biochemical markers in acs
advertisement

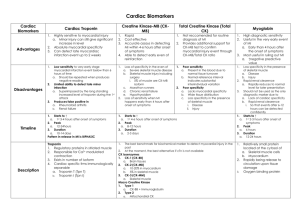
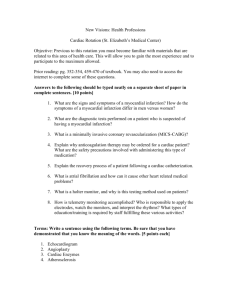
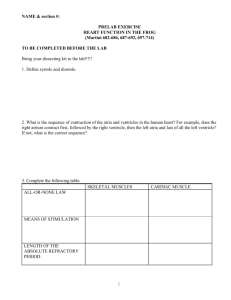
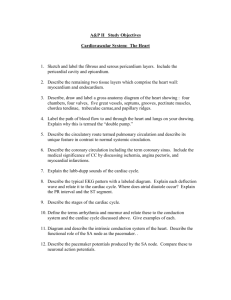
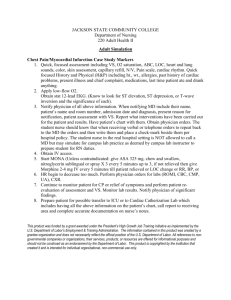
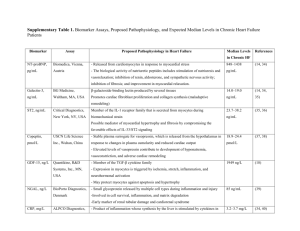
Biochemical Markers in Cardiac Disease Dr/Ehsan Mohamed Rizk ACUTE CORONARY SYNDROME (ACS) Ischemic heart diseases (acute coronary syndrome) includes: 1-Angina 2-Unstable angina 3-Myocardial infarction: most serious form of ischemia that leads to injury or even death of myocardium. The most common cause of myocardial ischemia is atherosclerosis. Risk factors for Coronary Artery Disease: 1-Age 2-Gender 3-Family history 4-Hyperlipidemia 5-Smoking 6-Hypertension 7-Diabetes 8-Obesity 9-High plasma homocysteine levels CRITERIA FOR DIAGNOSIS OF ACS Triad of criteria: Clinical picture Severe & prolonged chest pain Atypical pain (epigastric) Silent ischemia. ECG changes consistent with acute MI Elevated serum cardiac MARKERS Diagnosis requires at least two of them. CARDIAC MARKERS MUST BE: Located in the myocardium. Released in cardiac injury. – – – – Myocardial infarction Non-Q-wave infarction Unstable angina pectoris Other conditions affecting cardiac muscle (trauma, cardiac surgery, myocarditis etc.) Can be measured in blood samples. THE IDEAL CARDIAC MARKER HIGH SENSITIVITY HIGH SPECIFICITY High concentration in myocardium Released after myocardial injury: Absent in non-myocardial tissue Rapid release for early diagnosis Not detectable in blood of nondiseased subjects The ideal cardiac marker does ANALYTICAL CLINICAL CHARACTERISTICS CHARACTERISTICS NOT yet exist! fk Long half-life in blood for late diagnosis Measurable by cost-effective method Simple to perform Rapid turnaround time Sufficient precision & accuracy Scand J Clin Lab Inves 1999;59 (Suppl 230):113-123 Ability to influence therapy Ability to improve patient outcome CARDIAC MUSCLE CELL Size and subcellular distribution of myocardial proteins determines time course of biomarker appearance in the general circulation CLASSIFICATION OF LABORATORY TESTS IN CARDIAC DISEASE Markers of cardiac tissue damage Markers of myocardial function Cardiovascular risk factor markers Genetic analysis for candidate genes or risk factors PATHOPHYSIOLOGY OF ACS Proinflammatory Cytokines IL-6 Plaque Destabilization MPO Plaque Rupture sCD40L Acute Phase Reactants hs-CRP Ischemia IMA Necrosis cTnT cTnI Myocardial Dysfunction BNP NT-proBNP BIOCHEMICAL MARKERS IN MYOCARDIAL ISCHAEMIA / NECROSIS RECENT CK-MB (mass) c.Troponins (I or T) Myoglobin FUTURE: Ischaemia Modified Albumin Glycogen Phosphorylase BB Fatty Acid binding Protein Highly sensitive CRP. Traditional AST activity LDH activity LDH isoenzymes CK-Total CK-MB activity CK-Isoenzymes ASPARATATE AMINOTRANFERASE (AST) An enzyme that catalysis the transfer of amino group from amino acid to keto acid which is important for providing α keto acid for tricarboxylic acid cycle (energy production) and providing amino acid for urea cycle. It is widely distributed in hear, liver, skeletal muscle, kidney and RBCs. AST activity is increased after myocardial infarction It is elevated in other conditions as: Liver disease: hepatitis, liver cirrhosis, neoplasia Muscle diseases: muscular dystrophy and dermatomyositis LACTATE DEHYDROGENASE (LDH) LDH is a hydrogen transfer enzyme that catalysis the oxidation of L-Lactate to Pyruvate. It is composed of 4 subunits of 2 types M type encoded by a gene on ch 11 H type encoded by a gene