CMS-1500 Billing
HP Provider Relations
October 2011
Agenda
– Objectives
– Enhanced Code Auditing
– Consent Form, Sterilization,
and Partial Sterilization
– Clear Claim Connection
– Prior Authorization
– Upcoming changes –
International Classification of
Diseases, 10th Revision,
Clinical Modification (ICD-10
CM)
– Code Sets
– CMS-1500
– Questions
– Claim Form Billing
Guidelines - Various
Specialties
2
CMS-1500 Billing
October 2011
– Fee Schedule
– Common Denials
– Helpful Tools
Objectives
Following this session, providers will be able to:
– Identify their provider classification
– Bill claims correctly for various specialties
– Understand the sterilization consent completion
– Have more information about prior authorization
– Identify the various provider code sets
– Find and understand how the fee schedule can assist
providers
– Know the common denial causes and resolutions
3
CMS-1500 Billing
October 2011
Learn
Enhanced Code Auditing
Enhanced Code Auditing
Why is the IHCP implementing the enhanced code auditing?
– The Indiana Health Coverage
Programs (IHCP) is implementing
enhanced code auditing into the
claims processing to support the
Office of Medicaid Policy and
Planning’s (OMPP’s) effort to promote
and enforce correct coding efforts for
more appropriate and accurate
program reimbursement
5
CMS-1500 Billing
October 2011
Enhanced Code Auditing
What supporting information is used for the new code auditing rules?
– Code auditing rules that have
been implemented represent
correct coding methodologies and
other coding methods based upon
general guidance from the Centers
for Medicare & Medicaid Services
(CMS), the American Medical
Association (AMA), specialty
society guidance, industry
standard coding, and prevailing
clinical practice
6
CMS-1500 Billing
October 2011
Enhanced Code Auditing
Multiple component billing
What is it?
– Identifies claims containing two or more procedure codes used to
report individual components of a service when a single, more
comprehensive procedure code exists that more accurately represents
the service performed
•
7
Individual unbundled procedures will be denied
CMS-1500 Billing
October 2011
Enhanced Code Auditing
Multiple component billing – Laboratory BT201102
– Effective for claims received on or after April 1, 2011
– Identifies when individual components of a bundled service are billed
separately rather than using the comprehensive Current Procedural
Terminology (CPT®) code
– Unbundled code line items will be denied:
• Edit
4186
Service denied. This is a component of a more comprehensive service. This service
is reimbursed under a distinct comprehensive code
Healthcare services should be reported with the procedure code that
most comprehensively describes the services performed
CPT is copyright 2010 American Medical Association. All rights reserved. CPT® is a registered trademark of
the American Medical Association.
8
CMS-1500 Billing
October 2011
Enhanced Code Auditing
Multiple component billing – Example of lab panel rebundling
Line
Date of
Number Service
To Date of Procedure Description
Service
Code
Billed
Component
Amount Rebundling EOB
01
4/1/2011
4/1/2011
82040
Albumin; serum, plasma
or whole blood
$100
Detail is denied with
EOB 4186
02
4/1/2011
4/1/2011
82247
Bilirubin; total
$100
03
4/1/2011
4/1/2011
82248
Bilirubin; total direct
$100
04
4/1/2011
4/1/2011
84075
Phosphatase, alkaline
$100
05
4/1/2011
4/1/2011
84155
Protein, total, except by
refractometry; serum,
plasma or whole blood
$100
Detail is denied
EOB 4186
Detail is denied
EOB 4186
Detail is denied
EOB 4186
Detail is denied
EOB 4186
06
4/1/2011
4/1/2011
84450
Transferase; aspartate
amino (AST) (SGOT)
$100
Detail is denied with
EOB 4186
07
4/1/2011
4/1/2011
84460
Transferase; alanine
amino (ALT) (SGPT)
$100
Detail is denied with
EOB 4186
9
CMS-1500 Billing
October 2011
with
with
with
with
Enhanced Code Auditing
Changes to code auditing methodologies – BT201135
Effective for date of service
(DOS) on or after July 15, 2011,
the IHCP began applying code
auditing of the following:
– CMS-1500 claims that are
billed with multiple units of the
same laboratory code on the
same date of service
Edit 4189 - Multiple units of the
same laboratory service are not
payable for the same date of
service, same member, and same
or different provider without
medical necessity
10
CMS-1500 Billing
October 2011
Enhanced Code Auditing
Changes to code auditing methodologies – BT201135
– CPT add-on codes reported without reporting a corresponding primary
procedure/service
•
Edit 4190 – Add-on codes are performed in addition to the primary service or
procedure and must never be reported as a stand-alone code
– Reporting multiple units of a primary service when add-on codes
should be used
•
11
Edit 4191 – A primary service or procedure code is limited to one unit per date of
service
CMS-1500 Billing
October 2011
Enhanced Code Auditing
Changes to code auditing methodologies – BT201135
Effective for DOS on or after August 1,
2011, the system began applying code
auditing of the following:
– Non-anesthesia services submitted by
an anesthesia provider specialty where
the service billed is not normally
performed by an anesthesia provider
specialty
•
12
Edit 4192 – Non-anesthesia services are not
reimbursable for the anesthesiology provider
specialty billed
CMS-1500 Billing
October 2011
Enhanced Code Auditing
Changes to code auditing methodologies – BT201135
– Non-anesthesia services submitted by an anesthesia provider
specialty where there is a more appropriate anesthesia code that
should be used for billing
•
Edit 4193 – Non-anesthesia services are not reimbursable for the anesthesiology
provider specialty billed.
