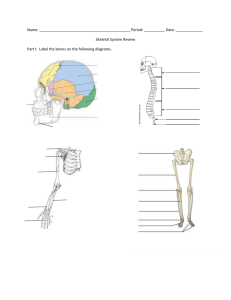
PEM Board Review Chapter 19: Trauma: Orthopedic & Hand A
advertisement

PEM Board Review Chapter 19: Trauma: Orthopedic & Hand A nondisplaced supracondylar fracture: although there is no obvious bony abnormality, the presence of a displaced anterior fat pad and a visible posterior fat pad suggest distention of the joint capsule: In the setting of a traumatic injury, this is likely a hemarthrosis due to an intra-articular fracture. Although an anterior fat pad may be normal, if present, as a thin radiolucency just anterior to the distal humerus, anterior displacement (“sail sign”) or the visible presence of the posterior fat pad are pathologic and suggest an underlying fracture. Appropriate management for such a fracture includes application of a posterior long-arm splint or long-arm cast and orthopedic follow-up care. Supracondylar fractures are the most common elbow fractures in children, with a peak incidence seen between the ages of 4 and 7 years. The most common causative mechanism is a fall onto an outstretched hand with the elbow in extension. Due to the position of the olecranon relative to the distal humerus when the elbow is extended, fracture through the supracondylar region with varying degrees of (most commonly) posterior displacement of the distal humerus results. Subtle displacement can be appreciated using the anterior humeral line; a line drawn along the anterior cortex of the humerus should intersect the middle third of the capitellum. If it crosses the anterior third, posterior displacement is present & vice versa. 1 If there is incomplete reduction or persistent neurovascular compromise, open reduction and fixation is performed. Diminished pulses or decreased perfusion that does not improve after reduction requires further evaluation with either surgical exploration or angiography. Volkmann ischemic contracture can result from unrecognized vascular compromise due to the fracture itself, vessel injury during reduction, or compartment syndrome. Orthopedic consultation is appropriate for a displaced supracondylar fracture, an open fracture, or a fracture with neurovascular compromise. Displaced fractures with neurovascular compromise require sedation and emergent reduction. Displaced fractures with intact neurovascular status can be reduced on a nonemergent basis. The estimated incidence of neurovascular injury in supracondylar fracture is 8% to 12%, which increases substantially if the fracture is displaced. The absence of a radial pulse is reported in 7% to 12% of all supracondylar fractures and 19% of displaced fractures. The most common nerve injured is the median (28% to 60%), followed by the radial (26% to 61%) and ulnar (11% to 15%). The brachial artery is the most commonly injured vascular structure in posteriorly displaced fractures. Thus, a detailed neurovascular examination is critical, including palpation of distal pulses and assessment of skin color, temperature, and capillary refill as well as sensory and motor aspects of the median, ulnar, and radial nerves. If the pulse is weak, Doppler ultrasonography should be undertaken. One of the earliest signs of ischemia is pain on passive flexion of the fingers, but such a finding is not possible to elicit in a comatose or an anxious child. Vascular injury can lead to compartment syndrome, with associated necrosis and fibrosis of the involved musculature. Some controversy surrounds whether a supracondylar fracture should be reduced immediately in the emergency department or be reduced in the operating room. A cool, pulseless hand that is still pink suggests some limb perfusion, and reduction in the emergency department might cause more harm and further impair flow. Radiography in a splinted position is needed to determine the extent of displacement. If the hand is cold, white, and pulseless, the clinician should perform gentle, inline traction in the emergency department to determine whether flow can be re-established prior to obtaining a radiograph. Application of a volar splint is appropriate for a distal forearm buckle fracture. This injury results most commonly from a forward fall onto an outstretched hand. Focal pain, tenderness, and swelling are present in the distal forearm. Supination of the forearm and flexion of the elbow while palpating over the radial head is one of two accepted methods for reducing radial head subluxation (nursemaid's elbow). Affected patients typically present with a history of being pulled by the involved arm. The injured arm is held in a pronated, slightly flexed, and adducted position, and there is generally no swelling or focal tenderness. Felon: an abscess of the digital pulp that is characterized by severe pain, swelling, and erythema of the pad of the fingertip. The distal phalanx encloses a connective tissue 2 framework in which multiple trabecula divide the pulp, which is composed of fat globules and eccrine sweat glands. The sweat glands open to the epidermis, providing a portal of entry for bacteria. Felon often is associated with a history of