on ch 12. There are 5 isoenzymes: LD-1 (4 H subunits) LD-2 (3 H and 1 M sumunits) LD-3 (2 H and 2 M sumunits) LD-4 (1 H and 3 M sumunits) LD-5 (4 M subunits) LDH Both total and LDH isoenzymes are elevated in myocardial injury. Level of LD-1 are elevated 10 – 12 after acute myocardial infarction, peak in 2 days and return to normal in 7 -10 days Usually the amount of LD-2 in the blood is higher than amount of LD-1. Patient with AMI have more LD-1 than LD-2 (ratio > 1) this is called "Flipped Ratio". An elevated level of LD=1 with flipped ratio has a sensitivity and specificity of approximately 75% - 90% for detection of AMI. CREATINE KINASE CK is a dimeric enzyme that regulates high energy phosphate production and utilization in contractile tissues. It is composed of two subunits: M subunit encoded by a gene on chromosome 14. B subunit encoded by a gene on chromosome 19. There are different isoenzymes: CK1 (CK-BB): the predominant isoenzyme found in brain. CK2 (CK-MB): represent 20 – 30 % of total CK in diseased cardiac tissue CK3 (CK-MM): 98% in skeletal muscles and 1% in cardiac muscles. CK-mitochondrial (CK-Mt): located in mitochondria and encoded by a different gene on chromosome 15. Macro-CK: CK complexed with Igs. CREATINE KINASE NORMAL VALUES: Vary according to – age sex race physical condition muscle mass PATHOLOGICAL INCREASES: Myocardial infarction or injury Skeletal muscle injury or disease Hypothyroidism IM injections Generalised convulsions Cerebral injury Malignant hyperpyrexia Prolonged hypothermia CREATINE KINASE: CK-MB In normal population CK-MB < 6% Total CK Sensitive marker with rapid rise & fall: Serum CK-MB levels rise within 2~8 hours after AMI. CK-MB values return to normal 2~3 days after the event. More specific than total CK but has limitations: False elevations in: -perioperative patients without cardiac injury -Skeletal muscle injury -Marathon runners -Chronic renal failure -Hypothyroidism MB Index = (CKMB /total CK) x 100 Combined use with MB Index helps to rule-out patients with skeletal muscle injury CK-MB RELATIVE INDEX AND CKMB mass: MB Index = (CKMB /total CK) x 10 Combined use with MB Index helps to ruleout patients with skeletal muscle injury CK-MB MASS: Measure the concentration of CK-MB protein is now available using sandwich technique with a detection limit < 1µg/dl. More sensitive than measurement of activity. CK-isoforms: Both M and B subunits have N-terminal lysine residues but only M subunit is hydrolyzed by carboxypeptidase-N enzyme found in blood. CK-MM is present in three isoforms: CK-MM3: tissue form. CK-MM2: (one lysine residue is removed). CK-MM1: (both lysine residue are removed) CK-MB has two isoforms: CK-MB2: tissue form. CK-MB1: circulating form. The ratio of tissue isoforms and plasma modified isoforms are used as markers of recent myocardial damage (elevated CK-MM3/CK-MM2 and CK-MB2/CK-MB1/CK-MB1 indicates a rise in tissue isoforms caused by recent release). MYOGLOBIN (Mb) Low MW protein Skeletal & cardiac muscle Mb identical Serum levels increase within 2h of muscle damage Peak at 6 – 9h Normal by 24 – 36h Excellent NEGATIVE predictor of myocardial injury – 2 samples 2 – 4 hours apart with no rise in levels virtually excludes AMI Rapid, quantitative serum immunoassays CARDIAC TROPONINS 1. 2. 3. It consists of 3 subunits troponin C, I, and T. The complex regulates the contraction of striated muscle. TnC binds to calcium ions. TnI binds to actin and inhibits actin-myosin interaction. TnT binds to tropomyosin, attaching to thin filament. THE TROPONIN REGULATORY COMPLEX cTnI cTns 1. Cardiac Troponin I (cTnl) is a cardiac muscle protein with a molecular weight of 24 kiloDaltons. 