Thrombocytopenia
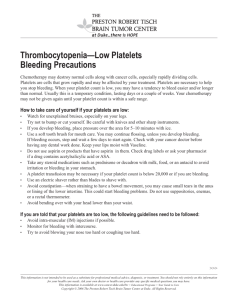
advertisement

Sadie T. Velásquez, M.D. 60-year-old white male presented with a 4-day history of bleeding from the gums, diffuse spontaneous ecchymoses, mild fatigue, and bone pain. The patient described a 6-month history of pain localized to his right thigh with extension to the posterior part of his right leg. Pt sent from an OSH for an abnormal peripheral smear. PMH: atrial fibrillation, hypercholesterolemia, and hypertension PSH: appy Social: no tobacco; moderate alcohol consumption until 1 year ago. Meds: ASA 325mg daily, metoprolol 50mg bid, simvastatin 40mg daily, HCTZ 25mg daily Physical: BP 138/64, P 57, T 98, RR 18 HEENT: dry blood in oropharynx Pulm: CTA Abdomen: liver and the spleen were not palpable. BLE: confluent ecchymoses involving the left ankle, B thighs posteriorly Laboratory values: Hb 13.4, platelets 107K, leukocytes 8.1, LFTs normal, creatinine normal, PTT 45, INR 1.92, fibrinogen <0.30 g/L, D-dimers >4 μg/mL (normal:≤0.40 μg/mL). Normal factors V, VII, XIII, and activated protein C Initial OSH Smear: consistent with a normochromic, normocytic anemia, with reduced platelets and large forms, and possible blasts with folded nuclei OSH PSA returns 2 days after admission at 276 smear 27-year-old woman is evaluated in the ER for a two-day history of HA, fatigue and gingival bleeding on brushing her teeth. She is otherwise healthy. Her only medication is an oral contraceptive, and medical and family histories are unremarkable. Physical: T 98.6, HR 65, BP 110/65, RR 18, SaO2 98% General: alert and oriented but reports having a headache. HEENT: Funduscopic examination is normal. There are a few scleral hemorrhages, and mild icterus is noted. Skin: Petechiae that had gone unnoticed by the patient are visible on the lower extremities. Laboratory studies: Hb 8 g/dL; platelet count of 34,000/µL; reticulocyte count of 12% of erythrocytes INR 1.1, aPTT 32 LDH 2000 creatinine 0.8 D-dimer negative Definition of thrombocytopenia Discuss the initial evaluation of thrombocytopenia Discuss major causes of thrombocytopenia Discuss the guidelines of each cause to include evaluation and management Normal platelet count 150-450,000/microL Produced in the bone marrow from megakaryocytes ~ 1000 - 5000 platelets are produced by each megakaryocyte Platelets survive in the circulation for 8 to 10 days Mechanisms for a reduced platelet count: decreased production increased destruction dilutional or distributional thrombocytopenia pseudothrombocytopenia Can occur when the marrow is suppressed or damaged After viral infections (eg, rubella, mumps, varicella, parvovirus, HCV, EBV) Certain infectious agents (HIV) Following chemotherapy or XRT to sites of platelet production Congenital or acquired bone marrow aplasia or hypoplasia Direct alcohol toxicity Vitamin B12 and folic acid deficiency ITP Drugs: heparin, quinine, quinidine, and valproic acid Alloimmune destruction (post-transfusion, neonatal, post transplantation) DIC TTP-HUS APL syndrome The HELLP syndrome Following certain infections (infectious mononucleosis, cytomegalovirus) HIV HIT Asymtomatic Menorrhagia Petechiae Purpura Gingival bleeding Ecchymoses History Medications Recent infection Prior hematologic disease Other medical history and current diseases Family history Recent vaccination Nutritional status Pregnancy Recent organ transplantation Recent transfusion Physical exam Ocular fundus for evidence of bleeding Lymphadenopathy, hepatosplenomegaly, and other masses Stool exam Laboratory CBC and smear Decreased platelet production Circulating blast cells A leukoerythroblastic blood picture Other cytopenias suggest the presence of a MD state Macrocytosis with hypersegmented PMNs=B12 or folic acid deficiency Normal sized or small platelets, in contrast to large sized platelets, suggest a reduced