ONLINE SUPPLEMENT
advertisement

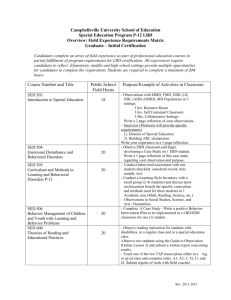
1 U U Supplemental Methods Treadmill training Wistar rats (Charles River, Saint-Constant, QC, Canada) were randomly assigned to sedentary (Sed) or intensive-exercise (Ex) groups. The exercise program has been previously described (1). Ex-rats underwent daily running training sessions on a treadmill. The treadmill had different lanes to serve as corridors for each animal and had a grid in the back that administered a small electric shock on contact to ensure that animals ran effectively. The electric shock was sufficient to encourage the animal to run without being harmful. The protocol included a 1-week progressive training program, starting with a 10-minute running session at 6 m/min and increasing gradually to steady-state 60-minute running at 28 m/min. Thereafter, animals were trained at this level 5 days a week for 8 or 16 weeks. Investigators observed all treadmill sessions to ensure effective running, and applied a semiquantitative scoring system (0-5) every 5 minutes to evaluate the quality of all training sessions of each rat (supplemental Figure 1A). Only rats that mastered the running training (rats that never had an average score <3.6 for 3 consecutive days) were included, thus confining the study to skillful endurance runners and avoiding inclusion of rats receiving multiple electrical shocks. A subgroup of rats in both the Sed and Ex group, underwent discontinuation of exercise for 4 weeks (DEx4) or 8 weeks (DEx8) after the initial 16 week-period, or prolongation of the sedentary period for parallel durations. Sed-rats were housed and fed in the same conditions as Ex-rats. Animals were euthanized 3 days after the last training session to avoid acute responses to exercise. Hearts were processed according to experimental needs (fixed in formalin for 2 histological studies, snap-frozen in liquid nitrogen for molecular biology experiments or retrogradely perfused for myocyte isolation). Distress assessment Physical and psychological distress might act as a confounding factor by inducing stress-related cardiac structural changes. Therefore, we compared the distress level in Sed and Ex groups by means of a previously described and validated scoring system (2,3). One experienced investigator, blind to group assignment and not otherwise linked to the study, evaluated Sed and Ex rats both in the chronic (at least 18 hours after a training session) and in the acute setting (one hour after a training session). Seven items were assessed and scored from 0 to 2 or 3 (depending on the item, where a higher score means more distressed). The final score for each rat was the sum of all individual items. All rats were assessed at least twice in each setting, and results averaged. Overall, no distress differences were detected between Sed and Ex groups (Supplemental Figure 1B). U Echocardiography Repeated transthoracic echocardiographic studies were performed in Sed and Ex groups in two different sets of animals: a training-evolution set (baseline, 8 weeks, and 16 weeks) and a detraining set (16 week-exercise, DEx4 and DEx8). Before echocardiography studies, rats in the Ex-group remained a minimum of 12 hours at rest to avoid changes induced by acute exercise. Procedures were performed under general anesthesia with 2%-isoflurane, using a phased-array probe 10S (4.5-11.5 Megaherz) in a Vivid 7 Dimension system (GE Healthcare Ultrasound, Horten, Norway). When the M-mode spectrum was traced in parasternal long axis view at the 3 level of the aortic valve, left atrial dimension at end-atrial systole (LADs) and at end-diastole (LADd), right atrial dimension at end-diastole (RADd) and right ventricular (RV) dimension (RVD) and wall thickness (RVWT) at end-cardiac diastole were measured. The M-mode spectrum was also obtained in parasternal short axis view at the level of papillary muscles, and left ventricular (LV) dimensions at both end-cardiac diastole (LVDd) and systole (LVDs) were measured. The thickness of LV anterior wall and the LV posterior wall at end-diastole were also measured in this view. Since animals differed in size during the study, all dimensions were indexed for body weight. Raw, non-indexed data are also shown for atrial measurement in the first set of rats (measurements at baseline, 8 weeks and 16 weeks time-points). LV mass was calculated and corrected using the formula suggested for small animals by Reffelmann et al. (4) LV ejection fraction (EF) was calculated using the formula packed in the Vivid 7 system ((LVDd-LVDs)/LVDd*100). Tricuspid annulus plane systolic excursion (TAPSE) was measured by M-mode echocardiography in an apical 4 chamber view. Continuous-wave Doppler at the conjunction of LV inflow and outflow was recorded in apical 5-chamber view, LV isovolumic relaxation time (IVRT) was measured, and corrected (IVRTc) by R-R intervals taken from simultaneously recorded ECGs (5) The average of 3 consecutive cardiac cycles was used for each measurement, with the operator being blinded to exercise or sedentary group-assignment. Special care was taken to use similar imaging-planes at follow-up studies in each rat. U Electrophysiological testing 4 A subgroup of rats at 8 weeks, 16 weeks, DEx4 and DEx8 time-points underwent in vivo