preceding minor penetrating trauma, such as a minor cut, splinter, or sliver. This closed compartment abscess requires urgent incision and drainage to prevent complications of osteomyelitis and necrosis of the finger tip. Local anesthesia should be achieved with a digital block. The preferred incision for drainage of a felon is parallel to the long axis of the digit and over the site of maximal fluctuance (volar longitudinal incision). The incision should not cross the distal interphalangeal joint, which could cause the complication of flexion contracture. In addition, probing proximal to the incision may cause extension of infection into the flexor tendon sheath. Lateral incisions are less preferred because of the potential for inadvertent injury to the digital nerves, which run along the radial and ulnar border of the digit. The “hockey stick” and “fishmouth” incisions (transverse incision at the distal tip of the finger) are associated with an increased risk of iatrogenic complications, which include permanent anesthesia, unstable fat pads, pain, and unacceptable scarring. After successful I&D of a felon, the wound should be packed with petrolatum gauze and the finger immobilized. A relative contraindication to drainage of a felon is more extensive finger and hand involvement, such as flexor tenosynovitis, which requires management by a hand surgeon. Administration of oral antibiotics to cover staph and strep is appropriate. IV ABX are not necessary if the wound is drained adequately. Paronychia is an inflammation or abscess of the lateral or posterior nailfolds. Occurs after minor local trauma, such as nail-biting, that disrupts the eponychial fold (cuticle), allowing bacteria to enter. Treated with warm soaks and antistaphylococcal oral ABX. If an abscess has formed, I&D is performed with an 11-blade scalpel along the cuticle of the involved nail margin, followed by warm soaks. Oral antibiotics also may be prescribed.If herpetic Whitlow is suspected, antibiotics are not indicated, and incision and drainage is contraindicated. The patient described in the vignette has suffered major trauma and has multiple areas of injury that require prompt care. The first priority, after initial stabilization, is to salvage the left hand, which is showing signs of neurovascular compromise (absent radial pulse, pale and cool extremity). The patient likely has a supracondylar fracture of the left extremity. The presence of signs of ischemia is an indication for immediate consultation with orthopedic surgery for reduction of the fracture. The injury sustained by the boy described in the vignette is suggestive of a fracture of the scaphoid (navicular) bone. The typical mechanism for this fracture is a fall onto an outstretched arm. Despite the lack of radiographic abnormality, he should be assumed to have a nondisplaced fracture until proven otherwise. Approximately 10% to 20% of patients who have scaphoid fractures do not have visible fracture lines on any radiographic view in the acute setting. Therefore, in the presence of a clinical suspicion (tenderness at the anatomic snuff box or pain on axial loading of the thumb), immobilization in a thumb spica splint is recommended, followed by repeat radiographs 3 and physical examination in 2 weeks. If the patient is pain-free and radiographs are negative at the time of follow-up, he or she may return to usual activities. If the radiographs are negative but pain persists on physical examination, the patient should undergo further imaging, such as magnetic resonance imaging. Because elastic bandages, commercial air splints, short arm volar splints, and slings allow mobility of the scaphoid bone, they should not be used when scaphoid fracture is suspected. Nonunion is rare in pediatric patients (<5%), but delayed diagnosis and improper or inadequate immobilization increase this likelihood. Most pediatric scaphoid fractures occur in teenage patients who sustain a fall on an outstretched pronated arm. Skateboarding and bicycling are the most frequent sports precipitating injury. Recommended treatment for avulsion type and incomplete fractures is immobilization for 4 to 6 weeks in a thumb spica cast. Most authors recommend 6 to 8 weeks of immobilization for middle third (waist) and transverse fractures. Some authors recommend a long arm cast initially, followed by short arm cast. Complications are more common with misdiagnosis and late presentation. Figure Grisel’s Syndrome: atlantoaxial rotary subluxation associated with inflammation or infection. If the subluxation is minimal and < 1 week in duration, no traction is required. All types show rotary displacement plus a) Type I: no anterior shift of axis; b) Type II: anterior shift <5mm; c) Type III: anterior shift > 5 mm; and d) Type IV: posterior shift of the axis. Treatment for Type I: soft cervical collar, analgesics, bed rest. Tx if sx’s 1-4 weeks: Hospitalization with halter traction, c-collar for 4-6 weeks; Tx if sx’s > 4 weeks: Hospitalization with skeletal traction, C-collar for 4-6 weeks. 