is dead? STATUS/ABILITY Status (Competency) Ability (Capacity) The assumption that all adults can make their own health care decisions Competency is assumed if a person is over the age of majority or is an emancipated minor. Competency is not all or nothing, but can be gradated. o In some areas, being pregnant or giving birth may give some level of competency such as making decisions regarding the pregnancy or the child. o Minors may also have rights to consent to reproductive services, alcohol, and drug abuse treatment. A health care provider’s determination that a person is able to make a specific decision at a particular time. Ability to understand questions asked of care provider Ability to understand implications of decisions made May not be possible in cases of intoxication, drug ingestion, serious injury, or mental incompetence MASS CASUALTY • One ambulance arrives at the scene of the accident and it can only accommodate one person. Who should be transported first? The drunk driver? The injured driver of the other car? The deceased passenger? Triage Systems for sorting patients to prioritize care and ration resources. Primary Triage is performed in the field by emergency pre-hospital personnel. This sorting consists of determining a patient’s needs and applying appropriate treatments. Secondary Triage is performed by emergency physicians at the hospital. Patients are sorted to take care of the most pressing medical needs first to stabilize the patient. Tertiary Triage is performed when available resources are insufficient to meet necessary demand. There are several different types of tertiary triage that may be used depending on the situation. For example: Triage Situations Military Goal is to return soldiers to the battlefield as quickly as possible. This system may suggest helping the least injured first. Depending on supply lines, rationing of resources may or may not be necessary. Incident In multiple casualty accidents the goal is to evacuate and treat patients as quickly as possible. Resources are usually available and thus rationing is not necessary, allowing most patients to receive necessary treatment. Disaster In a mass casualty situation, resources are quickly overwhelmed. Goal is to sort patients to provide greatest care to those who can immediately benefit. Egalitarian 1. First come, first served: Whomever you see first or who comes to you first gets care first OR 2. Lottery: Everyone gets a number and you treat the winning numbers. Need Those who have are the sickest should receive available resources first. Triage Frameworks Utilitarian 1. Patients with minor injuries who will survive with minimal care. Treat last. 2. Patients with injuries who will likely survive with delayed care 3. Patients with injuries that require immediate care and have a high chance of survival. Treat first. 4. Patients who are unlikely to survive. Make comfortable and do not treat. PROMISES • The drunken driver of the car is an MP and has requested that you do not disclose his indiscretion (you did vote for him). However, a police officer has requested that you take a blood draw (she did not vote for him). What do you do? • This case has two main issues: confidentiality and the blood draw request. DUTY TO TREAT – FLIGHT SITUATION • You are a physician heading out on a well deserved holiday overseas. On your 10 hour flight, a flight attendant makes an announcement asking for anyone who may be a doctor to press the call button. As you are flying over international waters, there is no possibility for other outside assistance for many hours. CASE • Ethically, you may have a professional obligation to assist if you have the proper training, ability, capacity (i.e. haven’t been enjoying the cocktails), and act safely (yours and the patients). • A legal duty depends on (a) point of origin and destination, (b) altitude of the plane, (C) nation over which you are flying, if any. • If the plane, was instead a boat in international waters, than International Admiralty and Maritime law requires FOR MORE INFORMATION • Klugman CM & Bard J (2012). Medicolegal & ethical aspects of prehospital emergency medicine. In Boylan M (ed) The ABC of Prehospital Emergency Medicine. London: Blackwell. • Gillespie CB. 1978. “EMT Oath & Code of Ethics.” National Association of Emergency Medical Technicians (NAEMT) http://www.naemt.org/about_us/emtoath.aspx • Klugman CM 2007. “Why EMS Needs Its Own Ethics” EMS Magazine 35 (10): 114-122. • Larkin GL & Fowler RL 2002. “Essential ethics for EMS: cardinal virtues and core principles” Emergency Medical Clinics of North America 20: 887-911. • Touchstone M (2010). “Professional Development: Parts 1-5” EMS Magazine JanuaryMay http://www.emsresponder.com/publication/bio.jsp?id=366&pubId=1