electrophysiological study (EPS). The procedure was performed under general anesthesia with 2%-isoflurane. The distal dipole of a 1.9F octapolar electrode catheter (Scisense, London, ON, Canada) was placed into the right atrium through a right internal jugular vein. Surface ECG (lead II) and intracardiac electrograms were processed with an analog-digital converter and stored in a computer (IOX 2.5.1.6, EMKA Technologies, Paris, France) for later offline analysis (ECG Auto 2.5.1.26, EMKA Technologies, Paris, France). Pacing was carried out with an impulse generator (Grass Technologies, RI, United States) triggered by custom-made software. To assess Wenckebach cycle length (WBCL), consecutive steps of 10-beat train stimuli were administered. Cycle length (CL) was reduced by 2 ms at each step until atrioventricular (AV) block was observed. The longest CL inducing Mobitz type-1 AV-block constituted the WBCL. Atrial arrhythmia inducibility was tested with double and triple extrastimulation to a minimal coupling interval of 20 ms during spontaneous sinus rhythm and following a 9-beat atrial-pacing train at a CL of 150 ms. Atrial burst pacing trains at 60 and 40 ms CL were applied for 7.5, 15 and 30 seconds if sustained AF was not induced by extrastimuli. AF was defined by >1-second irregular atrial electrograms at ≥800 bpm with irregular ventricular response. AF was considered non-sustained when it lasted between 1 and 30 seconds, sustained when lasting more than 30 seconds, and long-lasting when >15 minutes. When long-lasting AF was induced, parasympathetic block was produced with intraperitoneal atropine injection (2 mg/kg). If no sustained AF was induced, 25 µg/kg of carbachol was injected intraperitoneally, and the AFinducibility determination was repeated 10 minutes later. If no sustained AF was induced, an 5 additional 25 µg/kg of carbachol (total dose of 50 µg/kg) was administered and the AFinducibility determination was again repeated. Because of the short refractory period in rats, particular attention is needed to obtain accurate values and detect changes. Atrial refractoriness was therefore specifically tested in a set of trained and sedentary rats at 16 weeks. All tests were performed between 10 am and 2 pm to account for circadian oscillation in autonomic tone. Body temperature was strictly maintained between 36.9ºC and 37.4ºC. Refractory period was tested through programmed right-atrial stimulation with a 9-beat train (S1, cycle length 150 ms) followed by an extrastimulus (S2) that was decreased 1 ms per step until refractoriness. Atrial effective refractory period was defined as the longest coupling interval failing to produce a propagated atrial response. U Surgical procedures All surgical procedures were performed under 2%-isoflurane anesthesia. Experiments were performed at least 48 hours after surgery to avoid contamination by acute effects of surgery. U ECG transducer : Through a small abdominal incision, an ECG transducer was inserted and U sutured to the abdominal musculature. ECG leads 1 and 3 were derived from subcutaneous electrodes. ECG signals were monitored in the conscious state by telemetry and sampled at 500 Hz. U Blood pressure transducer : The retroperitoneum was accessed through an abdominal incision U and abdominal aorta dissected and exposed. During a brief (<30 seconds) blood-flow suspension, the descending aorta was cannulated and the aortic incision was sealed with 6 biological glue and cellulose paper. The transducer was sutured in the inner abdominal wall. Blood pressure recordings were sampled at 500 Hz. U Indwelling catheter implantation (Port-a-cath) : An incision was made in the right side of the U anterior aspect of the neck. The right jugular vein was dissected and cannulated with permeable tubing designed for repeated drug-administration to rats in the conscious nonsedated state. Permeability was ensured and tubing was subcutaneously diverted to the back, where it was extruded and connected to a harness. U Telemetry recordings In a subgroup of 15 rats (8 Ex, 7 Sed), a consecutive 24 hour ECG recording was obtained at baseline, 8 weeks, 16 weeks, DEx4 and DEx8, and stored in a computer (IOX 2.5.1.6, EMKA Technologies, Paris, France). Recording was initiated at 2 pm; the dark-phase cycle was established between 6 pm and 6 am, with 6 am to 6 pm comprising the light-phase cycle. All analyses were performed offline (ECG Auto 2.5.1.26, EMKA Technologies, Paris, France). Through a semi-automatic QRS recognition software (ECG Auto 2.5.1.26, EMKA Technologies, Paris, France), all RR intervals were recorded; mean RR per hour per group was calculated at each time-point. Results were plotted for one-hour periods; periods with analyzable data from under 95% of the time were excluded. Telemetry recordings were also used to assess spontaneous arrhythmic events in Sed and Ex groups. An experienced researcher manually reviewed all recordings, looking for AF or atrial tachycardia episodes. Furthermore, a period of 10 minutes of each hour (from minutes 25 to 35) of all recordings was automatically scanned for consecutive RR variations > 15%, in search of 7 isolated premature atrial complexes (PACs). All automatically selected beats were subsequently reviewed manually, and those with