4 Pseudosubluxation of C2 on C3 may be visible in up to 30% of lateral C-spine x-rays of children < 8 years old. Swischuk described the spinolaminar line, which is a line connecting the anterior edges of the spinous processes of C1 and C3. The line should pass through the cortex of the anterior edge of the spinous process of C2 or be less than 1-2 mm anterior to it. A larger distance warrants further investigation for a fracture. Fracture of the arch of C2 would be highest on the differential. The malalignment in pseudosubluxation is accentuated in flexion. The prevertebral soft tissue should be less than half the width of the adjacent vertebral body. Sever’s Disease: a calcaneal apophysistis, an overuse injury associated with running and jumping sports, especially in poorly cushioned cleats. It is seen in skeletally immature athletes, and may be associated with growth spurts in either gender. Symptoms are intermittent heel pain, positive squeeze test of heel, a tight Achilles Tendon, and pain over the calcaneal apophysis. Treatment: Achilles tendon stretching, a heel cup for the athletic shoe, and icing before and after physical activity. Iselin’s Disease: A apophysitis at the base of the 5th metatarsal. Stress fractures are less common in prepubescent athletes. Monteggia Fracture: a combination of a fracture of the middle or proximal ulna and a proximal dislocation of the radial head. Radial head alignment is assessed on a lateral film by the radial-capitellar line—a line drawn through the axis of the radial shaft that should bisect the capitellum in all views—need to assess elbow! Galeazzi Fracture: Middle to distal Radial fracture with distal ulna dislocation. These children will have difficulty with wrist pronation and supination—need to assess wrist! A Triplane Fracture involves the metaphysis (sagital plane), physis (transverse plane), and epiphysis (coronal plane). It is a type of SALTER IV fracture. It is more common in ages 12-15 years with partial closure of the tibial physis. Fibular fractures are often associated with this injury. Closed reduction may be adequate, but CT scan, to fully assess the alignment of the articular surfaces, is necessary to determine appropriate treatment. Those with residual displacement of >2 mm after closed reduction will require open reduction and fixation (> 50% of patients end up needing this). Remodeling of fractures in children allows for good outcomes with less than perfect initial alignment. Fractures that are closer to the growth plate have a better potential for remodeling with time. Bowing deformities do not remodel well, and often need reduction. “Acceptable allowances” in angulation and rotation are more conservative in patients over 10 years of age or who have less than 2 years of growth potential. Allowances in angulation for distal radius buckle fractures are up to 20 degrees for children less than 8-10 years old, and up to 10 degrees of angulation for those over 10 years old. In general, shortening of only 1 cm or less is acceptable. 5 Little League Elbow: Tenderness of the medial epicondyle from overuse; it precedes a fracture of the medial epicondylar apophysis. Ulna nerve dysfunction can occur with widely displaced fractures or when the fragment is impacted in the elbow joint, and emergent open reduction may be required to restore nerve function. The elbow should NOT be manipulated in a closed manner with evidence of nerve injury or compression! Hip dislocations in adolescents are usually the result of high impact trauma, such as high speed MVC’s, but not so in younger children. A posterior dislocation is much more common than an anterior dislocation. Under sedation, a posterior dislocation is reduced with the patient supine; the pelvis is stabilized by an assistant, longitudinal traction is applied to the thigh with the leg still in adduction and internal rotation, and, when adequeate muscle relaxation is achieved as evidenced by the return of the leg to normal length, the hip is flexed to 90 degrees and then gently abducted and externally rotated while extending the hip. To reduce an anterior hip dislocation, place the child supine, and pull the leg upward with the knee flexed. Reducing these dislocations within 6 hours reduces the risk of osteonecrosis. Sling and swath, with follow-up Ortho visit in 1 week is adequate for uncomplicated proximal humerus fractures without neurovascular compromise. Open physeal fractures (Seymour’s Fracture) of the distal phalanx should have the nail removed, the nail bed repaired and the dorsal nail fold splinted open and oral antibiotics are adequate. The ACL is the most commonly torn ligament in the knee. Both the Lachman (preferred) and the anterior drawer test are abnormal. These are performed with the hip and knee in 20-30 degrees and 90 degrees of flexion, respectively. While stabilizing the knee, the proximal tibia is anteriorly stressed. Movement of greater than 2 mm compared to the other knee, a “soft endpoint” or increased pain are considered abnormal. A posterior drawer test is used to test the integrity of the posterior cruciate