•
Claim lines containing non-anesthesia services submitted by an anesthesiology
provider specialty will be denied. Providers may resubmit the denied details with the
anesthesia code(s) as appropriate.
– These anesthesia-related code auditing rules apply only to providers
enrolled with the anesthesia specialty
•
13
Multiple specialty providers will not be subjected to this type of code auditing
CMS-1500 Billing
October 2011
Enhanced Code Auditing
Changes to code auditing methodologies – BT201135
Effective for dates of service on or after August 31, 2011, the
following code audits were implemented:
– Evaluation and management (E/M) codes billed on the same
date of service as a procedure with a global period
• Edit 4194 – Identifies procedure codes billed by the same provider on the same
date of service as a code with a global period
– E/M codes billed within the pre-operative period
• Edit 4196 – Identifies procedure codes billed by the same provider within a
procedure's preoperative period
Note: E/M services performed in a postoperative period that
are unrelated to a surgical procedure should only be reported
using the proper modifier
14
CMS-1500 Billing
October 2011
Enhanced Code Auditing
Billing reminders – Use of modifiers
– Modifiers may be appended to Healthcare Common Procedure
Coding System (HCPCS)/CPT codes only when clinical
circumstances justify them
– A modifier should not be appended to an HCPCS/CPT code solely
to bypass Component Rebundling auditing
•
The use of modifiers affects the accuracy of claims billing and reimbursement, and
Component Rebundling auditing
–Same procedures, performed during the same session
• Roll all the units to a single line, unless otherwise specified in medical policy
15
CMS-1500 Billing
October 2011
Announcing
Clear Claim Connection
Clear Claim Connection
– Clear Claim Connection is a web-based solution that enables
HP/OMPP to share the National Correct Coding Initiative (NCCI) claim
auditing rules with providers
– The tool is for providers to perform claim analysis prior to submitting
the claim for processing
– Providers have access to Clear Claim Connection through a link within
the Claim Submission menu option on Web interChange
•
17
Web interChange users must have access to Claim Submission to use Clear Claim
Connection
CMS-1500 Billing
October 2011
Clear Claim Connection
18
CMS-1500 Billing
October 2011
Clear Claim Connection
Enter NPI or LPI
19
CMS-1500 Billing
October 2011
20
CMS-1500 Billing
October 2011
Click “Disallow” or “Review”
to obtain clinical edit
clarification
21
CMS-1500 Billing
October 2011
22
CMS-1500 Billing
October 2011
Clear Claim Connection – Overview
– Select the Clear Claim Connection link under the Code Auditing
menu
– Choose appropriate National Provider Identifier (NPI) if it is not
currently populated
– Click Continue button and click Agree on the Terms and Agreement
page to access the Clear Claim Connection
– Enter claim detail information to determine how the claim will process
according to the auditing rules set up in ClaimsXten McKesson
– Click Review Claim Audit Results to view the results
– Click New Claim to input information for another claim
– Click Current Claim to change the information on the current scenario
and continue with claim analysis
23
CMS-1500 Billing
October 2011
Discuss
HP ICD-10 Compliance Project Status
Details
– Professional diagnosis codes will increase to 12 entries per
transaction .
– Diagnoses fields will increase from 5 characters to 7.
– ICD-9 procedure fields will increase from 4 characters to 7
alphanumeric characters for ICD-10 .
– Diagnosis code pointer (professional claims) will expand from 4
positions to 8 (4, 2-character fields).
– The ICD version qualifier will be required on paper, Web, or EDI claim
submissions to indicate the version of ICD codes being used.
– Claims submitted with both ICD-9 and ICD-10 listed will be rejected.
– Date of service (DOS) will aid in determining if ICD-9 or ICD-10 is
used when billing your claims to the IHCP.
25
CMS-1500 Billing
October 2011
FAQs
– What is the current implementation time frame?
HP has completed the assessment for the Medicaid Management
Information System (MMIS) and is on target for the October 1, 2013,
implementation of the ICD-10 Compliance Project.
– Is there going to be a system freeze? If so, when?
Yes, there will be a system freeze. Currently, it is scheduled for
September 2013.
– Will there be vendor testing? When?
Yes, there will be vendor testing that will include managed care entities
(MCEs). Vendor testing is scheduled to begin January 1, 2013.
– Will providers/vendors be able to use the ICD-9 codes after the
October 1, 2013, implementation?
No, you must use ICD-10 codes for DOS or DOD on or after the October
1, 2013, implementation date. There is no grace period.