early, non-sinusal P-wave morphology were counted as PACs. Results are shown as number of PACs per 100,000 beats. Autonomic tone assessment Autonomic tone components (reflecting parasympathetic and sympathetic tone) were assessed by mean of heart rate changes to sequential pharmacological blockade. All animals underwent procedures to evaluate both parasympathetic and sympathetic tone indices in random order within 24 hours. Experiments were performed in awake, unrestrained rats in which ECG transducers and port-a-cath devices had been implanted. To study the time course of the effects of both drugs used for this analysis, single doses of propranolol (2 mg/kg) or atropine (1 mg/kg) were administered at separate occasions in a subgroup of three rats. Heart rate was stored and measured offline at different time-points (baseline, 15 sec, 30 sec, 45 sec, 60 sec, 2 min, 3 min, 5 min, 10 min, 20 min, 30 min, 40 min, 50 min, 60 min and 70 min) (Supplemental Figure 2A). Atropine reached maximal effect 45 seconds after injection, and effects were maintained for 30 minutes. Propranolol showed a slightly more gradual action, requiring 1 minute to reach maximal effect, with effect maintained for 50 minutes. On this basis, we decided that later experiments should be completed no later than 15 minutes after the first drug injection in order to allow for simultaneous effect of both drugs, and a 5 to 7 minute delay between drugs was chosen. To estimate parasympathetic tone, propranolol (2 mg/kg) was administrated intravenously; 5 to 7 minutes later, parasympathetic effects were blocked with atropine (1 mg/kg). The parasympathetic tone index was defined as the difference between heart rate 8 after propranolol and heart rate after propranolol+atropine (Supplemental Figure 2B, upper panel). Conversely, to estimate sympathetic tone, atropine (1 mg/kg) was administrated intravenously; 5 to 7 minutes later, sympathetic effects were blocked with propranolol (2 mg/kg). The sympathetic tone index was defined as the difference between heart rate after atropine and heart rate after atropine+propranolol (Supplemental Figure 2B, lower panel). Baroreflex sensitivity (BR) testing was used to evaluate reflex control of parasympathetic/sympathetic tone. In rats with an ECG transducer, an implanted arterial bloodpressure transducer and a chronically indwelling venous catheter, progressively increasing doses of phenylephrine (Phe, 1, 2, 4, 8 and 16 µg/kg) and nitroprusside (NTP, 0.5, 1, 2, 4 and 8 µg/kg) were used to raise and lower blood pressure, respectively. Maximum changes in mean blood pressure and heart rate (assessed by CL) for each dose were determined (Supplemental Figure 3) and plotted against each other. Effects of NTP and Phe were analyzed separately. Regression lines were fitted to the data for each animal (Figure 5A). Mean slopes of regression lines were then compared between Ex and Sed groups as an index of baroreflex sensitivity. 9 Fibrosis quantification Fibrosis was quantified in histological samples from both atria by mean of picrosirius-red staining, as previously described (1). Six to 10 slides were obtained in each animal. Representative atrial photomicrographs covering the whole section were obtained with an Olympus BX60 microscope and a QI-maging Q-cam, and quantified with an automated color recognition processing software (ImageJ, U.S. National Institutes of Health, Bethesda, Maryland, USA). Perivascular, pericardial and endocardial collagen was excluded from measurements. Results were calculated as a percentage of total tissue cross-sectional area. Analyses were blinded to investigative-group for each animal. Cardiomyocyte isolation Atrial myocytes were enzymatically isolated in a Langendorff apparatus. Rats were anesthetized with intraperitoneal ketamine (100 mk/kg) and xylazine (10 mg/kg), and treated with heparin (1 mg/kg body-weight). Hearts were rapidly excised and immersed in ice-cold Tyrode solution (NaCl 140 mmol/L, KCl 5.5 mmol/L, MgCl 2 1 mmol/L, HEPES 5 mmol/L, KH 2 PO 4 0.3 B B B B B B mmol/L, dextrose 10 mmol/L; pH adjusted to 7.5 with NaOH) with 2 mmol/L CaCl 2 . The aorta B B was cannulated and the heart retrogradely perfused in situ with Tyrode solution containing 200-μmol/L Ca 2+ . The solution was then switched to Ca 2+ -free Tyrode solution until the heart P P P P stopped beating. Collagenase was then added (collagenase type-II 0.5 mg/mL) for about 50 minutes. Atria were then removed, placed in KB solution (KCl 20 mmol/L, KH 2 PO 4 B B B B 10 mmol/L, glucose 10 mmol/L, mannitol 40 mmol/L, albumin 0.1%, L-glutamic acid 70 mmol/L, β-hydroxybutyric acid 10 mmol/L, taurine 20 mmol/L, EGTA 10 mmol/L), minced 10 in small pieces and cells gently collected. Cells were stored at room temperature until use, within 6 hours after collection. I KACh measurement B B Ionic-current recordings were obtained at 37°C with the whole-cell tight seal patch clamp technique. Borosilicate glass electrodes (Sutter Instrument) filled with pipette solution were connected to a patch-clamp amplifier (Axopatch 200A, Axon). Electrodes had tip resistances of 2 to 5 MΩ when filled. Currents were elicited with 500-millisecond pulses from a holding potential of -40 mV to voltages ranging from -120 to +20 mV, and are expressed as densities (pA/pF). I KACh was obtained by subtraction of the current obtained after the application of B B carbachol (10 nmol/L, 100 nmol/L, 1 µmol/L, 10 µmol/L) from baseline values. Currents were elicited with 500-millisecond pulses from a holding potential of -40 mV to voltages ranging from -120 to +20 mV. The internal solution for K + -current recording contained (in mmol/L) potassium-aspartate P P 110, KCl 20, MgCl 2 1, MgATP 5, Li-GTP 0.1, HEPES 10, sodium-phosphocreatine 5, and B B EGTA 5.0, titrated to pH 7.3 with KOH. Concentration-response curves were constructed with the I KACh current density at -120 mV at 10 nmol/L, 100 nmol/L and 1 µmol/L carbachol B B concentrations. In each group, a curve was determined to fit an equation of the form: Y = T Min + (Range/(1+10 LogEC50-x )), in which Y=change in current; Min=minimum response plateau; P P T Range=difference between minimum and maximal effect plateau; EC50=concentration of carbachol that induces a 50%-maximal I KACh response; x=carbachol concentration. TimeB B dependent increases in IKACh were fitted by a mono-exponential equation, and the mean timeconstants in the Sed and Ex groups were compared. 11 mRNA quantification RNA isolation and generation of cDNA Frozen atrial samples were homogenized and total RNA was isolated from the tissue using Trizol. Following RNA purification, RNA was quantified using a Nanodrop ND-100 Spectrophotometer. DNAse I (Sigma, USA) treatment was performed and lack of genomic DNA-contamination was confirmed by PCR. The quality of total RNA was assessed with polyacrylamide-gel micro-electrophoresis (Agilent 2100 Bioanalyzer, Agilent Technologies, USA). RNAs with a RIN number above 7.5 were used for gene-expression analysis. TaqMan low-density arrays TaqMan low-density arrays (TLDAs, Applied Biosystems, USA) were used in a two-step RT-PCR process as previously reported (6). First-strand cDNA was synthesized from 420 ng of total RNA using the High-Capacity cDNA Archive Kit (Applied Biosystems) with random hexamer primers. PCR reactions were then performed on TaqMan low-density arrays using the ABI PRISM 7900HT Fast Real-Time PCR System (Applied Biosystems). Thermal profile for the PCR reactions was: 2 min 50°C; 10 min 95°C; and 40 cycles with 30 sec 95°C, 1 min 60°C. The wells of each TLDA were pre-loaded with pre-designed fluorogenic TaqMan probes and primers. Data were collected with instrument spectral compensation and Applied Biosystems SDS 2.3 software and grouped, with RQ Manager software. GAPDH was selected as the reference gene, and the ΔCt method (7) was applied to determine the mRNA expression level. The outliers (a maximum of one value per group) were excluded using Dixon’s Q test. 12 RGS4 knockout model Animals The Rgs4 knockout mouse (Rgs4tm1Dge1/J) strain, backcrossed onto a C57Bl/6 background, was obtained from The Jackson Laboratory (Bar Harbor, Maine). Details of its construction may be found at http://jaxmice.jax.org/strain/005833.html. Wild type littermates were used for comparison to rgs4-/- mice in all experiments. Atrial fibrillation inducibility Electrocardiogram (ECG), intracardiac ECG (iECG) and atrial tachypacing protocols were performed as described previously (8). Briefly, 16- to 20-week old male mice were anaesthetized with 1% isoflurane inhalation. Surface two-lead ECG was recorded from subcutaneous 25-gauge electrodes. ECG was recorded with a Gould ACQ-7700 differential amplifier, digitized at 1 msec, using the Ponemah software package (DSI, St. Paul, Minnesota). A 2F octapolar catheter (CIBer Mouse EPO Catheter, NuMed Inc., Hopkinton, New York) was inserted through the right jugular vein into the right ventricle. The distal electrodes were used to record from the right ventricle, while the proximal electrodes were used for both pacing and recording from the right atrium. Right atrial burst pacing (15-20 pulses) at pulse intervals ranging from 10 to 40 ms were performed in an attempt to induce atrial arrhythmias. Triple extrastimuli down to a minimal coupling interval of 20 ms were also added if the burst pacing protocol did not induce an arrhythmia. Three induction attempts were performed at baseline and following 10 µg/kg carbachol (ip). If no arrhythmias were observed, an additional three attempts were made following 30 µg/kg carbachol (ip). The ECG channels were amplified and filtered 13 between 0.5 and 250 Hz. High fidelity intracardiac electrogram signals were filtered between 5 and 400 Hz and acquired at a sampling rate of 1000 Hz. All experiments were performed with the experimenter blinded to the genotype of the individual mice. Statistical analysis Data for continuous variables is expressed as mean±SEM. Normal distribution was assessed with Shapiro-Wilks test. Statistical analysis was generally performed by fitting data into a linear mixed effects model (MIXED procedure), in which main factors and all their possible interactions were introduced. When significant interaction was found, pairwise comparisons were performed within each value of a significant main factor. In the absence of interaction but with a significant main factor effect, post-hoc comparisons between groups in the main effect were carried out. Post-hoc comparisons were executed with LSD (least significant differences) test; please note