Nerve Pathology
advertisement

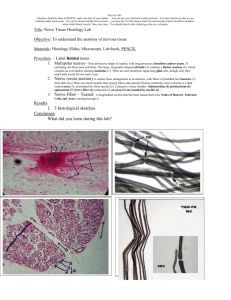
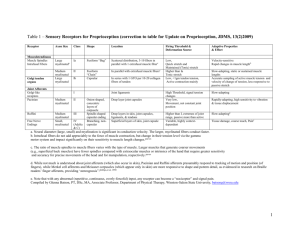
David Lacomis, MD Nerve Biopsy Major indication is “vasculitis” May not show specific cause of neuropathy in most cases Nerve Biopsy Processing Paraffin sections o Inflammation Semi-thin, plastic sections (most useful) o Axon-loss o Demyelination o Inflammation o Inclusions Teased Fibers o Demyelination and axonal degeneration Organization of Peripheral Nerve (H & E-Stained Paraffin-Embedded Section) cross-section of 4 fascicles Individual axons are surrounded by endoneurial connective tissue. Perineurial connective tissue (yellow arrow) surrounds fascicles. All fascicles are bundled in loose epineurial connective tissue (black arrow) that contains the larger blood vessels in addition to capillaries that can also be seen in the perineurium and endoneurium. Sural Nerve Cross-Section (Trichrome) The sheaths of myelinated axons stain red while the connective tissue stains blue. Higher power shows myelinated axons more clearly. Cross-Section: 1 Micron Thick (Toluidine Blue) Normal dist. of myelinated fibers in a 74 year-old woman. Younger people have more myelinated axons. Large-fibers (7 microns or larger) make up 40% and small-fibers compose 60% of myelinated axons. Unmyelinated fibers are also present in the nerve fascicle, but they are difficult to see without ultrastructural study. There is normally a bimodal distribution of myelinated fiber diameters. The thickness of the myelin sheath is generally proportional to the axon diameter. In some forms of polyneuropathy, such as hereditary motor sensory neuropathy type I, the large myelinated fibers may be preferentially affected, while in amyloidosis, for example, the small myelinated fibers may be preferentially affected. Normal Anatomy of a Single Axon The myelinated segments are called internodes. Internode length increases as does the axon diameter. For large axons, the internodal length ranges between 0.35 and 1.83 mm and is approximately 1/3 of that size for smaller myelinated axons. Especially in the elderly, there is significant variability in internodal length. One Schwann cell associated with unmyelinated axons (REMAK cells) may surround more than one axon. The unmyelinated fibers actually outnumber myelinated fibers approximately 4 to 1. Normal Single Teased Fibers from the Sural Nerve Due to osmication, the myelin sheath stains dark. Nodes of Ranvier border each internodal segment. Ultrastructural Study of a Normal Myelinated Fiber Normal myelin sheath thickness and axon contents The inner mesaxon (yellow arrow) is where the myelin sheath begins to overlap itself. The outer mesaxon (red arrow) in the site is where the last turn of the Schwann cell cytoplasm overlaps itself. At the Schmidt-Lanterman incisures, the state of the myelin sheath is noted. Reich’s Pi granules are normal variants and are structures present in the Schwann cell cytoplasm. They increase with age. They appear to be of lysosomal origin. (H&E, Paraffin) Polyglucosan bodies may be normal or seen in great numbers in a storage disease. The bodies are also PAS+. Renaut bodies are fibrillary structures present in the subperineurial area. They are composed predominantly of fibroblasts. They are lightly staining with H&E. Renaut bodies are also lightly stained with Trichrome. In contrast to amyloid deposits, they do not stain with Congo Red. These structures are normal variants. They do appear to be more common in areas of focal nerve compression and with aging. Renaut Body (Toluidine Blue-Stained Section) Axonal Degeneration (H&E- Stained Paraffin Section) Shows myelin ovoids due to contraction of the myelin sheath as the underlying axon degenerates. This phenomenon occurs in Wallerian degeneration distal to the site of axonal transection, and it also occurs in axonal polyneuropathies. In teased fibers, linear myelin ovoids are seen in a patient with an axonal polyneuropathy. Myelin ovoids may begin in the paranodal areas or adjacent to the SchmidtLanterman incisures. Myelin Ovoid in a Patient with Diabetic Neuropathy Significant dropout in large and small myelinated axons is present as well as a degenerating axon with debris-laden cytoplasm. Axonopathy Note fragmentation of the myelin sheath, contraction of the axon, and increased contents in the Schwann cell cytoplasm. Further fragmentation of the myelin sheath is shown in a degenerating axon. Axonal Polyneuropathy Perivascular macrophages containing Pi-like granules and lipid deposits are present, probably as a result of ingesting contents of degenerating myelinated axons. Ultrastructural Examination in a Patient with Axonal Polyneuropathy Examination reveals an increase in endoneurial collagen, a severe dropout in myelinated axons, and flat stacks of Schwann cell cytoplasm, consistent with a loss of the unmyelinated fibers. Cross-Section of Axonal Sprouts Muscle Nerve regeneration occurs within the Schwann cell tube. Midroni G et al. Biopsy Diagnosis of Peripheral Neuropathy. Butterworth-Heinemann. 