26
CMS-1500 Billing
October 2011
ICD-10 IHCP Provider Readiness Survey
– The first IHCP Provider Readiness Survey is in development
• A link
to the survey will be posted on the Indiana Medicaid Web site Provider
page
– The survey will be available from November 7 to November 14
– Upcoming Bulletins, Banner Pages, and Newsletters will include
information about accessing the survey
– This survey should be completed by the individual that is instrumental
in planning, implementing, and managing the transition to ICD-10 in
the provider’s business
– Survey results will help us help you, by tracking your progress and
capturing your issues
27
CMS-1500 Billing
October 2011
Learn
1500 Claims
Types of 1500 Claims
– 837P – Electronic transaction
•
Companion Guide available on IHCP Web
site: provider.indianamedicaid.com
– Web interChange
– Paper claim
– Replacement/Adjustment request
(for a previously paid claim)
29
CMS-1500 Billing
October 2011
Web interChange – 1500 Electronic filing
30
CMS-1500 Billing
October 2011
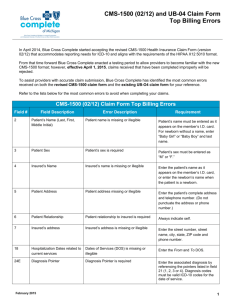
Paper Claim Form Locators – CMS-1500
31
CMS-1500 Billing
October 2011
Paper Claim Form Locators
CMS-1500
Fields
Description
1
INSURANCE CARRIER SELECTION – Enter X for Traditional Medicaid. Required.
1a
INSURED’S I.D. NUMBER (FOR PROGRAM IN ITEM 1) – Enter the IHCP member
identification number (RID). Must be 12 digits. Required.
2
PATIENT’S NAME (Last Name, First Name, Middle Initial) – Provide the member’s last
name, first name, and middle initial obtained from the Automated Voice Response (AVR)
system, electronic claim submission (ECS), Omni, or Web interChange verification.
Required.
OTHER INSURED’S NAME (Last Name, First Name, Middle Initial) – If other insurance
is available, and the policyholder is other than the member shown in fields 1a and 2,
enter the policyholder’s name. Required, if applicable.
OTHER INSURED’S POLICY OR GROUP NUMBER – If other insurance is available,
and the policyholder is other than the member noted in fields 1a and 2, enter the
policyholder’s policy and group number. Required, if applicable.
9
9a
EMPLOYER’S NAME OR SCHOOL NAME – If other insurance is available, and the
policyholder is other than the member shown in fields 1a and 2, enter the requested
policyholder information. Required, if applicable.
9c
32
CMS-1500 Billing
October 2011
Paper Claim Form Locators
CMS-1500
Fields
Description
9d
INSURANCE PLAN NAME OR PROGRAM NAME – If other insurance is available, and
the policyholder is other than the member shown in field 1a and 2, enter the policyholder’s
insurance plan name or program name information. Required, if applicable.
IS PATIENT’S CONDITION RELATED TO – Enter X in the appropriate box in each of the
three categories. This information is needed for follow-up third-party recovery actions.
Required, if applicable.
EMPLOYMENT (CURRENT OR PREVIOUS) – Enter X in the appropriate box. Required,
if applicable.
10
10a
10b
AUTO ACCIDENT – Enter X in the appropriate box. Required, if applicable.
PLACE (State) – Enter the two-character state code. Required, if applicable.
10c
OTHER ACCIDENT – Enter X in the appropriate box. Required, if applicable.
11
INSURED’S POLICY GROUP OR FECA NUMBER – Enter the member’s policy and
group number of the other insurance. Required, if applicable.
11a
INSURED’S DATE OF BIRTH – Enter the member’s birth date in MMDDYY format.
Required, if applicable.
SEX – Enter an X in the appropriate sex box. Required, if applicable.
33
CMS-1500 Billing
October 2011
Paper Claim Form Locators
CMS-1500
Fields
Description
11b
EMPLOYER’S NAME OR SCHOOL NAME – Enter the requested member
information. Required, if applicable.
INSURANCE PLAN NAME OR PROGRAM NAME – Enter the member’s
insurance plan name or program name. Required, if applicable.
IS THERE ANOTHER HEALTH BENEFIT PLAN? Enter X in the appropriate
box. If the response is Yes, complete fields 9a–9d. Required, if applicable.
11c
11d
14
16
17
DATE OF CURRENT ILLNESS (First symptom date) OR INJURY (Accident
date) OR PREGNANCY (LMP date) – Enter the date of the last menstrual
period (LMP) for pregnancy-related services in MMDDYY format. Required for
payment for pregnancy-related services.
DATES PATIENT UNABLE TO WORK IN CURRENT OCCUPATION – If field
10a is Yes, enter the applicable FROM and TO dates in a MMDDYY format.
Required, if applicable.
NAME OF REFERRING PROVIDER OR OTHER SOURCE – Enter the name of
the referring physician. Required, if applicable. For waiver-related services,
enter the provider name of the case manager. Required for Care Select PMP
for dates of service prior to January 1, 2011.
Note: The term referring provider includes those physicians primarily responsible
for the authorization of treatment for lock-in or Right Choices Program
members.
34
CMS-1500 Billing
October 2011
Paper Claim Form Locators
CMS-1500
Fields
Description
18
HOSPITALIZATION DATES RELATED TO CURRENT SERVICES – Enter the
requested FROM and TO dates in MMDDYY format. Required, if applicable.
19
RESERVED FOR LOCAL USE – Enter the Care Select primary medical provider (PMP)
two-digit alphanumeric certification code. Required for Care Select members when
the physician rendering care is not the PMP or a physician in the PMP’s group or
a clinic for dates of service prior to January 1, 2011.
21.1 to
21.4.