that LSD does not correct for multiple post-hoc comparisons. For repeated measure analyses, covariance matrix structure was chosen amongst compound symmetry, Toeplitz, autoregressive (AR1) and unstructured based on the lowest Akaike’s Information Criterion (AIC). Statistical analyses were carried out with SPSS 19.0 (IBM, Armonk, NY, USA) and GraphPad 5.0 (La Jolla, CA, USA). RT-PCR results did not follow a normal distribution and were analyzed with non-parametric Mann-Whitney U test. Frequency variables were compared with χ 2 or Fisher’s exact test. A p<0.05 was considered significant. P P Detailed statistical analysis description for each figure follows: Figure 1B: A Fisher exact test test was applied to compare AF-inducibility between Sed and Ex P groups at each time-point (8 weeks and 16 weeks). 14 Figure 1C: A Fisher’s exact test was applied to compare AF-inducibility between Sed and Ex groups. Figure 2A, 2B and 2E: A linear mixed effects model was applied, including hour (24 hours for each study-day) and time-point (baseline, 8 weeks, 16 weeks, DEx4 and DEx8) as repeated factors, group (Sed, Ex) as a non-repeated factor, and all the interaction terms (hour x time-point, hour x group, time-point x group, hour x time-point x group). No overall (hour x time-point x group) significant interaction was found. Significant interaction was found for the group x time-point and time-point x hour interactions at the 0.001 level; pairwise comparisons within group factor (Sed vs Ex) are shown at each time-point. Figure 2C and 2D: The 8-week time-point, and the 16-week, DEx4 and DEx8 results were obtained in one set of rats each. For the 8-week time-point, Sed and Ex groups were compared with an unpaired t-test. A linear mixed model analysis of variance was applied for the 16-week, DEx4 and DEx8 (repeated-measures data), as the results were obtained in single sets of rats. This analysis included time-point (16-week, DEx4 and DEx8) as a repeated factor, group (Sed, Ex) as a non-repeated factor and the interaction tern (time-point x group). Significant interaction was found for parasympathetic tone (Figure 2C) at the 0.05 level, and pairwise comparisons (Sed vs Ex) are shown at each time-point. No differences were found for sympathetic tone (Figure 2D). Figure 3A: A linear mixed-effects model was applied, including time-point (Baseline, 8-wk, 16-week) as a repeated factor, group (Sed, Ex) as a non-repeated factor and the interaction term (atria x group). For diastolic LA dimensions (upper panel), significant interaction was found at the 0.05 level and pairwise comparisons (Sed vs Ex) are shown within each time-point. For the LA systolic and RA diameter, no significant differences were found. 15 Figure 3B: A linear mixed-effects model was applied, including time-point (Baseline, 8-wk, 16-week) as a repeated factor, group (Sed, Ex) as a non-repeated factor and the interaction term (time-point x group). For diastolic and systolic LA dimensions (upper and center panel), significant interaction was found at the 0.01 level and pairwise comparisons (Sed vs Ex) are shown within each time-point. For RA-diameter, a significant group main effect at the 0.01 level, and time-point main effect at the 0.001 level, without interaction, were found. Figure 3D: A linear mixed-effects model was applied, including atria (right, left) as a repeated factor, group (Sed, Ex) as a non-repeated factor and the interaction term (atria x group). Significant effect was found for group (Sed, Ex) factor, without significant interaction. Figure 4A: A χ 2 test was applied to compare AF-inducibility between Sed and Ex groups at P P DEx4 and DEx8 time-points. No significant differences were found. Figure 4B: A linear mixed effects model was applied, including time-point (DEx4, DEx8) and group (Sed, Ex) as non-repeated factors, and the interaction term (time-point x group). Significant difference was found for group main effect, without significant interaction. Figure 4C: A linear mixed-effects model, including time-point (16-week, DEx4 and DEx8) as a repeated factor, group (Sed, Ex) as a non-repeated factor and the interaction term (dose x group) was used. No significant interaction was found for either diastolic or systolic left atrial dimensions (left and center panel), but a significant group effect was found. Significant interaction was found at the 0.05 level for right-atrial diameter, and pairwise comparisons within group factor (Sed, Ex) are shown at each time-point. Figure 5B: A linear mixed-effects model was applied separately for bradycardic (phenylephrine, PE) and tachycardic (nitroprusside, NTP) responses. Results at each time-point were obtained in different sets of rats, so time-point (8-week, 16-week, DEx4 and DEx8) and group (Sed, Ex) 16 were included as non-repeated factors, as well as the interaction term (time-point x group). For the bradycardic response, the interaction factor was found to be significant at the 0.05 level. Pairwise comparisons for group factor (Sed vs Ex) are shown at each time-point. No differences were found for the tachycardic response. Figure 6A: Pairwise comparisons between Sed and Ex groups were carried out with unpaired t-test. Figure 6B: Amplitude of I KACh was plotted as a function of carbachol concentration to