bone marrow response Increased destruction Evidence of MAHA Large platelets Associated autoimmune disease Underlying lymphoproliferative disease May be helpful Attention: Normal to increased numbers of megakaryocytes Decreased numbers of megakaryocytes In a hypercellular marrow, megaloblastic changes in the red cell and granulocytic series suggests vitamin B12 or folic acid deficiency, while dysplastic changes in the red cell, granulocytic, and megakaryocytic lineages suggests a myelodysplastic disorder Granulomata, increased reticulin or collagen fibrosis or infiltration with malignant cells establishes the diagnosis of marrow invasion Severe reduction or absence of megakaryocytes with no other abnormalities may be due to the presence of an autoantibody directed against the thrombopoietin receptor, seen in SLE Definition of thrombocytopenia Discuss the initial evaluation of thrombocytopenia Discuss major causes of thrombocytopenia Discuss the guidelines of each cause to include evaluation and management Underlying disorder associated with DIC Systemic activation of coagulation Widespread fibrin deposition Consumption of platelets and coagulation factors Microvascular thrombosis Thrombocytopenia and coagulation factor deficiency Organ failure Bleeding Sepsis and severe infection Trauma Organ destruction Malignancy Obstetric Vascular abnormalities Severe liver failure Toxic and immunological insults Clinical suspicion supported by relevant laboratory tests Screen with PTT, aPTT or platelet count Fibrin degradation products and D-dimers may be helpful Fibrinogen can be normal in as many as 57% of patients Peripheral smear with fragmented RBCs Scoring system (ISTH 5 step diagnostic algorithm) Sensitivity 91%, specificity of 97% Risk assessment: Does the pt have an underlying disorder known to be associated with overt DIC? Yes →proceed No →stop Order global coags (PT, platelets, fibrinogen, fibrin related marker) Score the test results Platelets > 100K=0, <100K=1, <50K=2) Elevated fibrin maker (D-dimer, FDP) no increase=0, moderate =2, strong=3 Prolonged PT <3s=0, >3 but <6s=1, >6s=2) Fibrinogen level >1g/l=0, <1=1 Calculate score: ≥5 compatible with overt DIC, repeat score daily <5 suggestive for non-overt DIC; repeat next 1-2 days Treatment of the underlying condition Plasma and platelets: Transfuse platelets if platelets are <50K and bleeding In non-bleeding pts, 10-20K and/or on clinical features In bleeding patients, fibrinogen deficiency can be corrected with purified fibrinogen or cryoprecipitate. 3g would raise fibrinogen by around 1g/l and can be given as 4 units of FFP, two cryoprecipitate pools or 3g of a fibrinogen concentrate. If thrombosis predominates, therapeutic doses of heparin should be considered In critically ill, non-bleeding patients, prophylaxis for DVTs with heparin or LMWH is recommended Initially described by Dr Eli Moschcowitz at the Mount Sinai Hospital in New York City in 1925. Moschcowitz ascribed the disease to a toxic cause. Moschcowitz noted that his patient, a 16 year-old girl, had anemia, petechiae (purpura), microscopic hematuria, and, at autopsy, disseminated microvascular thrombi. Predominant histologic abnormality is the formation of platelet microvascular thrombi Idiopathic TTP: Deficiency of ADAMSTS13 Secondary TTP: drugs, post bone marrow transplatation, SLE, malignancy, pregnancy, infection (HIV, E. coli 0157:H7) Severe thrombocytopenia (usually lower than HUS)* Microangiopathic hemolysis (schistocytes, polychromasia)* May be absent from the peripheral smear in the first 24- 48 hours after presenation Neurologic signs Renal impairment Difficult to differentiate from HUS if this predominates Fever Full blood count and smear Reticulocyte count Clotting screen including fibrinogen and D-dimers Urea and electolytes LFTs LDH UA Direct antiglobulin test Plasma