MEDICAID RESUBMISSION CODE, ORIGINAL REF. NO. – Applicable for Medicare
Part B crossover claims only. For crossover claims, the combined total of the Medicare
coinsurance, deductible, and psych reduction must be reported on the left side of field
22 under the heading Code. The Medicare paid amount (actual dollars received from
Medicare) must be submitted in field 22 on the right side under the heading Original Ref
No. Required, if applicable.
22
35
Note: Report the PMP qualifier and ID number in 17a.
DIAGNOSIS OR NATURE OF ILLNESS OR INJURY – Complete fields 21.1, 21.2,
21.3, and/or 21.4 to field 24E by detail line. Enter the ICD-9-CM diagnosis codes in
priority order. A total of four codes can be entered. At least one diagnosis code is
required for all claims except those for waiver, transportation, and medical equipment
and supply services. Required.
CMS-1500 Billing
October 2011
Paper Claim Form Locators
CMS-1500
Fields
Description
24A to 24I
Top Half –
Shaded
Area
NATIONAL DRUG CODE INFORMATION – The shaded portion of fields 24A to 24I is
used to report NDC information. Required as of August 1, 2007.
To report this information, begin at field 24A as follows:
1. Enter the NDC qualifier of N4
2. Enter the NDC 11-digit numeric code
3. Enter the drug description
4. Enter the NDC Unit qualifier
F2 – International Unit
GR – Gram
ML – Milliliter
UN – Unit
5. Enter the NDC Quantity (Administered Amount) in the format 9999.99
DATE OF SERVICE – Provide the FROM and TO dates in MMDDYY format. Up to six
FROM and TO dates are allowed per form. Required.
24A
Bottom
Half
36
CMS-1500 Billing
October 2011
Paper Claim Form Locators
CMS-1500
Fields
Description
24B
PLACE OF SERVICE – Use the POS code for the facility where services were
rendered. Required.
For a list of POS codes, go to the Place of Service Codes Overview page on the CMS
Web site at cms.hhs.gov.
24C
EMG – Emergency indicator. This field indicates services were for emergency care for
service lines with a CPT or HCPCS code in field 24D. Enter Y or N. Required, if
applicable.
24D
PROCEDURES, SERVICES, OR SUPPLIES
CPT/HCPCS – Use the appropriate procedure code for the service rendered. Only one
procedure code is provided on each claim form service line. Required.
MODIFIER – Use the appropriate modifier, if applicable. Up to four modifiers are
allowed for each procedure code. Required, if applicable.
DIAGNOSIS CODE – Enter number 1–4 corresponding to the applicable diagnosis
codes in field 21. A minimum of one, and a maximum of four, diagnosis code references
can be entered on each line. Required.
24E
37
CMS-1500 Billing
October 2011
Paper Claim Form Locators
CMS-1500
Fields
Description
24F
$ CHARGES – Enter the total amount charged for the procedure performed, based on
the number of units indicated in field 24G. The charged amount is the sum of the total
units multiplied by the single unit charge. Each line is computed independently of other
lines. This is a 10-digit field. Required.
24G
DAYS OR UNITS – Provide the number of units being claimed for the procedure code.
Six digits are allowed, and 9999.99 units is the maximum that can be submitted. The
procedure code may be submitted in partial units, if applicable. Required.
24H
EPSDT Family Plan – If the patient is pregnant, indicate with a P in this field on each
applicable line. Required, if applicable.
38
CMS-1500 Billing
October 2011
Paper Claim Form Locators
CMS-1500
Fields
Description
24I
Top Half –
Shaded
Area
RENDERING ID QUALIFIER – Enter the qualifier indicating what the number reported in
the shaded area of 24J represents – 1D for IHCP LPI rendering provider number or ZZ
for rendering provider taxonomy code.
1D is the qualifier that applies to the IHCP provider number (LPI) for atypical
nonhealthcare providers. The LPI includes nine numeric characters. Atypical providers
(for example, certain transportation and waiver service providers) are required to
submit their LPIs.
ZZ is the qualifier that applies to the provider taxonomy code. The taxonomy code
includes 10 alphanumeric characters. The taxonomy code may be required for a one-toone match.
Taxonomy – Enter the taxonomy code of the rendering provider. Taxonomy may be
needed to establish a one-to-one NPI/LPI match if the provider has multiple locations.
24J
Top Half –
Shaded
Area
RENDERING PROVIDER ID – Enter the LPI if entering the 1D qualifier in 24I for the
Rendering Provider ID. Required, if applicable for non-healthcare providers only.
LPI – The entire nine-digit LPI must be used. If billing for case management, the case
manager’s number must be entered here.
39
CMS-1500 Billing
October 2011
Paper Claim Form Locators
CMS-1500
Fields
Description
24J
Bottom
Half
RENDERING PROVIDER NPI – Enter the NPI of the rendering provider. Required if
applicable.
28
TOTAL CHARGE – Enter the total of all service line charges in column 24F. This is a 10digit field, such as 99999999.99. Required.
29
AMOUNT PAID – Enter the payment received from any other source, excluding the
Medicare paid amount. All applicable items are combined and the total entered in this
field. This is a 10-digit field. Required, if applicable.
Other insurance – Enter the amount paid by the other insurer. If the other insurer was
billed but paid zero, enter 0 in this field. Attach denials to the claim form when submitting
the claim for adjudication.