ligament. McMurray and Apley tests are used to diagnose meniscal injuries, which usually present with medial or lateral joint line pain. The patellar apprehension test is used to evaluate patellar subluxation. Avulsion of the apophysis of the iliac crest is common in adolescents. The crest is attached to the external and internal oblique abdominal muscles. Increasing pain will be elicited with active flexion of the torso. Treatment consists of bed rest, ice, pain medications, then non-weight bearing for 2-4 weeks followed by PT. Internal fixation is considered if the fragment is displaced > 20 mm. The most common pelvic apophyseal injury in adolescents involves the anterior superior ileac spine (injured with forceful contraction of the Sartorius), then the anterior inferior iliac spine (rectus femoris) then the ischial tuberosity (hamstrings), then iliac crest (abdominal obliques). 6 For finger fractures, ANY rotational deformity should be initially corrected with closed reduction, and, if unsuccessful, with internal fixation. A skier with tenderness at the base of the ulnar aspect of the thumb after falling who has normal x-rays should be placed in a thumb spica splint for 3-6 weeks for a possible avulsion of the ulnar collateral ligament of the proximal phalanx of the thumb— commonly referred to as “skier’s” or “gamekeeper’s thumb”. You will see adduction instability of the first MCP joint of the thumb. Ulnar Nerve: wrist flexion, finger spread, and power grasping; also sensory to the ulnar aspect of the 4th finger and the entire 5th finger; injured in anterolaterally displaced supracondylar fractures. Median Nerve: flexion at the PIP joints, opposition of the thumb and 5th finger; anerior interosseous branch is tested with OK sign. Sensory to the 1st, 2nd, 3rd, and radial aspect of 4th; injured in posterolaterally displaced supracondylar fractures. Radial Nerve: wrist extension, thumbs up sign; sensation to the radial aspect of the dorsum of the hand; Injured in posteriomedially displaced supracondylar fractures. Gustilo Classification of open fractures with increased risk of complications with progressively higher numbers is: Type I: wound < 2 cm Type II: wound 2-10 cm Type III: wound > 10 cm A: adequate soft tissue coverage B: inadequate soft tissue coverage C: associated arterial injury Patients who have pain in their anterior tibial area out of proportion from what would be expected from a simple flare of Osgood-Schlatter could have a fracture of the tibial tubercle (which may be confused with Osgood-Schlatter Disease). It carries an increased risk of compartment syndrome due to tearing of the anterior tibial compartment vessels. A patient should be placed in a posterior splint and transferred immediately to a tertiary care center. Early signs of compartment syndrome are pain disproportionate to the injury, and increased pain with active flexion and passive extension. A compartment pressure > 30-40 mm Hg or within 30 mm Hg of the diastolic BP is abnormal. For Proximal Femur (Head and neck) fractures, the Delbet Classification, unlike other schemes is worse with a lower number: I-III are intracapsular and have a higher risk of vascular damage. Type IV (intertrochanteric) is outside the joint capsule and has a decreased risk of complications. In a younger child with a twisting knee injury who hears a “pop” and has a hemarthrosis, the most common cause is patellar dislocation, followed by tibial tubercle avulsion, 7 followed by tibial spine avulsion. Tunnel views should be ordered to evaluate the tibial spines in young children (in addition to standard views). For evaluating fractures of the metacarpals and phalanges, the physical exam is more accurate than x-rays in assessing for rotational injuries. When the fingers are flexed to the palm, all fingers should point to the scaphoid bone, and all the nails should be parallel with NO overlap of the fingers. The usual treatment for a boxer’s fracture (metacarpal neck fracture) is ulnar gutter splint with ortho follow-up in one week. However, closed reduction should be performed when: A) > 10 degrees of angulation in the 2nd and 3rd metacarpals B) > 20 degrees of angulation in the 4th metacarpal C) > 30 degrees of angulation in the 5th metacarpal Capitellum articulates with radius; Trochlea articulates with ulna “C-T” on AP view. Median nerve is the most common nerve injury in supracondylar fractures. A line drawn along the midshaft of the proximal radius should intersect the capitellum in all radiographic views. CRITOE: age at which elbow ossification centers appear: 1,3, 5, 7, 9, 11. C=capitellum R=radius I=internal (medial) epicondyle T=trochlea O=olecranon E=external (lateral) epicondyle Elbow dislocations: uncommon in children; most are posterior and closed. Nerve entrapment or a fracture fragment in the joint mandates surgery. For greenstick fractures, the angulation is overcorrected toward the cortical break, in essence, completing the fracture to prevent persistent angulation and subsequent deformity. A splint is then applied. For subungual hematomas > 25% nail removal and nail bed repair is often advocated but you can trephinate instead if the nail and nail margin is intact. Ankle Fractures: Tillaux fracture and Maisonneuve Fracture are at the more severe end of the injury spectrum. Tillaux Fracture: A Salter III fracture of the lateral distal tibia (due to asymmetric closing of the growth plate. CT may be required to see it and open reduction and internal fixation are usually required. 