2. The human cTnl has a additional amino acid residues on its Nterminal that are not exist on the skeletal form. 3. The half life of cTnI is estimated to be 2~4 hours. 4. Serum increase is found between 2-8 hours and returns to normal 7~10 days after AMI. 5. Cardiac TnI levels provide useful prognostic information. 6. Reference range: cTnI <2 ng/ml cTnT 1.Cardiac Troponin T (cTnT) is present in fetal skeletal muscle. 2. In healthy adult skeletal muscle cTnT is absent. 3. The gene of cTnT may be re expressed in skeletal muscle disease. 4. Biological half life and early serum increases of cTnT are similar to that of cTnI. 5. Peak between 12~96 hours and return to normal 14 days after AMI. TROPONIN SUMMARY Regulatory complex of striated muscle contraction Early release ex cytosolic pool Prolonged release due degradation of myofilaments Distinct skeletal & myocardial muscle forms High specificity for myocardial injury Sensitive to minor myocardial damage ISCHAEMIA-MODIFIED ALBUMIN (IMA) Serum albumin is altered by free radicals released from ischaemic tissue Angioplasty studies show that albumin is modified within minutes of the onset of ischaemia. IMA levels rise rapidly, remain elevated for 2-4 h + return to baseline within 6h Clinically may detect reversible myocardial ischaemic damage Not specific (elevated in stroke, some neoplasms, hepatic cirrhosis, end-stage renal disease) Thus potential value is as a negative predictor Spectrophotometric assay for IMA adapted for automated clinical chemistry analysers FDA approved as a rule-out marker in low risk ACS patients (2003) Glycogen phosphorylase BB (GPBB): Glycogen phosphorylase (GP) is a glycolytic enzyme which plays an essential role in the regulation of carbohydrate metabolism. It functions to provide energy supply for muscle contraction Three GP isoenzymes are found in human tissues: o GP-LL in liver o GP-MM in muscle o GP-BB in brain. GP-BB is the predominant isoenzyme in myocardium. With the onset of tissue hypoxia when glycogen is broke down, GP-BB is converted from structurally bound to cytoplasmic form. In AMI GP-BB: Increases 1 – 4 after onset of chest pain Peaks before CK-MB and cTnT Return to reference interval 1 – 2 days after AMI. However it is not cardiac specific. BIOCHEMICAL MARKERS IN ACS: RELEASE, PEAK AND DURATION OF ELEVATION Marker LD-1 Total CK CK-MB CK-MB isoforms cTnI cTnT Myoglobin IMA Duration of elevation 7 – 10 days start Peak 24 – 47 h 3–8h 4–6h 2–3h 48 – 72 h 12 – 30 h 24 h 18 h 6h 24 h 7 – 10 days 6h 2h Few minutes 12 – 48 h 6–7h 2–4h 7 – 10 days 24 h 6h 3 – 4 days 48 – 72 h < 24 h BIOCHEMICAL MARKERS IN ACS: RELEASE, PEAK AND DURATION OF ELEVATION BIOCHEMICAL MARKERS IN ACS UNSTABLE ANGINA PECTORIS (UA) Characterised by chest pain at rest ? Caused by disruption of liquid-filled atherosclerotic plaque with platelet aggregation & thrombus formation Variable degree of ischaemia resulting in reversible or irreversible injury Non-occlusive plaques may produce sufficient ischaemia for release of low molecular weight markers cTnI & cTnT are often elevated in patients with unstable angina pectoris without additional clinical signs (ECG) or classical laboratory signs of acute MI (elevated CK-MB) These patients have a very high risk of cardiac events CARDIAC TROPONINS IN UNSTABLE ANGINA PECTORIS (UA) QUESTION: Does an elevated Troponin level in the absence of other