BALANCE DUE – TOTAL CHARGE (field 28) – AMOUNT PAID (field 29) = BALANCE
DUE (field 30). This is a 10-digit field, such as 99999999.99. Required.
30
40
CMS-1500 Billing
October 2011
Paper Claim Form Locators
CMS-1500
Fields
Description
31
SIGNATURE OF PHYSICIAN OR SUPPLIER INCLUDING DEGREES OR
CREDENTIALS – An authorized person, someone designated by the agency or
organization, must sign and date the claim. A signature stamp is acceptable; however, a
typed name is not. Providers that have signed the Claims Certification Statement for
Signature on File form will have their claims processed when a signature is omitted from
this field. The form is available on the Forms page on indianamedicaid.com. Required if
applicable.
DATE – Enter the date the claim was filed. Required.
BILLING PROVIDER INFO & PH # – Enter the billing provider office location name,
address, and the ZIP Code+4. Required.
33
Note: If the U.S. Postal Service provides an expanded ZIP Code (ZIP Code + 4) for a
geographic area, this expanded ZIP Code must be entered on the claim form.
33a
41
CMS-1500 Billing
BILLING PROVIDER NPI – Enter the billing provider NPI. Required.
October 2011
Paper Claim Form Locators
CMS-1500
Fields
Description
33b
BILLING PROVIDER QUALIFIER AND ID NUMBER – Healthcare providers may enter
a billing provider qualifier of ZZ and taxonomy code. Taxonomy may be needed to
establish a one-to-one NPI/LPI match if the provider has multiple locations.
If the billing provider is an atypical provider, enter the qualifier 1D and the LPI. Required.
Note: Qualifiers are ZZ = Taxonomy and 1D = LPI
42
CMS-1500 Billing
October 2011
Explain
Billing Guidelines
Billing Guidelines
Provider classifications
– Billing Provider – Provider classification assigned to a billing
entity or solo practitioner at a service location
– Group Provider – The classification given to a corporation or
other business structure that has rendering providers linked that
are the performers of the services provided
– Rendering Provider – A provider that performs the services for a
group or clinic and is linked to the group or clinic
– Dual – A billing provider performing services as a sole proprietor
at an assigned service location and is also a rendering provider
working for a group
44
CMS-1500 Billing
October 2011
Billing Guidelines
Anesthesia
– Use Current Procedural Terminology
(CPT®) codes 00100-01999 (refer to
IHCP Provider Manual chapter 8 for
more information)
– One unit = 15 minutes
– Bill the actual time in minutes and
include it in field 24G
– Additional units are allowed based on a
patient’s age when billing for emergency
services (bill using procedure code
99140)
CPT is copyright 2010 American Medical Association. All rights reserved. CPT® is a registered trademark of
the American Medical Association.
45
CMS-1500 Billing
October 2011
Billing Guidelines
Anesthesia
– Providers bill postoperative pain
management using code 01996
– The IHCP does not separately
reimburse this code on the same day the
epidural is placed
•
However, it is reimbursed for subsequent days
when an epidural is managed
Note: When two claims for the same billing
NPI but with different rendering NPIs are
denying for edit 4181, they need to be
special batched. Contact your field
consultant .
46
CMS-1500 Billing
October 2011
Billing Guidelines
Chiropractic services
– IHCP limits chiropractic services to 50
per member, per calendar year
• The
IHCP reimburses for no more than five
office visits out of the 50 total units
– Package B reimbursement is
available for medically necessary
pregnancy-related services. Refer to
Chapter 8 of the IHCP manual for a
listing of pregnancy diagnosis codes.
– Package C members are allowed five
office visits and 14 therapeutic
physical medicine treatments per
member, per calendar year
47
CMS-1500 Billing
October 2011
Billing Guidelines
Chiropractic services
– The following are covered codes for office
visits:
•
99201, 99202, 99203, 99211, 99212, 99213
– The following are covered codes for
manipulative treatment:
•
98940-98943
Note: Services denied by Medicare must be
billed as Medicaid primary claims and
be submitted with the Medicare
Remittance Notice (MRN)
48
CMS-1500 Billing
October 2011
Billing Guidelines
Injections
– The IHCP reimburses for physician office
injectable drugs using Healthcare
Common Procedure Coding System
(HCPCS) J codes and CPT immunization
codes
– Pricing includes the current average
wholesale price plus a $2.90
administration fee
– The IHCP reviews pricing for a physician
office administered drug each quarter
– To price appropriately, HCPCS code
J3490 must be submitted with the
appropriate NDC, name, strength, and
quantity
49
CMS-1500 Billing
October 2011
Billing Guidelines
Injections and NDC codes
– The IHCP Provider Manual contains lists of J codes that
require a National Drug Code (NDC)
•
Chapter 8, Section 4
– For paper CMS-1500 claims forms, report NDC information
in the shaded area of field 24
•
Refer to bulletin BT200713 dated May 29, 2007
– The NDC is not used for provider reimbursement
50
CMS-1500 Billing
October 2011
Billing Guidelines
Mental health RBMC
– Outpatient mental health services are carved-in to the riskbased managed care (RBMC) delivery system
– Services provided to RBMC members by the following specialty
types are the responsibility of the managed care entities
(MCEs):
51
•
Freestanding Psychiatric Hospital