exchange (has decreased mortality from 90 to 10-30%) initiated within 24 hours of presentation Average number of procedures is 3-36 Daily plasma exchange should be continued for a minimum of 2 days after complete remission Adjunctive treatment with corticosteroid therapy is recommended for all with pulse methylprednisolone 1gIV x 3 days Antiplatelet therapy with low-dose ASA should be commenced on platelet recovery (>50K) Supportive therapy with RBC transfusion as needed Supplement with folate in all patients Platelet transfusions are contraindicated unless there is life-threatening hemorrhage MAHA, thrombocytopenia and renal failure Clinical overlap with TTP Epidemic form associated with bloody diarrhea (90% VTEC) Secondary causes include post solid organ/BMT, drugs, SLE, malignancy, pregnancy and familial deficiency or defect in complement Meticulous fluid and electrolyte balance and BP control HD as required Avoid anti-motility drugs and antibiotic treatment due to adversely affecting outcome FFP and plasma exchange have not been shown to improve outcome HIT type II: immune-mediated disorder characterized by the formation of antibodies against the heparin-platelet factor 4 complex * HIT antibodies activate platelets intravascularly causing release of platelet microparticles and increased thrombin generation. Activated platelets are removed prematurely from the circulation Type I HIT: lesser fall in platelets within the first two days after heparin initiation and often returns to normal with continued heparin administration. Nonimmune. Typical onset HIT usually occurs days 5-10 (seroconversion) and days 7-14 (threshold defining thrombocytopenia Rapid-onset HIT (fall in 24 hours) is strongly associated with recent heparin exposure (30-100 days) Three factors associated with HIT: Unfractionated heparin (UFH) >low molecular weight heparin (LMWH) Surgical > medical patients Female > Male Suspect if one of the below with heparin in the preceding 5-10 days: Onset of unexplained thrombocytopenia Venous or arterial thrombosis with thrombocytopenia Platelet decrease by ≥ 50 percent, even if absolute thrombocytopenia is not present Necrotic skin lesions at heparin injection sites Anaphylactoid reactions occurring after IV heparin bolus Initial diagnosis is clinical Serotonin release assays*, heparin-induced platelet aggregation assays, and solid phase immunoassays to confirm the diagnosis 0-3: Low probability, 4-5: Intermediate probability, 6-8: High probability • Patients with intermediate or high pretest probability for HIT should be treated Stop heparin/heparin products Heparin cessation alone is often not sufficient, since these patients remain at risk for subsequent thrombosis a direct thrombin inhibitor lepirudin (caution in renal disease), bivalirudin, or argatroban (caution in liver disease); fondaparinux Warfarin should be initiated after pt stable and platelet count has increased to ≥150,000 Overlap VKA and thrombin inhibitors x 5 days VKA at least 2-3 months Low-molecular-weight (LMW) heparin, the heparin analogue fondaparinux, and heparinoids, such as danaparoid, are associated with a much lower incidence of HIT Use UFH with care or the substitution of LMWH when appropriate Limiting heparin duration to <5 days and initiating coumgain early to minimize heparin use is also a strategy in those requiring long-term anticoagulation Diagnosis is based on history, PE, CBC and examination of the peripheral smear to exclude other causes History Bleeding symptoms: type of bleeding, severity, duration, prior surgery history, pregnancies Systemic symptoms: weight loss, fever, HA, symptoms of autoimmune disorders Risk factors for HIV Pregnancy status Medications: heparin, EtOH, quinidine, sulfonamides, ASA Transfusion history Family history Comorbid conditions that may increase risk of bleeding Lifestyle: vigorous