signs reflect irreversible myocardial damage? – – – – Epidemiological studies Animal experiments Clinical trials Sensitive imaging techniques MI must be REDEFINED! Say YES! “ACS REDEFINED” If Troponins are not available, best alternative is CK MBmass Degree of elevation of the marker is related to clinical risk CK(total), AST & LDH (Cardiac Enzymes) should NOT be used! Combine early (myoglobin) & late (Troponins) markers Serial testing: admission, 6 – 9 h, 12 – 24 h An elevated Troponin level in the absence of clinical evidence of ischaemia should prompt searching for other causes of cardiac damage ACS REDEFINED Revised Criteria: Acute/Evolving/ Recent MI Typical myocardial necrosis-associated rise & fall of Troponin or CK-MBmass PLUS One of: – Cardiac Ischaemia symptoms – Q waves on ECG – ST segment changes indicative of ischaemia – Coronary artery imaging (stenosis/obstruction) OR Pathologic findings of an acute MI BIOCHEMICAL MARKERS IN AMI ASSESSMENT OF REPERFUSION “Washout” Marker Level Successful reperfusion Unsuccessful reperfusion phenomenon – enzymes & proteins have direct vascular access when occluded coronary circulation becomes patent Peak concentrations earlier & at higher levels if reperfusion successful Time Due to short plasma half life (t½ = 10 min) Myoglobin is considered the best re-perfusion marker BIOCHEMICAL MARKERS IN ACS CURRENT RECOMMENDATIONS AMI – Routine diagnosis Retrospective diagnosis Skeletal muscle pathology Reinfarction Reperfusion Infarct size Risk stratification in UA Troponins (CK-MBmass) Troponins Troponins Mb, CK-MBmass Mb, Tn, CK-Mbmass Troponins Troponins BIOCHEMICAL MARKERS OF MYOCARDIAL FUNCTION CARDIAC NATRIURETIC PEPTIDES: (ANP, BNP & pro-peptide forms) Family of peptides secreted by cardiac atria (+ ventricles) with potent diuretic, natriuretic & vascular smooth muscle relaxing activity Levels of these neuro-hormonal factors can be measured in blood Clinical usefulness (especially BNP/N-terminal pro-BNP) – Detection of LV dysfunction – Screening for heart disease – Differential diagnosis of dyspnea CARDIOVASCULAR RISK FACTORS ESTABLISHED RISK FACTORS Raised serum low density lipoprotein cholesterol Decreased serum high density lipoprotein cholesterol Smoking High Blood pressure Increased plasma glucose concentrations Physical inactivity Obesity Advanced age EVIDENCE ++ ++ ++ ++ + + + ++ Clear evidence, and modification + of the risk factor decreases the risk of cardiovascular disease EMERGING RISK FACTORS Inflammatory Markers Sensitive C-reactive protein Interleukins Serum amyloid A Pregnancy-associated plasma protein A Chronic infection (Chlamydia pneumoniae, Helicobacter pylori, etc) Procoagulant Markers Plasma Homocysteine Tissue plasminogen activator Plasminogen activator inhibitor Lipoprotein A Process Markers Fibrinogen D-dimer Coronary artery calcification Boersma et al, Lancet, 2003:361,p849 + + + ? ? + + + + + ? ? + Clear evidence, but less clear whether modification of the risk factor decreases the risk of cardiovascular disease ? Risk factor under scrutiny GENETIC ANALYSIS OF CANDIDATE GENES OR RISK FACTORS FOR CARDIOVASCULAR DISEASE Recent explosion of genetic analysis & micro-array technology Common cardiovascular diseases are polygenic. Multiple susceptibility loci interact with lifestyle & environment Single gene defects may account for some of the cardiomyopathies, inherited cardiac arrhythmias Possible genetic cardiovascular risk factors under assessment Technology is still complex & expensive but is developing very rapidly