CARDIOVASCULAR EXAMINATION
advertisement

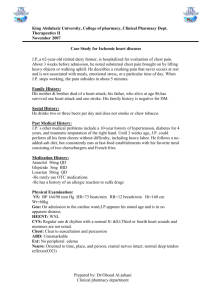
Dr. J.A. Coetser GKV 353 CoetserJA@ufs.ac.za 0833542861 A 56 year old white male presents to casualties at 3h40am, complaining of severe chest pain that started 30min earlier. WHICH IMPORTANT ASPECTS WOULD YOU ELICIT FROM THE HISTORY? When evaluating symptomatic complaints • Site • Onset • Character • Radiation • Alleviating factors • Timing • Exacerbating factors • Severity Determine the cause! 4 cardinal features • Duration (timing) • Location (site) • Quality (character) • Precipitating and aggravating factors Angina • Crushing pain, heaviness, discomfort or choking • • • • sensation in retrosternal area Central rather than left chest May radiate to jaw and/or arms Rarely below umbilicus Typical vs. atypical angina Typical vs. atypical angina Typical angina Meets all 3: 1. Characteristic restrosternal chest discomfort – typical quality and duration 2. Provoked by exertion or emotion 3. Relieved by rest or GTN or both Atypical angina Meets 2 of above Non cardiac chest pain Meets 1 or none of above Pain from acute coronary syndromes (myocardial infarction and unstable angina) • Often comes on at rest • Pain present >30min Angina Acute coronary syndromes • Clot dissolves • Coronary blood flow returns • No cardiac muscle damage UNSTABLE ANGINA • Clot persists • Coronary blood flow cut off • Cardiac muscle dies MYOCARDIAL INFARCT Pleuritic pain • Due to movement of pleural surfaces on one another • Inflammation of pleura or pericardium Viral infection of pleura Pneumonia Pulmonary embolism • Made worse by inspiration • Often relieved by sitting up and leaning forward Dissecting aneurysm • 3 features Severe, tearing pain Rapid onset Radiates to back • Proximal aorta dissection = anterior chest pain • Descending aorta dissection = interscapular pain • Hx of HPT, or connective tissue disorder e.g. Marfan’s syndrome Massive pulmonary embolism • Sudden onset • May be retrosternal/angina-like • Can be associated with dyspnoea, collapse and cyanosis Spontaneous pneumothorax • Sharp pain and severe dyspnoea • Localized to one part of chest Oesophageal disorders • Reflux disease can mimic angina • Oesophageal spasm Especially after drinking hot or cold fluid Associated with dysphagia Relieved by nitrates Don’t forget: • Cholecystitis • Herpes zoster Dyspnoea definition: unexpected awareness of breathing • Sensation of increased force needed for work of breathing Need to distinguish between cardiac and respiratory causes Cardiac dyspnoea • LV output fails to rise during exercise • Increased LV end-diastolic pressure • Raised pressure in LA • Raised pressure in pulmonary venous system • Leakage of fluid into interstitial space • Decreased lung compliance NYHA classification of dyspnoea Class I Disease is present, but no dyspnoea OR Dyspnoea only on heavy exertion Class II Dyspnoea on moderate exertion (climbing stairs) Class III Dyspnoea on minimal exertion (getting dressed, washing) Class IV Dyspnoea at rest Orthopnoea • Dyspnoea in the supine position • In supine position, interstitial oedema distributes to all lung zones, decreasing overall oxygenation • In sitting position, oedema redistributes to lower zones, leaving upper zones free for oxygenation • Other causes of orthopnoea Massive ascites Pregnancy Bilateral diaphragmatic paralysis Large pleural effusion Severe pneumonia Paroxysmal nocturnal dyspnoea (PND) • Severe dyspnoea that wakes patient from sleep • Has to sit up and gasps for breath • Mechanism Sudden failure of LV Reabsorption of peripheral oedema at night while supine with overload of LV Don’t forget anxiety as cause of dyspnoea • Inability to take deep enough breath to fill lungs in satisfying way Ankle oedema of cardiac origin • Usually symmetrical • Worst in evenings, improves during night • As failure progresses, involves legs, thighs, genitalia and abdomen • Find out if pt is on a calcium channel blocker, i.e. Adalat XL® (nifedipine), amlodipine, etc., which can also cause ankle oedema • If oedema also involves face, think of nephrotic syndrome Definition palpitations: unexpected awareness of the heartbeat • Ask pt to tap out beat with finger • Ask if palpitations are slow or fast, regular or irregular, and what the duration is • Any fast arrhythmia can produce angina if pt also has ischaemic heart disease Atrial fibrillation • Completely irregular rhythm Atrial or ventricular ectopic beat • Sensation of skipped beat, followed by particularly heavy beat Ventricular tachycardia • Rapid palpitations followed by syncope Syncope = transient loss of consciousness resulting from cerebral anoxia, usually due to inadequate cerebral blood flow Presyncope = transient sensation of weakness without loss of consciousness (I’m about to faint) NB: ask about family history of sudden death • Long QT syndrome / Brugada syndrome Postural syncope • LOC when standing for long periods or standing up suddenly Ask about drugs that can cause postural hypotension Micturition syncope • LOC when passing urine Vasovagal syncope • LOC with emotional stress Syncope due to arrhythmia • LOC regardless of position Exertional syncope • Aortic stenosis • Hypertrophic cardiomyopathy Claudication = pain in one or both calves (thighs or buttocks) on walking more than a certain distance (claudication distance) 6 P’s of peripheral vascular disease • • • • • • Pain Pallor Pulselessness Parasthesiae Perishingly cold Paralysed Lumbar spinal stenosis (pseudo claudication) • Pain relieved by flexing spine • Exacerbated by walking downhill Common symptom of cardiac failure Remember other causes • Lack of sleep • Anaemia • Depression Previous ischaemic heart disease Hypercholesterolaemia Smoking Hypertension Family history • 1st degree relatives (parents of siblings) • Especially if <60yrs Diabetes mellitus • DM is a coronary heart disease equivalent • Risk of diabetic for MI is the same as a non-diabetic who has had an infarct Chronic kidney disease Which medications? Any side-effects? Previous procedures, e.g. CABG, angioplasty • Ask how many arteries were bypassed? • How many stents were placed? Previous MI or angina? • Increases risk for further events Rheumatic fever Hypertension • Alcohol use • Salt intake • Obesity • Lack of exercise • Kidney disease • NSAIDs Ischaemic heart disease can interfere with daily functioning • Is patient still working? • Has living arrangements changed? Enquire about rehabilitation programs