•
Outpatient Mental Health Clinic
•
Community Mental Health Center
•
Psychologist
•
Certified Psychologist
•
Health Service Provider in Psychology (HSPP)
•
Certified Clinical Social Worker
•
Psychiatric Nurse
•
Psychiatrist
CMS-1500 Billing
October 2011
Billing Guidelines
Mental health RBMC
Services that are the MCE’s responsibility:
– Office visits with a mental health diagnosis
– Services ordered by a provider enrolled in
a mental health specialty, but provided by
a nonmental health specialty (such as a
laboratory and radiology)
– Mental health services provided in an
acute care hospital
– Inpatient stays in an acute care hospital or
freestanding psychiatric facility for
treatment of substance abuse, chemical
dependency or patients with a mental
health diagnosis
52
CMS-1500 Billing
October 2011
Billing Guidelines
Medicaid Rehabilitation Option (MRO)
– Effective July 1, 2010, MRO services no longer require the
use of modifiers to note the midlevel scope of practice
– MRO services require the use of the HW modifier
– Providers should use the NPI of the supervising
practitioner, which is the physician or health service
provider in psychology (HSPP)
– Group setting should be billed using the U1 modifier
Note: When billing Group setting for addiction counseling,
do not use a modifier
Refer to Bulletin BT201023 dated July 8, 2010
53
CMS-1500 Billing
October 2011
Billing Guidelines
Mental health RBMC
– MCEs
•
Anthem
anthem.com
•
Managed Health Services (MHS)
managedhealthservices.com
•
MDwise
mdwise.org
– Behavioral Health Organizations (BHOs)
54
•
Anthem
anthem.com
•
Cenpatico (MHS)
cenpatico.com
•
MDwise
mdwise.org
CMS-1500 Billing
October 2011
Billing Guidelines
Surgical services
Cosurgeons:
– Cosurgeons must append modifier 62 to the surgical
services
– Modifier 62 cuts the reimbursement rate to 62.5% of the
rate on file
Bilateral Procedures:
– To indicate a bilateral procedure, providers bill with one unit
in field 24G, using modifier 50
– Use of this modifier ensures that the procedure is priced at
150% of the billed charges or the rate on file
Note: If the CPT code specifies the procedure as bilateral,
then the provider must not use modifier 50
55
CMS-1500 Billing
October 2011
Billing Guidelines
Surgical services
– Postoperative care for a surgical procedure includes 90
days following a major procedure surgical procedure and
10 days following a minor surgical procedure
– Separate reimbursement is available for care during the
global postoperative period for:
•
Services unrelated to the surgical procedure
•
Care not considered routine
•
Postoperative care for surgical complications
–
For surgery codes only, separate reimbursement is
available for surgeries that have unusual complications
using modifier 22
– Additional documentation is required
56
CMS-1500 Billing
October 2011
Billing Guidelines
Multiple surgery procedures
– When two or more covered surgeries are performed during
the same operative session, multiple surgery reductions
apply to the procedure based on the following adjustments:
•
100% of the global fee for the most expensive procedure
•
50% of the global fee for the second most expensive procedure
•
25% of the global fee for the remaining procedures
– All surgeries performed on the same day, by the same
rendering physician, must be billed on the same claim form;
otherwise, the claim will be denied and the original claim may
be adjusted
57
CMS-1500 Billing
October 2011
Billing Guidelines
Therapy services requirements
– A qualified therapist or qualified assistant under the direct
supervision of the therapist, must provide the therapy
– Therapy must be provided at the level of complexity that is
based on the condition of the member based on the
evaluation
– Reimbursement is made only for medically reasonable and
necessary therapy
– The IHCP does not cover therapy rendered for diversional,
recreational, vocational, maintenance therapy or avocational
purposes, or for the remediation of learning disabilities or
developmental activities that performed by nonmedical
personnel
– Coverage is not provided for rehabilitative services for a
member longer than two years from the initiation of the
therapy unless a significant change in medical condition
58
CMS-1500 Billing
October 2011
Billing Guidelines
Therapy services requirements
– When a member is receiving therapy, ongoing evaluations to assess progress
or lack of progress are part of the program
•
The IHCP does not separately reimburse for ongoing evaluations
– One hour of billed therapy must include a minimum of 45 minutes of direct
patient care with the balance of the hour spent in related patient services
– The IHCP does not approve any type of therapy services for more than one
hour per day per type of therapy
59
CMS-1500 Billing
October 2011
Billing Guidelines
Therapy services – Physical therapist assistant (PTA) billing
• The PTA is precluded from performing and interpreting tests, conducting
initial or subsequent assessments, and developing treatment plans
60
•
Under direct supervision, a PTA is still required to consult with the
supervising physical therapist daily to review treatment
•
The consultation can be either face-to-face or by telephone
•
Claims will be billed with modifier HM – Less than a bachelor’s degree –
with the code billed and the rendering supervisor’s NPI
•
Pricing for these services will be at 75% of the fee on file for the