8 Maisonneuve Fracture: is actually 2 fractures—the first is a medial malleolar fracture of the distal tibia. The second is an oblique fracture of the proximal fibula. There is consequent disruption in the interosseous membrane between the tibia and fibula and the ankle joint is unstable—subsequent diastasis of the joint is likely. Require open reduction and internal fixation; pitfall—focusing the physical exam and x-rays just on the ankle and missing the proximal fibula. Ottawa Knee Rules: Obtain knee radiographs if there is a history of acute knee injury and at least one of the following: Inability to walk 4 steps immediately after the injury and in the ED (regardless of limp) Tenderness over the patella Tenderness of the head of the fibula Inability to flex the knee to 90 degrees Age greater than 55 years Ottawa Ankle Rules: Obtain ankle radiographs if there is acute ankle injury and at least one of the following: Inability to bear weight (4 steps) immediately after the injury and in the ED (regardless of limp) Tenderness to palpation over the posterior edge or tip of the lateral malleolus Tenderness to palpation over the posterior edge or tip of the medial malleolus Ottawa Foot Rules: Obtain foot radiographs if there is a history of acute foot injury and at least one of the following: Inability to bear weight immediately after the injury and in the ED Tenderness to palpation over the base of the 5th metatarsal Tenderness to palpation over the navicular bone Displaced fractures of the calcaneus and the midfoot sustained under a high-impact mechanism require ortho consultation in the ED. Avascular necrosis and compartment injuries are serious complications of these Lisfranc-type injuries (tarsometatarsal joint injuries after a midfoot plantar-flexion injury). Pseudo-Jones Fracture (Dancer’s Fracture): avulsion of the proximal 5th metatarsal—tx— hard soled shoe for 2 weeks Jones Fracture: fracture to the neck of the 5th metatarsal (more distal than pseudo-Jones); higher complication rate due to low vascular area therefore treatment is posterior splint and non-weight bearing with crutches. Compartment Syndrome: 6 P’s!! pain, pallor, pulselessness (palpable pulse does NOT exclude diagnosis!), paresthesia, prolonged capillary refill, and paralysis. Pallor and pulselessness are late findings. Early findings are disproportionate pain and pain on 9 passive stretch. Increased pain and decreased sensation are cardinal signs that a compartment syndrome is beginning. The boy described in the vignette has a clenched-fist injury with signs suggestive of tenosynovitis or early septic arthritis, necessitating inpatient management with parenteral antibiotics for a likely bacterial infection. Human bite injuries can be occlusional, in which the upper and lower teeth come together on a body part, or clenched-fist, in which the dominant hand typically strikes the teeth of another person. The former are more common in the young preschool child and more likely to occur on the face, upper extremities, or trunk. Child abuse should be suspected if the intercanine distance is greater than 3 cm (suggestive of an adult perpetrator) or occlusional bites are present on the genitals of a young child. Clenched-fist injuries are the most serious of human bite wounds and are more common in adolescents. Abrasions or lacerations occur typically on the fourth and fifth metacarpals. In many instances, the injuries are trivial and ignored by the patients. Clenched-fist injuries are highly prone to infection because of the proximity of the bone, joint capsule, and tendon to the overlying skin. In addition, relaxation of the skin and soft tissue after the fist is unclenched allows the oral microbes to enter a deeper and now effectively closed space, leading to septic arthritis, osteomyelitis, or tenosynovitis. Management of lacerations includes copious irrigation with sterile saline and removal of debris. Surgical evaluation to determine involvement of nerves, muscles, tendons, and bone is important. In general, lacerations should be left open and re-evaluated in a few days for delayed primary closure. Very large lacerations may be candidates for primary closure. Because most human clenched-fist wounds are small, local wound care, elevation of the injured extremity, and splinting and immobilization are indicated. Antibiotic prophylaxis is indicated in clenched-fist bites, deep puncture wounds, wounds requiring surgical repair, and those with associated crush injury. Monotherapy with amoxicillin-clavulanic acid is the prophylactic measure of choice. Alternatively, a twodrug regimen composed of