define the B B concentration-response curve. Least square difference fitting method was applied to build a curve with three parameters (maximum, minimum, EC50). Figure 6C: A non-parametric Mann-Whitney U-test was performed to compare mRNA expression between 16-week Sed and Ex groups for Kir3.1 and Kir3.4. Figure 7A: Non-parametric Mann-Whitney U-test was used to compare mRNA results between Sed and Ex groups for each gene. Figure 7D: Pairwise comparisons (WT vs KO) of AF inducibility-rates were carried out with a Fisher’s exact test. Supplemental Table 1: Unpaired t-test was used to compare ECG parameters between Sed and Ex groups for each electrophysiological parameter. Supplemental Table 2: A linear mixed-effects model was applied including time-point (baseline, 8 weeks and 16 weeks) as a repeated factor, group (Sed, Ex) as a non-repeated factor and the interaction term (time-point x group). Significant interaction was found for LVDd, LVSd, LV PW, IVS, LV mass, LVEF, IVRTc, RV WT, TAPSE, LADd and LADs and pairwise comparisons (Sed vs Ex) are shown within each time-point. Significant group effect (Sed vs Ex) without interaction was found for RAD. 17 Supplemental Table 3: A linear mixed-effects model was applied including time-point (16 weeks, DEx4 and DEx8) as a repeated factor, group (Sed, Ex) as a non-repeated factor and the interaction term (time-point x group). Significant interaction was found for LVDd, IVS, IVRTc, RVD, TAPSE, and RAD and pairwise comparisons (Sed vs Ex) are shown within each time-point. Significant group effect (Sed vs Ex) without interaction was found for LVSd, LV PW, LV mass, LVEF, RV WT, LADd and LADs. Supplemental Figure 1B: Unpaired t-test was applied to compare Sed and Ex groups at each of chronic and acute setting. Supplemental Figure 2: A one-way analysis of variance was separately applied to atropine and propranolol experiments. Both were significant at the 0.001 level. Post-hoc analyses with LSD test were used to compare heart rate at each time-point to heart rate at baseline. Supplemental Figure 5B: A Fisher exact test was applied to compare the proportion of inducible rats at each carbachol dose (baseline, CCh25, CCh50) in both groups (Sed, Ex). All AF episodes (including sustained and non-sustained AF episodes) and sustained AF episodes were analyzed separately. Supplemental Figure 6A: Pairwise comparisons between Sed and Ex groups were carried out with unpaired t-tests. Supplemental Figure 6B: For each carbachol dose, pairwise comparisons between Sed and Ex groups were carried out with unpaired t-tests. Supplemental Figure 7: Non-parametric Mann-Whitney U-test was used to compare mRNA results between Sed and Ex groups for each gene. Supplemental Figure 8: Pairwise comparisons between Ex rats with long-lasting AF (>15 min) and Ex rats with AF lasting <15 min for heart rate (A) and echocardiographic parameters (F) 18 were carried out with unpaired t-tests. mRNA expression (B-E) values were compared with non-parametric Mann-Whitney U-test. 19 References 1. Benito B, Gay-Jordi G, Serrano-Mollar A, et al. Cardiac arrhythmogenic remodeling in a rat model of long-term intensive exercise training. Circulation 2011;123:13-22. 2. Lloyd MH, Wolfensohn SE. Practical use of distress scoring systems in the application of humane end points.In Hendriksen C.F.M. and Morton D.B.(eds), Humane Endpoints in Animal Experiments for Biomedical Research: "Proceedings of the International Conference, 22-25 November 1998,Zeist, The"Netherlands. Royal Society for Medicine Press Ltd., London, pp 48-53. 1999. 3. Morton DB, Griffiths PH. Guidelines on the recognition of pain, distress and discomfort in experimental animals and an hypothesis for assessment. Vet Rec 1985;116:431-6. 4. Reffelmann T, Kloner RA. Transthoracic echocardiography in rats. Evalution of commonly used indices of left ventricular dimensions, contractile performance, and hypertrophy in a genetic model of hypertrophic heart failure (SHHF-Mcc-facp-Rats) in comparison with Wistar rats during aging. Basic Res Cardiol 2003;98:275-84. 5. Shi Y, Denault AY, Couture P, Butnaru A, Carrier M, Tardif JC. Biventricular diastolic filling patterns after coronary artery bypass graft surgery. J Thorac Cardiovasc Surg 2006;131:1080-6. 6. Gaborit N, Le BS, Szuts V, et al. Regional and tissue specific transcript signatures of ion channel genes in the non-diseased human heart. J Physiol 2007;582:675-93. 7. Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 2001;25:402-8. 8. Kovoor P, Wickman K, Maguire CT, et al. Evaluation of the role of IKACh in atrial fibrillation using a mouse knockout model. J Am Coll Cardiol 2001;37:2136-43. 20 Supplemental Tables Supplemental Table 1. ECG and EP parameters 8 weeks Parameter 16 weeks DEx4 DEx8 Sed (n=9) Ex (n=8) Sed (n=20) Ex (n=14) Sed (n=20) Ex (n=8) Sed (n=12) Ex (n=7) PR 53±2 53±3 51±1 53±1 60±1 57±2 66±2 61±2 Pdur 23±1 23±1 21±1 22±1 21±0.1 20±0.2 22±0.3 22±0.4 QRS 22±1 21±1 22±1 22±1 21±0.1 20±0.4 22±0.3 22±0.4 QTc 187±10 183±8 205±3 214±4 176±5 175±4 189±7 192±11 WBCL 127±5 120±3 121±3 139±4** 112±2 113±7 126±4 117±4 SCL 187±4 200±8 195±4 223±6*** 185±4 190±11 210±5 200±7 ECG (ms) EP study (ms) AF inducibility (%) SAF 1/9 (11%) 2/8 (25%) 3/20 (15%) 9/14 (64%)** 0/20 (0%) 1/8 (12%) 1/12 (8%) 0/7 (0%) All AF 3/9 (33%) 3/8 (38%) 8/20 (40%) 14/14 (100%)*** 9/20 (45%) 5/8 (63%) 4/12 (33%) 3/7 (43%) ECG intervals and EPS measurements at 8 weeks, 16 weeks, DEx4 and DEx8 time-points. Comparisons with non-paired t-test, except for inducibility (Fisher exact test). Pdur: P wave duration; QTc: Bazett’s corrected QT interval; WBCL: Wenckebach cycle length; SCL: sinus cycle length; SAF: sustained atrial fibrillation; All AF: includes non-sustained and sustained AF episodes. *p<0.01**p<0.01; ***p<0.001. 