or traumatic activities Physical exam Bleeding signs Type and severity Liver, spleen, lymph nodes; jaundice and other stigmata of liver disease Evidence of infection Evidence for autoimmune disease Evidence for thrombosis Neurologic function Skeletal abnormalities Laboratory data CBC with examination of a peripheral blood smear HIV Bone Marrow biopsy in those over 60 years old and in patients considering splenectomy TSH Platelet count >20K should not be hospitalized if they are asymtpmatic or have minor purpura Platelets >50K do not routinely require treatment Treatment is indicated with platelets <20-30,ooo and those with counts <50K and significant bleeding or risk factors for bleeding Glucocorticoids are the initial treatment Those with severe, life-threatening bleeding should also be hospitalized and should receive supportive care along with treatment for ITP Regimens for treatment include high-dose glucocorticoid therapy, IVIG and platelet transfusions Splenectomy is appropriate in specific situations such as bleeding symptoms if platelets remain below 30K after 4-6 weeks of medical treatment 60-year-old white male presented with a 4-day history of bleeding from the gums, diffuse spontaneous ecchymoses, mild fatigue, and bone pain. The patient described a 6-month history of pain localized to his right thigh with extension to the posterior part of his right leg. Pt sent from an OSH for an abnormal peripheral smear. PMH: atrial fibrillation, hypercholesterolemia, and hypertension PSH: appy Social: no tobacco; moderate alcohol consumption until 1 year ago. Meds: ASA 325mg daily, metoprolol 50mg bid, simvastatin 40mg daily, HCTZ 25mg daily Physical: BP 138/64, P 57, T 98, RR 18 HEENT: dry blood in oropharynx Pulm: CTA Abdomen: liver and the spleen were not palpable. BLE: confluent ecchymoses involving the left ankle, B thighs posteriorly Laboratory values: Hb 13.4, platelets 107K, leukocytes 8.1, LFTs normal, creatinine normal, PTT 45, INR 1.92, fibrinogen <0.30 g/L, D-dimers >4 μg/mL (normal:≤0.40 μg/mL). Normal factors V, VII, XIII, and activated protein C Initial OSH Smear: consistent with a normochromic, normocytic anemia, with reduced platelets and large forms, and possible blasts with folded nuclei OSH PSA returns 2 days after admission at 276 27-year-old woman is evaluated in the ER for a two-day history of HA, fatigue and gingival bleeding on brushing her teeth. She is otherwise healthy. Her only medication is an oral contraceptive, and medical and family histories are unremarkable. Physical: T 98.6, HR 65, BP 110/65, RR 18, SaO2 98% General: alert and oriented but reports having a headache. HEENT: Funduscopic examination is normal. There are a few scleral hemorrhages, and mild icterus is noted. Skin: Petechiae that had gone unnoticed by the patient are visible on the lower extremities. Laboratory studies: Hb 8 g/dL; platelet count of 34,000/µL; reticulocyte count of 12% of erythrocytes INR 1.1, aPTT 32 LDH 2000 creatinine 0.8 D-dimer negative George JN, et al. Idiopathic thrombocytopenic purpura: a practice guideline developed by explicit methods for the American Society of Hematology. Blood. 88(1):3-40, 1996 Jul 1. Allford SL. Hunt BJ. Rose P. Machin SJ. Haemostasis and Thrombosis Task Force, British Committee for Standards in Haematology. Guidelines on the diagnosis and management of the thrombotic microangiopathic haemolytic anaemias. British Journal of Haematology. 120(4):556-73, 2003 Feb. Warkentin TE., et al. Heparin-induced thrombocytopenia: recognition, treatment, and prevention: the Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest 2008: 133; 340S-380S. Levi M, Toh CH, Thachil J, Watson HG. Guidelines for the diagnosis and management of disseminated intravascular coagulation. British Committee for Standards in Haematology. Br J Haematol 2009 Apr;145(1):24-33. MKSAP 15 UpToDate