Approach in Vascular Patient
advertisement

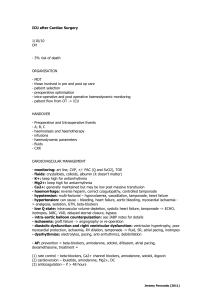
Approach in Vascular Patient กิตติพนั ธุ์ ฤกษ์เกษม PhD, FACA Topic • Artery - Limb Ischaemia - Aneurysm • Venous - Varicose vein • Leg ulcer Limb Ischaemia • Aetiology: most often atherosclerosis > trauma • Most management decisions are based upon 1.Differentiation acute vs chronic 2. Mechanism of occlusion 3.Location of the occlusion 4.Status of limb 5.Fitness of patients 1.Differentiation acute vs chronic What is acute ischaemia? Acute ischaemia • Period of onset in minutes or hours • Sudden catastrophic • Less effect in upper extremity and leg affected by chronic ischaemia Acute ischaemia • Symptom 5P pain pulselessness paresthesia pallor paralysis Marble white right foot in acute limb ischaemia What is chronic ischaemia? Chronic ischaemia • Symptom of limited circulation over months or years • Slow deterioration of function • Gradually symptom • Life style changes-stop smoking or exercise: remission collateral vv Chronic ischaemia • Symptom and sign Claudication rest pain ulceration/gangrene Why should the effectes of acute arterial ischaemia occlusion be less in someone affected already by symptom of chronic ischaemia or in upper limb? Collateral vessels!! 2. Mechanism of occlusion Acute iscahemia caused by •Trauma • Non trauma - embolus - thrombosis Trauma-fracture tibia Embolus • Mobile solid mass • Free floating in blood • Capable of occluding a vein or artery distal to its site of origin Composition of embolus • Atheromatous debris or thrombus(clot) (common) Common source of atheromatous or thrombus emboli • • • • Left ventricle wall after MI Left atrium in atrial fibrillation Diseased mitral valve or aortic valve Atheromatous plaques in aorta or iliac vessels This embolus lodge at the area where arterial tree is smaller than the embolus e.g. bifurcation or pre-existing stenosis Atheromatous debris-blue toe syndrome Thrombosis • Rupture of an atheromatous plaque esp moderate and severe stenosis • Virchow’s triad: abnormality of flow, blood, vessel wall Is it possible to differentiate between thrombosis and embolus as a cause of acute ischaemia?? • Sometimes!!! • Previously asymptomatic, preexisting cause with sudden onset of severe ischaemia (normal contralateral pulse) = embolus • Previous claudication and sudden onset of acute ischaemia = thrombosis Chronic ischaemia • Progressive narrowing • Cause : Atheromatous disease is the common cause Other uncommon cause: Aneurysm: » popliteal aneurysm: special nature » Diabetes Some rare disease » Buerger’s disease » Hyperhomocysteineaemia » Takayasu’s disease 3. Location • Acute occlusion: more proximal, the more extensive ischaemia • Diagnostic location determines the best treatment 3. Location-aorto-iliac disease • Chronic: claudication at buttock, thigh calf, loss of femoral pulse in men: Leriche syndrome (French surgeon who described distal aortic occlusion and erectile impotence) • Acute: catastrophic for ipsilateral limb, buttock, perineum Distal aorta occlusion Location Common femoral disease • Chronic: thigh and calf claudication, palpable the femoral pulse just below inguinal ligament • Acute: femoral bifurcation is the common site of embolus-typical ischaemic limb Location-superficial femoral disease • Chronic :a very common place for stenosis or occlusion where it passes posteriorly through adductor hiatus (Hunter’s canal) It can produce calf claudication, but rarely severe in presence of profunda femoris artery • Acute: rare Bilateral occlusion of superficial femoral artery with collateral circulation via profunda Location-popliteal atery dsease • Chronic: calf claudication • Acute: sudden occlusion from thrombus or embolus causes severe ischaemia due to occlusion geniculate arteries Location: crural arterial disease • Occlusion only one out of three vessel can asymptom unless either chronic or acute disease involve all three vessels 4. Status of the limb-acute iscahemia Determine chance of saving limb vs amputation • Pain: severe pain not response to opiate with tenderness in muscle:often irreversible ischaemia • Paresthesia: range from percentible alternation to numbness. Numbness indicate acute critical ischaemia • Pallor: pale -> unfixed mottling -> fixed mottling (do not blanch on pressure) frequently beyond salvage 4. Status of the limb-acute ischaemia • Pulselessness • Paralysis: stiff of the limb, when patient cannot move ankle joint indicated severe ischaemia 4. Status of the limb –chronic ischaemia Early calf claudication like angina i.e.tight, stiff or crushing pain What factors influence claudication distance? Anything increases work of walking • • • • Excess weight Walking uphill Walking against wind Carry shopping More severe form • Very short distance- a few steps • Rest pain first felt in the distal parts such as toes and dorsum of the foot – awake patient need rise from bed and walking around to relieve • Unable to lie flat without pain patient sleep with hanging leg out of beds cause edema and worsen microvascular perfusion Hanging foot Last stage of chronic • Gangrene, clinical depend on the degree of decomposition • Range from ulcer (skin necrosis) to gangrene of toe and foot • Gangrene: wet gangrene: black, soggy, discoloured green and malodorous requires urgent amputation Dry gangrene: black hard, brittle, wrinkle rarely odour : may autoamputation or surgery in proper time 5. Fitness of patient • Determine investigation and treatment “ surgeon need to consider the ability of