21 Supplemental Table 2. Evolution of echocardiographic parameters (normalized to body-weight) with exercise training Baseline 8 weeks 16 weeks Sed (n=19) Ex (n=20) Sed (n=18) Ex (n=17) Sed (n=17) Ex (n=16) 3.15±0.09 3.11±0.06 1.55±0.04 1.71±0.02* 1.35±0.04 1.66±0.03*** 1.48±0.07 1.48±0.04 0.76±0.03 0.87±0.03 0.69±0.03 0.94±0.03*** 0.57±0.01 0.57±0.02 0.29±0.01 0.35±0.01*** 0.26±0.01 0.33±0.01*** 0.57±0.01 0.58±0.02 0.31±0.01 0.38±0.01*** 0.28±0.01 0.36±0.01*** 2.65±0.07 2.75±0.06 1.87±0.04 2.13±0.04** 1.72±0.05 2.18±0.07*** LVEF (%) 87.58±1.03 86.87±1.07 86.22±0.68 84.41±1.29 84.15±1.04 79.78±1.17*** IVRTc (ms) 1.12±0.05 1.09±0.03 1.18±0.04 1.47±0.06*** 1.25±0.04 1.45±0.05** 1.3±0.04 1.3±0.04 0.66±0.02 0.72±0.02 0.58±0.02 0.68±0.02 1.07±0.028 1.03±0.028 0.54±0.11 0.65±0.011 0.59±0.008 0.72±0.012* 2.76±0.01 3.10±0.11 3.57±0.10 3.58±0.09 3.68±0.10 3.45±0.09 1.94±0.06 1.94±0.04 0.97±0.03 1.13±0.02** 0.86±0.03 1.17±0.03*** 1.38±0.06 1.33±0.04 0.69±0.02 0.71±0.03 0.61±0.02 0.77±0.02** LV measurements LVDd (mm/kg) + P LVSd (mm/kg) + P P P LVPW (mm/kg) + P IVS (mm/kg) + P P LV mass (g/kg) + P P P LV function RV dimensions RVD (mm/kg) + P P RVWT(mm/kg) + P P RV function TAPSE (mm) Left atrium LADd (mm/kg) + P LADs (mm/kg) + P P P 22 Right atrium RAD (mm/kg) + ### P P 2.22±0.07 2.28±0.1 1.05±0.04 1.17±0.02 0.97±0.04 1.15±0.03 Significant interaction was found for LVDd, LVSd, IVS, LVPW, LV mass, LVEF, IVRTc, RV WT, LADs and LADd, and pairwise comparisons (Sed vs Ex) are shown within each time-point. Significant group main effect was found for RAD without interaction and overall significance for Sed vs Ex is shown. LVDd: left ventricle end-diastolic diameter; LVSd: left ventricle end-systolic diameter; LVPW: left ventricle posterior wall thickness; IVS: interventricular septum thickness; LVEF: left ventricular ejection fraction; IVRTc: isovolumetric relaxation time corrected by RR interval; RVD: right ventricular diameter; RVWT: right ventricular wall thickness; TAPSE: tricuspid annular plane systolic excursion; DT: deceleration time; LADd: left atrial diameter in atrial diastole; LADs: left atrial diameter in atrial systole; RAD: right atrial diameter. *p<0.05, **p<0.01, ***p<0.001 Sed vs Ex. ### p<0.001 Sed vs Ex (group effect). + P P Values for chamber dimensions, LV wall thickness and LV mass, are normalized to body weight; therefore values at baseline are much greater than at 8- and 16-week exercise. NB. The results in Supplemental Table 2 are for a distinct group of rats from those in Supplemental Table 3; having been studied repeatedly at baseline, 8-week and 16-week Ex. 23 Supplemental Table 3. Evolution of echocardiographic parameters during detraining 16 weeks Sed (n=15) DEx4 DEx8 Ex (n=10) Sed (n=15) Ex (n=10) Sed (n=10) Ex (n=6) 1.16±0.03 1.51±0.03*** 1.23±0.04 1.42±0.07** 1.19±0.04 1.33±0.07 LVSd (mm/kg) + ### 0.53±0.03 0.75±0.03 0.56±0.03 0.69±0.05 0.55±0.02 0.7±0.06 LVPW (mm/kg) + # 0.28±0.01 0.32±0.01 0.29±0.01 0.3±0.01 0.26±0.01 0.28±0.01 0.31±0.01 0.36±0.02** 0.32±0.01 0.32±0.02 0.3±0.01 0.31±0.02 1.67±0.04 1.91±0.06 1.77±0.05 1.97±0.14 1.73±0.05 1.8±0.12 88.53±1.04 85.4±1.54 88.49±0.89 86.41±1.17 88.44±1.17 83.12±1.85 1.49±0.05 1.73±0.08* 1.42±0.05 1.37±0.06 1.39±0.09 1.53±0.05 3.54±1.04 3.62±0.10*** 3.68±0.12 3.73±0.12** 3.63±0.07 3.67±0.26 0.45±0.02 0.42±0.01 0.44±0.02 0.45±0.02 0.44±0.02 0.46±0.02 3.48±0.11 3.476±0.077 3.08±0.14 3.36±0.15 3.15±0.11 3.09±0.07 0.83±0.03 1.08±0.04 0.89±0.02 1.03±0.05 0.84±0.03 0.97±0.04 0.55±0.03 0.71±0.04 0.64±0.02 0.75±0.04 0.57±0.02 0.70±0.02 LV measurements LVDd (mm/kg) + P P P P P IVS (mm/kg) + P P P LV mass (g/kg) + # P P LV function LVEF (%) # P P IVRTc (ms) RV dimensions RVD (mm/kg) + P P RVWT (mm/kg) + ### P P RV function TAPSE (mm) Left atrium LADd (mm/kg) + ## P P LADs (mm/kg) + ### P P 24 Right atrium RAD (mm/kg) + P P 0.79±0.03 1.06±0.07*** 0.79±0.04 1.0±0.05** 0.82±0.04 0.84±0.07 Significant interaction was found for LVDd, IVS, IVRTc, RVD and RAD, and pairwise comparisons (Sed vs Ex) are shown within each time-point. No interaction with a significant group (Sed, Ex) main effect was found for LVDs, LVPW, LV mass, LVEF, RVWT, LADd and LADs, and overall Sed vs Ex differences are shown. LVDd: left ventricle diastolic diameter; LVSd: left ventricle systolic diameter; LVPW: left ventricle posterior wall thickness; IVS: interventricular septum thickness; LVEF: left ventricular ejection fraction; IVRTc: isovolumetric relaxation time corrected by RR interval; RVD: right ventricular diameter; RVWT: right ventricular wall thickness; TAPSE: tricuspid annulus plane systolic excursion; DT: deceleration time; LADd: left atrial diameter in atrial diastole; LADs: left atrial diameter in atrial systole; RAD: right atrial diameter. *p<0.05, **p<0.01, ***p<0.001 Sed vs Ex. #p<0.05, ##p<0.01, ###p<0.001Sed vs Ex (group effect). + P P Values for chamber dimensions, LV wall thickness and LV mass, are normalized to body weight. NB. The results in Supplemental Table 3 are for a distinct group of rats from those in Supplemental Table 2; having been studied repeatedly at 16-week Ex, 4-week and 8-week detraining. 