1995. Denervated Schwann Cell Bands (Bands of Bungner) More rounded stacks of Schwann cell processes, sometimes in association with multiple axons within a single Schwann cell tube, are characteristic of Bands of Bungner. These bands are due to multiplication of Schwann cells of denervated myelinated and unmyelinated axons that had previously regenerated (see previous slide). If regeneration does not occur, these bands will totally collapse. Muscle Cross-section of sprouting nerve that then degenerated Cluster of Regenerating Myelinated Axons Clusters are defined by the presence of three or more closely opposed myelinated axons, generally within a single Schwann cell basal lamina. Eventually, the basal lamina will disintegrate and each myelinated axon will have its own basement membrane. Microfasciculation of Regenerating Axons Seen in diabetic neuropathies and ischemic neuropathies. Shown here are multiple microfascicles as well as thinly myelinated fibers and a dropout in myelinated fibers. Thinly myelinated fibers are often indicative of remyelination, but the remyelinating process is better seen with teased fibers. Myelin Ovoids in Diabetic Polyneuropathy End-Stage Diabetic Polyneuropathy A regenerating group of myelinated fibers is isolated in a nerve that is severely damaged in diabetic polyneuropathy. Diabetic Polyneuropathy Very few remaining axons are present. Also note the thickening of the capillary (arrow). Also associated with thickening of the perineurium (). * Overt degeneration of the perineurium may also be seen in diabetic polyneuropathy. Demyelinating Neuropathy Segmental demyelination is shown in two internodes. Onion Bulbs Redundant layers of Schwann cell processes are noted surrounding myelinated axons. Onion bulbs are indicative of demyelination and remyelination. They may be seen with inherited demyelinating polyneuropathies or other more chronic acquired demyelinating neuropathies such as chronic inflammatory demyelinating polyneuropathy (CIDP). Inflammatory Neuropathies Mononuclear inflammatory cells are seen adjacent to myelinated axons of the lumbar roots in a patient with Guillain-Barré Syndrome. Vesicular demyelination is noted in a patient with Guillain-Barré Syndrome. In GBS, macrophages will strip the myelin from the axon. Chronic Inflammatory Demyelinating Polyneuropathy Onion bulbs, which are present in this specimen, may be seen in approximately 15-40% of patients. Significant axon loss as is shown here is quite common. Teased fibers show a mixture of demyelination and axonal loss. Thus, the pathologic findings of CIDP are mixed and often do not allow a definitive pathologic diagnosis. Chronic Inflammatory Demyelinating Polyneuropathy Endoneurial and perivascular inflammation is seen in approximately 10 to 50% of patients with CIDP (leukocyte common antigen immunohistochemistry). Necrotizing Vasculitis An artery with fibrinoid necrosis and inflammatory cell invasion within the vascular wall is shown in the epineurium. Necrotizing vasculitis is also seen in an intramuscular artery from the same patient. The diagnostic yield in patients with suspected peripheral nervous system vasculitis is increased when both muscle and nerve are biopsied. Patchy Loss of Myelinated Axons in a Patient with Vasculitic Polyneuropathy The fascicular loss is thought to be due to endoneurial ischemia within the central region of the fiber or in sectors. Such a spatial pattern of loss is also seen in some patients with diabetic polyneuropathy. Thus, this is thought to be a feature of an ischemic process. Subperineurial edema is an early feature in vasculitic neuropathy. Paraneoplastic Neuropathy DRG Neuron Lymphocytic dorsal root ganglionitis is typical of paraneoplastic sensory neuropathy. Sarcoidosis Sural nerve specimen shows a typical perivascular granuloma in the epineurium. Multinucleated giant cells are not commonly seen in neural sarcoidosis. Perineuritis Perineuritis manifested as a sensory neuropathy is associated with patchy infiltration of the perineurial lamellae by epitheliod cells and lymphocytes. An example of toxic neuropathy is that induced by amiodarone. In this particular neuropathy, there is a demyelinating element and lipid inclusions can be seen in Schwann cell cytoplasm. Most toxic neuropathies, however, cause an axonal polyneuropathy. Amyloid Polyneuropathy Endoneurial Congo Red positive staining is present. The Congo Red positive material has the characteristic features of apple-green birefringence with polarized light. Leprosy Bacilli can be seen within perineurial cells, endothelial cells, and within macrophages in this disorder. Leprosy is the most common cause of neuropathy in many third world countries. CMT-1 Normal HMSN-I or Charcot-Marie Tooth disease type I is a chronic demyelinating polyneuropathy in which many onion bulbs are commonly seen. Onion Bulbs in CMT-1 Genetic studies may be more useful in diagnosing some inherited neuropathies. This image reveals FISH in a patient with a duplicated PMP 22 segment on chromosome 17 due to CMT 1a. In hereditary liability to pressure palsies, due to a deleted PMP22 segment, numerous sausage-like swellings or tomaculae are present on teased fiber preparations.