Going Out on a Limb - Lourdes Health System
advertisement

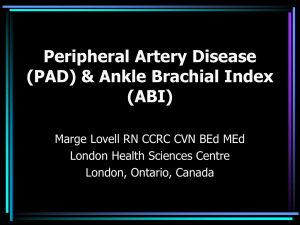
No Financial Disclosures Adam M. Levine, D.O. FACC Lourdes Cardiology Services South Jersey Heart Group September 13, 2014 • Who is at risk for development of PAD • When and How to screen • How to treat • PAD affects 12-20% of Americans age 65 and older.1 • 12 million with PAD in the U.S. alone2 • 3x greater risk in those with diabetes over the age of 50.3 • 4x greater risk in current or past smokers. 1 1. Becker, GJ, et al. The Importance of Increasing Public and Physician Awareness of Peripheral Arterial Disease. J Vasc interv Radiol 2002; 13[1];7-11. 2. “Peripheral Arterial Disease in People with Diabetes”, American Diabetes Association Consensus Statement, Diabetes Care, Volume 26, Number 12, December 2003, 3333-3341. 3. “Diagnosis of PAD is Important for People with Diabetes”, American Diabetes Association Consensus Statement, Diabetes Care, November 21, 2003, www.diabetes.org. • Age less than 50 years with diabetes, and one additional risk factor (e.g., smoking, dyslipidemia, hypertension, or hyperhomocysteinemia) • Age 50 to 69 years and history of smoking or diabetes • Age 70 years and older • Leg symptoms with exertion (suggestive of claudication) or ischemic rest pain • Abnormal lower extremity pulse examination • Known atherosclerotic coronary, carotid, or renal artery disease • Asymptomatic, may have functional impairment • Reproducible (typical) claudication • Atypical Leg Pain • Critical Limb Ischemia • Rest pain, tissue loss, threatened limb loss • Acute Limb Ischemia • Pain, Pulseless, Pallor, Parasthesias, Paralysis • 1.5-2 million people in the US and Europe suffer from CLI1 • Mortality rates for CLI patients2 •at one year : 25% •two years : 31.6% •three years : 60% • 40-50 % amputation rate within 1st year of Dx. 3 1-2. “Conquering Critical Limb Ischemia”, Michael R. Jaff, DO and Giancarlo Biamino, MD, Endovascular Today, February 2004, Volume 3, No. 2 3. Dormandy J.A., Heeck L., Vig S.: The fate of subjects with critical leg ischemia. Semin Vasc Surg 12. 142-147.1999; Symptomatic and Asymptomatic PAD Prior Diagnosis of PAD Newly Diagnosed PAD (n=457) (n=366) 5.5 12.6 46.3 61.7 25.8 48.3 Claudication No Symptoms Hirsch AT et al. JAMA. 2001;286:1317-1324. Non-Specific Symptoms PARTNERS Study Prognosis in Patients with Intermittent Claudication Population >55 yr Intermittent Claudication Peripheral Vascular Outcomes Worsening Claudication 16% Lower Extremity Bypass Surgery 7% Adapted from Weitz JI et al. Circulation. 1996;94:3026-3049. Other Cardiovascular Morbidity/Total Mortality Major Amputation 4% Nonfatal Cardiovascular Event (MI/Stroke, 5-year Rate) 20% 5-yr Mortality 30% Cardiovascular Cause 75% Does “Asymptomatic” PAD Really Matter? Coronary Artery Surgery Study (CASS) in patients with known CAD the presence of PAD increased Cardiovascular mortality by 25% during a 10 yr follow-up (J AM Coll Cardiol 1994:23:1091-5) PAD, symptomatic or asymptomatic, is a powerful independent predictor of CAD and CVD (Vasc.Med.3,241,1998.) • Claudication: Dull cramping or pain in muscles of hips, thighs or calf muscles when walking, climbing stairs, or exercise which is relieved with cessation of activity • Fatigue in legs which may require patient to stop and rest while walking • Slow or shuffled gait & having difficulty keeping up with others • Neuropathy or pain in feet with exercise • Rest pain or night pain that occurs when legs elevated in bed, relieved when placed in dependent position. Typically in the distal foot, possibly in vicinity of an ulcer • Impotence may be a sign of iliac disease and may see some relief with sildenafil citrate. Differential Diagnosis of Exertional Leg Pain • Vascular Causes Atherosclerosis Thrombosis Embolism Vasculitis Thromboangiitis obliterans Takayasu arteritis Giant cell arteritis Aortic coarctation Fibromuscular dysplasia Irradiation Endofibrosis of the external iliac artery Extravascular compression Arterial entrapment (e.g., popliteal artery entrapment, thoracic outlet syndrome) Adventitial cysts • Cool, dry, atrophic skin on legs • May have signs of cellulitis • • • • • • Thickened or deformed nails-dystrophic Hair loss or uneven distribution on legs Muscle weakness or atrophy Bruits on auscultation Ulcers or wounds on lower extremities Gangrene • Pulse intensity should be assessed and should be recorded numerically as follows: • • • • 0 - absent 1 - diminished 2 - normal 3 - bounding Non-invasive tests1 ABI (Ankle/Brachial Index) Exercise Test Segmental Pressures Segmental Volume Plethysmography Duplex Ultrasonography MRA (Magnetic Resonance Arteriography),or CTA Invasive tests1 Peripheral Angiography 1. Krajewski and Olin Chapter 11 Peripheral Vascular Disease. 