the patient to withstand our effort. Our job should be relieve the symptom of which the patient complain” • Common causes of unfitness - pre-event unfitness: cardiac e.g. MI, Lung-renal-metabolic disease - per-event unfitness: dehydration, acidosis, uncontrolled DM - postevent unfitness: myoglobinaemia, severe acidosis, MI Investigation of occlusive disease • Clinical examination: full history » Presence or absence of pulse » Status of the limb » Other test BUN, CR, electrolyte CBC, plasma viscosity Coagulation EKG, CXR Fixed wave Doppler examination • Ankle brachial pressure index (ABPI) 0.5-0.9 claudication < 0.5 critial limb ischaemia < 0.3 gangrene Treadmill testing • Walking incline 10% at speed 3 km/hr • Test of function to allow monitoring disease and the result of therapeutic effort Ultrasound-duplex scan • Composed of 1. B-mode ultrasound reveal the anatomy:aneurysm, 2. occlusive lesion Doppler signal: flow indicate stenosis Duplex scan of SFA stenosis Contrast arteriography • Injection contrast agent make lumen visible • Conventional angiogram: direct intraarterial route • Now we have digital subtraction angiogram(DSA) • CT angiogram: need of arterial puncture • From the picture, what is the diagnosis? Computerised tomographic (CT) angiograhy • Helical CT scan with intra-arterial contrast injection • Look the relation between artery and other structure well Carotid body tumor Magnetic resonance arteriography(MRA) • without contrast or IV gadolinium • Suitable in patient should not given iodine containing contrast due to renal disease or allergy Aneurysm • Pulsatile expansile mass Clinical feature: • invade surrounding tissue cause- pain • rupture • embolisation - ischaemia e.g. claudication, trash foot Ruptured AAA Trash foot-multiple small atheromatous debris Investigation • Ultrasound • CT scan • ??? angiogram CT scan “Infrarenal AAA” Angiogram of popliteal aneurysm Venous disease Functional anatomy • Superficial venous system devided into 3 parts Long saphenous vein (LSV) Short saphenous vein (SSV) Perforating or communicating vein (PV) Superficial venous system • LSV: medial malleolus to groin • SSV: outer border of foot behind lateral malleolus ascend to middle of the calf 60% to pop V., 20% to LSV and 20% wherelse Superficial venous system • PV connnect superficial and deep vein • > 50 PV in one leg • PV in thigh connect directly between superficial and deep system, in leg connect indirectly via venous plexus Deep venous system • 3 artery below knee, there are 2 vein beside of artery from foot up to knee joint • Then pop V beside artery then in thigh ->superficial femoral vein join with profunda femoris vein -> common femoral vein Physiology of venous drainage • Normal: superficial to deep and from distal(foot) to proximal(thigh and heart ) • ?? At standing position, blood at ankle has to return against gravity to heart over a distance of > 1 metre “how” How 4 factors support this system • Functioning vein valves: resist > 300 mmHg • Functioning foot and calf muscle pumps: weight compress venous plexus in foot and calf muscle compress sinusoidal and deep vein in leg • Residual arterial pressure • Negative intrathoracic pressure “ however absent valve or damaged valve, the muscle pump cannot work efficiently” Pathophysiology of varicose vein • Abnormal dilated and tortuous superficial vein of the leg • Response to a pathological increase in the vein’s intraluminal pressure • This increases due to higher intraluminal pressure of deep vein (necessary to allow movement of blood out of leg) from deep to superficial system Aetiology • Primary e.g. saphenofemorla valve incompetence Aetiology • Secondary mostly due to previous DVT – Simple obstruction – Destroying the valves within deep vein These lead to blood move to superficial system (compensatory mechanism) ** a must to know this, otherwise we may worsen patient with VV surgery** Primary VV or secondary VV Clinical feature of varicose vein • • • • • Cosmetic presentation Discomfort and pain Cramps Swelling Complication - thrombophebitis - haemorrhage - CVI Patients assessment in VV(1) • History: past Hx of DVT • Examination: standing position Area of VV Brodie Tredelenberg test Perthes’ test Continous wave Doppler VV Brodie Tredelenberg test Patients assessment in VV(2) • Radiological evaluation when suspected of previous DVT Duplex scan Ascending venography (inject radioopaque in foot and watching it rise in the deep vein) Varicose eczema Chronic leg ulcer Neuropathic ulcer Venous ulcer Arterial ulcer Acute non-traumatic leg pain Localised to skin soft tissue, vein -cellulitis -lymphagitis -thrombophlebitis Pain radiate from back Exacebate by bending -lumbosacral N root compression Deep pain in whole legThigh, calf 5P Pain, uniform swelling No paresis or sensory loss Emboli source, no IC,N contralat pulse*heparin +ac emboli - ac thrombosis DVT, rupture of baker’s cyst Chronic non-traumatic leg pain Pain radiate from back Exacebate by bending -lumbosacral N root compression Pain in calf, foot Not radiate to back claudication Critical limb ischaemia Rest pain, gangrene, ulcer Varicose vein History of swelling, DVT Confirm with duplex scan Primary VV Intervention Sx, sclerotherapy Secondary VV Supportive treatment edge base Ulcer Punch out Black, dry Deep to tendon position Digit, heel Ischaemic ulcer Flat, sloping edge, soft Shallow, edema, erythrema Infection, granulation tissue Digit, pressure Point, heel, metartarsal head Sensory ulcer Above media malleolus Asso DVI Venous ulcer