25 Supplemental Figure Legends Supplemental Figure 1: Running and distress assessment scores. (A) Representative diagram showing a semi-quantitative score system to evaluate the quality of running of all Ex rats (0 meaning refusal to run, 1 meaning very bad running with continuous contact to the electrical grid, and 5 being very good running confined to the front of the treadmill). An investigator graded all Ex rats every 5 minutes during each 60-minute training session, and an average score was obtained per rat at the end of each session. The left panel schematically shows the positionrange of rats in the treadmill corresponding to each score. Results of average running scores of Ex rats are represented on the right panel (whiskers showing min and max values). (B) Items assessed in the distress evaluation score. Each item was given a score between 0 and 2 or 3. Results (mean±SEM) for blinded distress assessment in the chronic (>18 hours after last training session) and acute (1 hour after training) settings are represented on the right. n=6 for both Sed and Ex. Supplemental Figure 2: Procedure for autonomic tone component assessment. (A) Time-course of heart rate changes after the administration of single intravenous doses of propranolol (2 mg/kg) or atropine (1 mg/kg; n=3 experiments/drug) in preliminary studies. Significant one-way ANOVA for each drug. n=3/group. Pairwise comparisons (post-hoc LSD) with heart rate at baseline (Bsl): *p<0.05, **p<0.01, ***p<0.001 vs baseline. (B) Representative heart rate recordings in experiments to assess parasympathetic and sympathetic tone before and after the administration of propranolol and atropine. Below each recording, a schematic representation showing β-, parasympathetic or double blockade status in parallel to heart rate changes. PS: parasympathetic; S: sympathetic. 26 Supplemental Figure 3: Procedure for the baroreflex sensitivity analysis. Representative recordings of mean blood pressure (mm Hg) and RR cycle length (ms) for phenylephrine (Phe) and nitroprusside (NTP) experiments are shown. Phe raises blood pressure and induces reflex bradycardia. After each dose of Phe, difference between baseline and maximum blood pressure, and difference between baseline and maximum cycle length (indicating minimum heart rate) were determined and plotted against each other. NTP lowers blood pressure, causing reflex tachycardia. After each dose of NTP, difference between baseline and minimum blood pressure and difference between baseline and minimum cycle length (indicating maximal heart rate) were measured and plotted against each other. Enlarged images for each dose indicating differences are shown within squares. Phe: phenylephrine; NTP: nitroprusside. Supplemental Figure 4: Representative recordings (ECG and atrial intracavitary electrogram, atrial EG) from a trained rat in which long-lasting AF (>15 minutes) was induced during EP study. Twenty seconds after the administration of atropine, AF reverted to sinus rhythm. Supplemental Figure 5: (A) Recordings from AF-inducibility burst-pacing tests in a sedentary rat. At baseline, no AF was induced. After the administration of 25 µg/kg of carbachol (CCh), non-sustained AF (3.7 seconds) was induced. After a cumulative dose of 50 µg/kg of carbachol, long-lasting AF was induced, reverting after 17 minutes (2 minutes after intraperitoneal atropine injection). (B) AF inducibility rates during EP study at each of the carbachol doses. Results are shown separately for all induced AF episodes (including both sustained and non-sustained AF) and only sustained AF episodes. CCh: carbachol; SAF: sustained AF. ***p<0.001 Sed vs Ex. 27 Supplemental Figure 6: (A) Current density-voltage relationship at 1 µM (n=9 for Sed, n=16) and 10 µM CCh (n=9 for Sed, n=17) doses. Average current density at -120 mV in both Sed and Ex group is shown at the right. (B) Time-constants for the time-dependent increase in current in both Sed and Ex group at 10 nM (n=9 for Sed, n=13 for Ex), 100 nM (n=9 for Sed, n=15 for Ex) and 1 µM (n=9 for Sed, n=16 for Ex). Supplemental Figure 7: mRNA expression of autonomic mediator and regulatory genes potentially involved in exercise-related autonomic remodeling. Autonomic receptor (A), and G-protein (B) expression-levels are shown. *p<0.05 Sed vs Ex by Mann-Whitney U-test. n=10 per group. Supplemental Figure 8: Structural and molecular remodeling in Ex rats with inducible long-standing AF (>15 minutes) compared to Ex rats with AF lasting <15 minutes. (A) Heart rate during EP study (n=9 for non-longlasting AF, n=5 for longlasting AF). (B-E) mRNA expression of autonomic mediators and regulatory genes in both groups study (n=6 for non-longlasting AF, n=4 for longlasting AF). (F) Echocardiography measurements of left and right atrial size (n=9 for non-longlasting AF, n=5 for longlasting AF). *p<0.05 Sed vs Ex by unpaired t-test. LL: Long-lasting inducible AF. n-LL: non-long lasting inducible AF. 28 29 30 31 32 33 34 35