an antibiotic active against Eikenella (doxycycline, trimethoprim-sulfamethoxazole, penicillin VK, cefuroxime, ciprofloxacin) and an antibiotic active against anaerobes (metronidazole or clindamycin) may be used. Antibiotics that are ineffective against Eikenella, including dicloxacillin, cephalexin, and erythromycin, should not be prescribed as monotherapy. Individuals who have infected hand wounds, should be hospitalized for evaluation and parenteral antibiotic therapy. Empiric antibiotic therapy with a beta-lactam/betalactamase inhibitor combination such as ampicillin-sulbactam, piperacillin-tazobactam, or ticarcillin-clavulanic acid should be initiated pending culture results. Alternate options include a third-generation cephalosporin with metronidazole or fluoroquinolones with metronidazole. The boy described in the vignette has an exsanguinating external hemorrhage and signs of compensated shock. The priorities that must be addressed simultaneously are control 10 of the hemorrhage and restoration of blood volume. The first step in attempting to control the hemorrhage is to apply direct pressure, which should be undertaken while simultaneously obtaining vascular access with at least two large-bore intravenous or intraosseous catheters. If bleeding cannot be stopped with direct pressure, use of the Windlass technique may be helpful. In this technique, a dressing is applied to the wound and held in place by a broad bandage that is secured by tying a knot directly over the wound. A pen or other cylindrical object is placed under the knot and rotated several times before being secured in place. This allows for maximal and sustained pressure directly over the wound. If the bleeding still cannot be stopped, application of a tourniquet may allow for stabilization until the patient can be brought to surgery. Although the use of tourniquets have been discouraged in the past due to concerns for ischemic injury, including injury to neurovascular structures, military experience in recent conflicts has shown they can play a safe role in temporarily controlling hemorrhage, especially in the prehospital setting. It is now accepted that a tourniquet may be left in place for up to 2 hours without significant risk of permanent ischemic injury. Multiple commercial tourniquet devices are available, and some trials have compared the effectiveness of various devices, but results do not conclusively support one device over another. Tourniquets that are applied in the prehospital setting should be left in place until the patient is transported to a site where definitive care is possible. In the emergency department, use of a tourniquet may allow for stabilization until the patient can be taken to the operating room. However, if a tourniquet has been in place and bleeding seems to be controlled, a trial of releasing it may be carefully undertaken. If hemostasis has been achieved it may sometimes be maintained after release of the tourniquet. In patients who are awake, the pain produced by ischemia with tourniquet use may require analgesics, including opioids if the patient is stable. Obtaining vascular access and attempting to restore blood volume without addressing the ongoing hemorrhage for this patient would likely be ineffective. Repair of an arterial laceration, as in this case, without operating room resources would have a small chance of success. Oversewing or stapling large scalp lacerations to obtain hemostasis can be efficacious, but this approach usually is not successful in vascular injuries of the limbs. In a study of nearly 300 children who had acute hip pain, Kocher and associates developed a clinical evaluation tool to determine the likelihood of septic arthritis. After retrospectively reviewing all of the cases, they used univariate analysis and multiple logistic regression analyses to compare patients who had true or presumed septic arthritis with those who had other diagnoses. Four predictors were ultimately identified: • Fever > 38 (100.4) • Elevated white blood cell count (>12x103/μL [12x103/L]) 11 • Elevated inflammatory marker(s) (ESR >40 mm/h) • Inability to bear weight The likelihood of septic arthritis based on number of predictors was: less than 0.2% with zero, 3% with one, 40% with two, 93% with three, and 99.6% with four predictors. Based on this algorithm, this girl had one predictor (fever) and a resultant 3% likelihood of having septic arthritis. If results of the initial laboratory and radiographic evaluations are normal and the child is able to bear weight, discharge with outpatient follow-up is appropriate. Children who have fever and elevated inflammatory markers or white blood cell counts should receive further evaluation for possible septic arthritis, osteomyelitis, or tumor. Such evaluation may include computed tomography scan, magnetic resonance imaging, bone scintigraphy, or ultrasonography to identify joint effusion or to guide joint aspiration. Hospitalization should be considered for patients who are unable to bear weight after administration of appropriate analgesic agents. 12