Mechanics of Breathing - (www.ramsey.k12.nj.us).
advertisement

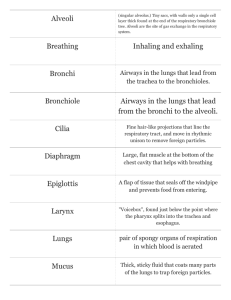
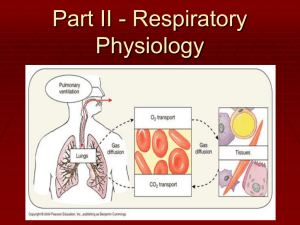
Pressure Relationships in the Thoracic Cavity Intrapulmonary pressure is the pressure in the alveoli, which rises and falls during respiration, but always eventually equalizes with atmospheric pressure. Intrapleural pressure is the pressure in the pleural cavity. It also rises and falls during respiration, but is always about 4mm Hg less than intrapulmonary pressure. Importance of Pressure Relationships Transpulmonary pressure (Palv – Pip) keeps the airspaces of the lungs open. The negative pressure of the intrapleural space and the tight coupling of the lungs to the thoracic walls is extremely important. If intrapleural pressure is equalized with intrapulmonary or atmospheric pressure, lung collapse will occur immediately Atelectasis (lung collapse) commonly occurs when air enters the pleural cavity through a chest wound; it can also result from ruptured visceral pleura (usually due to pneumonia) allowing air to enter the pleural cavity from the respiratory tract Pneumothorax (air in the intrapleural space) is reversed by closing the hole and drawing air out of the intrapleural space with chest tubes, allowing lungs to reinflate and resume normal function. Pulmonary Ventilation Mechanical process causing gas flow into and out of the lungs according to volume changes in the thoracic cavity. (A.K.A. “Breathing”) Consists of two phases: Important physics rule to remember for breathing mechanics: Inspiration: period of time when air flows into the lungs Expiration: period of time when gases exit the lungs Volume changes lead to pressure changes Pressure changes lead to flow of gases to equalize pressure Boyle’s Law: (when temp constant) P1V1 = P2V2 At a constant temperare, pressure varies inversely with volume P = pressure in mm Hg V = volume in cubic mm Intrapulmonary & Intrapleural Pressure Relationships During Pulmonary Ventilation Gases, like liquids, conform to the shape of their container Unlike liquids, gases always fill their container In a large volume, the gas molecules will be far apart and the pressure will be low If the volume is reduced, the gas molecules will be compressed and the pressure will rise Inspiration Diaphragm and intercostals muscles contract Diaphragm moves inferiorly and flattens during contraction, causing height of thoracic cavity to increase Intercostals contraction lifts the ribcage and thrusts sternum forward, increasing anterioposterior and lateral dimensions (circumference) Lungs adhere tightly to the thorax walls (due to surface tension of fluid between pleural membranes), they are stretched to the new, larger size of the thorax. As intrapulmonary volume increases, gases with in the lungs spread out to fill the larger space. Resulting decrease in the gas pressure in the lungs produces a partial vacuum (pressure less than atmospheric pressure), which sucks the air into the lungs. Expiration Passive process that depends mostly on natural elasticity of the lungs than on muscle contraction. As inspiratory muscles relax and resume normal resting length, rib cage descends and lungs recoil. As the thoracic and pulmonary volume to decrease, gases inside the lungs are forced closer together and intrapulmonary pressure rises to above atmospheric pressure. This causes gases to flow out to equalize pressure inside and outside of the lungs. Normally this is a passive process, but if passageways are narrowed due to spasms of bronchioles (asthma) or clogged with mucus/fluid (bronchitis/pneumonia), it becomes an active process, using intercostal muscles to help depress rib cage and abdominal muscles to help squeeze air out of lungs. Events of Inspiration Steps of Expiration Physical Influences on Pulmonary Ventilation: Airway Resistance Friction in the respiratory passageways is the major non-elastic source of resistance to gas flow F = ΔP/R Gas flow in/out of the alveoli is directly proportional to the difference in pressure between the atmosphere and the alveoli, normally small changes in pressure cause large changes in volume of gas flow (gradient ~2mmHg less, moves 500mL air in/out per breath) Gas flow inversely changes with resistance, which is mainly determined by conducting tube diameter. Resistance is usually insignificant because relatively speaking they are huge at the initial part of the conducting zone and as the diameter gets small diffusion takes over. Greatest resistance is in the bronchi. Inhaled irritants & inflammatory chemicals can cause constriction of the bronchioles and reduce air passage, accumulation of mucus or infectious material can also increase resistance Physical Influences on Pulmonary Ventilation: Alveolar Surface Tension Forces At a liquid-gas boundary, the molecules of liquid are more strongly attracted to each other than to the gas. This produces a surface tension at the liquid surface that draws the liquid molecules even closer and reduces contact with gas molecules and resists any force that tends to increase the area of the surface. The liquid film that coats the alveolar walls is always acting to reduce the alveoli to their smallest size. This film contains surfactant (as opposed to being pure water) to reduce surface tension. When too little surfactant is present, the excess surface tension can collapse the alveoli requiring complete reinflation with each breath, requiring tremendous energy (IRDS – infant respiratory distress syndrome) Physical Influences on Pulmonary Ventilation: Lung Compliance Healthy lungs are distensible (stretchy). The ease with which they can be expanded is called lung compliance. CL CL is a measure of the change of lung volume (ΔVL) that occurs with a given change in transpulmonary pressure (Δ[Palv – Pip) Meaning, the higher the lung compliance, the easier it is to expand the lungs at any transpulmonary pressure. The two factors that determine lung compliance are distensibility of lung tissue and the surrounding thoracic cage, and surface tension in the alveoli (contributes to elastic recoil). Excessive compliance indicates a loss of elastic recoil of the lungs, as in old age or emphysema. Decreased compliance means that a greater change in pressure is needed for a given change in volume, as in atelectasis, edema, fibrosis, pneumonia, or absence of surfactant. Respiratory Adjustments: Exercise Ventilation can increase 10-20x during exercise Breathing becomes deeper and more vigorous (“Hyperpnea”), but respiratory rate may not be significantly changed. Any respiratory changes meet metablolic demands so O2/CO2 levels in the blood are not altered. Change in breathing is prompted by rising CO2 and declining O2, which causes drop in blood pH. Respiratory Adjustments: High Altitude At elevation above 8000ft, air density and oxygen pressure are lower, which may cause symptoms of “acute mountain sickness” (AMS) Respiratory and hematopoietic adjustments occur called “acclimiatization”. Chemoreceptors become more responsive to increases in CO2/decreases in O2, resulting in increased ventilation. Within a few days, respiratory volume stabilizes at a level 2-3 L/min higher than at sea level.