procedure billed
•
Chapter 8, section 4 provides a listing of codes that can be billed by a
PTA
CMS-1500 Billing
October 2011
Billing Guidelines
Podiatry services – Routine foot care
– Routine foot care is only covered if a
member has been seen by a medical
doctor or doctor of osteopathy for treatment
or evaluation of a systemic disease during
the six-month period prior to rendering
routine foot care
– A maximum of six routine foot care
services is covered per rolling 12-month
period when the member has one of the
following:
61
•
Systemic disease of sufficient severity that a
treatment of the disease may pose a hazard when
performed by a nonprofessional
•
Systemic conditions that result in severe circulatory
embarrassment or has had areas of desensitization
in the legs or feet
CMS-1500 Billing
October 2011
Billing Guidelines
Podiatry services – routine foot care
– ICD-9-CM diagnosis codes that
represent systemic conditions that justify
coverage for routine foot care:
•
Diabetes mellitus: ICD-9-CM codes 250.00250.91
•
Arteriosclerotic vascular disease of lower
extremities: ICD-9-CM codes 440.20-440.29
•
Thromboangitis oblierans: ICD-9-CM code 443.1
•
Post-phlebitis syndrome: ICD-9-CM code 459.1
•
Peripheral neuropathies of the feet: ICD-9-CM
codes 357.1-357.7
– Routine foot care is not a covered
service for Package C members
62
CMS-1500 Billing
October 2011
Billing Guidelines
Podiatry services – routine foot care
– Reimbursement is limited to one office visit using
procedure code 99211, 99212, and 99213 per member, per
12 months, without obtaining prior authorization
– New patient office visits, using procedure codes 99201,
99202, and 99203 are reimbursable at one per member,
per provider, within the last three years as defined by the
CPT guidelines
– On the initial visit, both the office visit and the procedure
performed are reimbursable
– For subsequent visits, reimbursement for the visit is
included in the procedure performed on that date and not
billed separately
•
63
Exception: If a second, significant problem is addressed on a
subsequent visit, the visit code may be reported with the 25 modifier
CMS-1500 Billing
October 2011
Billing Guidelines
Evaluation and management codes
– Reimbursement is available for office visits to a maximum
of 30 per rolling 12-month period, per IHCP member,
without prior authorization (PA), and subject to the
restrictions in Section 2 of 405 IAC 5-9-1
– Per 405 IAC 5-9-2, office visits should be appropriate to the
diagnosis and treatment given and properly coded
Procedure Codes
99201-99215
99241-99245
99271-99275
64
CMS-1500 Billing
October 2011
99381-99397
99401-99429
Billing Guidelines
Evaluation and management codes
– Professional services rendered during the course of a
hospital stay must be submitted on Web interChange,
using the electronic 837P transaction or on a paper CMS1500 claim form
– The IHCP makes reimbursement in accordance with the
appropriate professional fee schedule
– The inpatient diagnosis-related group (DRG)
reimbursement methodology does not provide payment for
physician fees, including the hospital-based physician fee
– New patient office visits are limited to one visit per member,
per billing provider – once every three years
65
CMS-1500 Billing
October 2011
Billing Guidelines
Obstetric services
– The IHCP covers the following 14 antepartum visits:
•
Three visits in trimester one
•
Three visits in trimester two
•
Eight visits in trimester three
– Providers use the following codes to bill for visits:
•
First visit – Evaluation and management (E/M) – 99201-99205
•
Visits one through six – 59425
•
Seventh and subsequent visits – 59426
– Providers use the following modifiers with procedure codes:
66
•
U1 for trimester one – Zero through 14 weeks
•
U2 for trimester two – 14 weeks, one day through 28 weeks
•
U3 for trimester three – 28 weeks, one day through delivery
CMS-1500 Billing
October 2011
Billing Guidelines
Pregnancy-related claims
– For pregnancy-related claims, indicate
the last menstrual period (LMP) in
MM/DD/YY format in
field 14
•
The IHCP will deny claims for pregnancyrelated services if there is no LMP
– Indicate a pregnancy-related
diagnosis code as the primary
diagnosis when billing for pregnancyrelated services
67
CMS-1500 Billing
October 2011
Billing Guidelines
Pregnancy diagnosis codes
– Use normal low-risk pregnancy diagnosis codes:
•
V22.0
•
V22.1
– Use high-risk pregnancy codes:
•
V60.0 through V62.9
For additional information, refer to the IHCP Provider Manual,
Chapter 8, Section 4
68
CMS-1500 Billing
October 2011
Describe
Sterilization and Partial Sterilization
Consent Form
70
CMS-1500 Billing
October 2011
Sterilization and Partial Sterilization
Partial sterilization
– A sterilization form is not necessary
when a patient is rendered sterile as a
result of an illness or injury
•
Providers must note partial sterilization with an
attachment to the claim indicating “Partial
Sterilization” and no consent required
– Partial sterilization can also be
submitted on the electronic 837P
transaction when “Partial Sterilization”
is indicated in the claim notes
71
CMS-1500 Billing
October 2011
Sterilization Procedure
Hysteroscopic Sterilization Procedure
– Can be performed in the office as an outpatient or in an
ambulatory surgical center (ASC)
– Device billed separately on CMS-1500 form using sterilization