2nd ed. 1996 I IIa IIb III MODIFIED The resting ABI should be used to establish the lower extremity PAD diagnosis in patients with suspected lower extremity PAD, defined as individuals with 1 or more of the following: exertional leg symptoms, nonhealing wounds, age ≥65 years, or ≥50 years with a history of smoking or diabetes. 2011 ACC/AHA Guideline for Management of PAD The Ankle-Brachial Index ABI = Lower extremity systolic pressure Brachial artery systolic pressure Normal PAD Rest pain/ulceration 0.95-1.2 <0.90 <0.40 The Ankle-Brachial Index is 95% sensitive and 99% specific for PAD Both ankle and brachial systolic pressures are obtained using a hand-held Doppler instrument Source: Peripheral Arterial Disease in People with Diabetes, ADA, Consensus Statement, Diabetes Care, Volume 26, Number 12, December 2003. Performing a resting ankle-brachial index measurement ABI >1.30 (abnormal) PVR, Toe-brachial index Duplex ultrasonography ABI 0.91 to1.30 (borderline &normal Measure ABI After exercise test MRA, or CTA Peripheral Angiography ABI <= to 0.90 (abnormal) Confirmation of PAD diagnosis Decreased post-exercise ABI Duplex ultrasonography MRA,or CTA Peripheral Angiography Duplex ultrasonography MRA,or CTA Peripheral Angiography Exercise ABI Confirms the PAD diagnosis Assesses the functional severity of claudication May “unmask” PAD when the resting ABI is normal I IIa IIb III • Duplex ultrasound of the extremities is useful to diagnose anatomic location and degree of stenosis of peripheral arterial disease. • Duplex ultrasound is useful to provide surveillance following femoral-popliteal bypass using venous conduit (but not prosthetic grafts). 2011 ACC/AHA Guideline for Management of PAD Arterial Duplex Ultrasound Testing Duplex ultrasound of the extremities can be used to select candidates for: • endovascular intervention; • surgical bypass, and • to select the sites of surgical anastomosis. However, the data that might support use of duplex ultrasound to assess long-term patency of PTA is not robust. • Duplex Ultrasound 3, 6, 12 months post and at yearly intervals • Early Failure Rates 9-47% after PTA • If recognized secondary patency rates > 90% • Indications for restudy • Worsening ABI ( 0.15) is an indication for restudy • Decreased flow less then 40 cm/sec • PSV >180 cm/sec, Vr > 2 I IIa IIb III • MRA of the extremities is useful to diagnose anatomic location and degree of stenosis of PAD. • MRA of the extremities should be performed with gadolinium enhancement. (Level of Evidence: B) • MRA of the extremities is useful in selecting patients with lower extremity PAD as candidates for endovascular intervention. I IIa IIb III • Computed tomographic angiography (CTA) of the extremities may be considered to diagnose anatomic location and presence of significant stenosis in patients with lower extremity PAD. • CTA of the extremities may be considered as a substitute for magnetic resonance angiography (MRA) for those patients with contraindications to MRA. Contrast angiography provides detailed information about arterial anatomy and is recommended for evaluation of patients with lower extremity PAD when revascularization is contemplated. (Class I, LOE B) • Suspected PAD • exertional leg symptoms or non-healing wounds • Age ≥65 years • Age ≥50 years with a history of smoking or diabetes. • ABI/PVR • If normal and symptomatic then Exercise ABI • • • • Duplex ultrasound MRA CTA Angiogram • Risk Factor Modification • Hypertension - BP < 140/90 • Diabetes – HgA1c ≤ 7% • Hyperlipidemia – LDL ≤ 100 • Smoking Cessation • Supervised Exercise Program (30-45 min/day, 3 days/week) • Class I, LOE A • Antiplatlet to reduce risk of MI, stroke, vascular death in PAD • Symptomatic • Aspirin (Class I, LOE B) • Clopidogrel (Class I, LOE B) • Asymptomatic • If ABI ≤ 0.90 (Class IIa, LOE C) • Cilostazol (Class I, LOE A) • Indicated to improved symptoms and increase walking distance in PAD • Contraindicated in CHF • 100mg BID • Endovascular • Advantage • • • • Local anesthesia No vein grafts needed Fast recovery Potential for Hybrid approach • Disadvantage • Lower Patency rates • Need for repeat procedures • Surgical • Advantage • Less interventions • Better patency • Disadvantage • • • • General anesthesia Need vein grafts Longer recovery Higher systemic complications 1 year primary patency 2 year primary patency 58% 51% Stents 65-85% 55-68% Bypass 77-81% 66-77% Percutaneous Transluminal Angioplasty (PTA) Source: J Endovas There 2004;11(suppl II):II-107-II-127 “Lower Extremity Endovascular Interventions” Bates and AbuRahma • Who is at risk for development of PAD • Diabetes, known vascular disease, Smokers, Older age • When and How to screen • Exertional leg symptoms or nonhealing wounds • Anyone age ≥65 years or ≥50 years with a history of smoking or diabetes. • ABI and doppler ultrasound is first line • How to treat • Aspirin, exercise, risk factor modification, cilostazol, revascularization • Prevention is KEY!!!!! • When in doubt, refer to your local vascular specialist.