HCPCS code A9900 – Miscellaneous supply, accessory, and/or
service component of another HCPCS code
– Use primary diagnosis code of ICD-9-CM V25.2 – Sterilization
– Print “Sterilization Device Implant” on the claim form or
accompanying invoice
– Submit cost invoice with claim
– Submit a valid, signed Sterilization Consent form
– Print Hysteroscopic Sterilization Procedure on the claim form or
on the invoice
Refer to BR201006 for more information
72
CMS-1500 Billing
October 2011
Explain
Prior Authorization
Prior Authorization
– Providers must verify member eligibility to determine the care
management organization (CMO) that will process the PA or Update
request
•
CMO information via Web interChange is real time
•
Send the PA request to the assigned CMO as of the date of the request
•
Send System Update Request form to the original CMO
– Example:
74
•
Member is assigned to MDwise on 4/3/11, when the PA is requested
•
On 4/15/11, the member transitions from MDwise to ADVANTAGE
•
On 4/23/11, the primary medical provider (PMP) requests a System Update to the PA
•
The PMP must request the System Update from MDwise
CMS-1500 Billing
October 2011
Prior Authorization
– Members can be reassigned from traditional Medicaid fee-for-service,
to Hoosier Healthwise/RBMC, or Care Select
– When the member changes programs, the receiving organization must
honor PAs approved by the prior organization for the first 30 days
following the reassignment, or for the remainder of the PA dates of
service, whichever comes first
– Example:
75
•
Member transitions from Hoosier Healthwise/RBMC to a Care Select CMO on
September 15, 2011
•
The MCE approved PA for dates of service 9/6/11 through 10/30/11
•
The Care Select CMO must honor the approved PA for 30 days from September 15,
2011
CMS-1500 Billing
October 2011
Prior Authorization
Member changes within a program
– When members transition from one CMO to another CMO, or from
Traditional Medicaid to Care Select, the receiving organization must
honor the approved PA until the PA expires
76
CMS-1500 Billing
October 2011
Prior Authorization
– Each CMO is responsible for processing medical service PA requests
and updates for members assigned to their organization at the time of
the request
– Traditional Medicaid fee-for-service PA requests are processed by
ADVANTAGE Health Solutions
– Pharmacy PA requests continue to be processed by Affiliated
Computer Services (ACS)
77
CMS-1500 Billing
October 2011
Prior Authorization Contact Information
– ADVANTAGE Health Solutions (fee-for-service)
•
P.O. Box 40789
Indianapolis, IN 46240
1-800-269-5720
1-800-689-2759 (Fax)
– ACS (Pharmacy)
•
78
1-866-879-0106
1-866-780-2198 (Fax)
CMS-1500 Billing
October 2011
Prior Authorization Contact Information
– MDwise – Care Select
•
P.O. Box 44214
Indianapolis, IN 46244-0214
1-800-356-1204
1-877-822-7186 (Fax)
– ADVANTAGE Health Solutions – Care Select
•
79
P.O. Box 80068
Indianapolis, IN 46280
1-800-440-2449
1-800-689-2759 (Fax)
CMS-1500 Billing
October 2011
Inform
Code Sets
Code Sets
The following provider types have specific code sets:
– Chiropractic
– Durable Medical Equipment
– Hearing Services
– Home Medical Equipment
– Optician
– Optometrist
– Transportation
– Vision
All code sets can be referenced on the
provider.indianamedicaid.com Web site
81
CMS-1500 Billing
October 2011
Describe
IHCP Fee Schedule
Fee Schedule
– The IHCP Fee Schedule is available on
the IHCP Web site and provides the
following information:
83
•
Coverage
•
Pricing for procedure codes
•
PA requirements for individual procedure codes
CMS-1500 Billing
October 2011
Deny
Common Denials for CMS-1500
Edit 2502
Recipient covered by Medicare Part B
–
Cause
• Medical claims for Medicare Part B coverage for a member have Part B on the
eligibility screen but there is no Medicare MRN with the claim showing
Medicare denial
–
Resolution
• Submit the Medicare payment on the right side of field 22 and the coinsurance,
deductible, or blood deductible on the left side
– Resolution
•
85
Submit the coordination of benefits information
CMS-1500 Billing
October 2011
Edit 558
Coinsurance and deductible amount missing
–
Cause
• Coinsurance and deductible amount are missing, indicating this is not a
crossover claim
–
Resolution
• Add coinsurance and/or deductible amount and/or Medicare paid amount to
the CMS-1500
• CMS-1500
86
Add
coinsurance and/or deductible amount on the left side of field 22
Add
the Medicare Payment amount on the right side in field 22
CMS-1500 Billing
October 2011
Edit 2505
Recipient covered by private insurance
–
Cause
• This member has private insurance, which must be billed prior to Medicaid
–
Resolution
• Add the other insurance payment to the claim
• CMS-1500
Add
other insurance excluding Medicare payments to field 29
• If the primary insurance denies, the explanation of benefits (EOB) must be
sent with the claim, either on paper with a paper claim, or as an attachment if
claim is sent on Web interChange
87
CMS-1500 Billing
October 2011
Find Help
Resources Available
Helpful Tools
Avenues of resolution
– IHCP Web site at indianamedicaid.com
– IHCP Provider Manual (Web, CD, or paper)
– Customer Assistance
• Local
• All
(317) 655-3240
others 1-800-577-1278
– Written Correspondence
• HP
Provider Written Correspondence
P. O. Box 7263
Indianapolis, IN 46207-7263
– Provider field consultant
89
CMS-1500 Billing
October 2011
Q&A