Pre-hospital Management for Blast Injury
advertisement

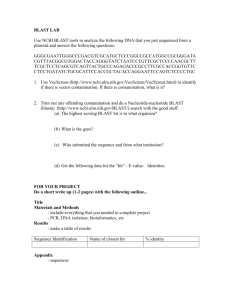
Pre-hospital and Emergency Department Management for Blast Injury Nat Krairojananan MD FRCST Department of Trauma and Emergency Medicine Phramongkutklao Hospital Physics of the explosive • Sudden rapid conversion from chemical component to gas, heat, pressure, light and flame • Low-order explosive devices < 400 m/sec. • High-order explosive devices 1400-9000 m/sec. Type of explosives Manufactured explosives • Military: C4 • Industrial: TNT Type of explosives Improvise Explosive Devices (IED) • Pipe bomb • ANFO (Ammonium Nitrate Fuel Oil) Factors influence severity of injuries • • • • Size and amount of explosive Distance from the detonation Media (air VS water) Detonation in the closed space Blast injury categorization Primary blast injury Secondary blast injury Tertiary blast injury Quaternary blast injury Quinary blast injury Primary blast injury • Caused by high order explosive only • Over pressure to air-filled organs • • • • • Blast lung: PTX, pulmonary contusion, PE Blast bowel: ruptured hollow viscus peritonitis Blast ear: TM perforation Blast brain: concussion Blast eye Secondary blast injury • Penetrating injury/ laceration • Fragmentation of case/shell or Shrapnel • Secondary fragment Secondary blast injury Tertiary blast injury • • • • • Blast wave Propulsion of body onto hard surface Propulsion of object onto individuals Structural collapsed Fall from height • Blunt injury • crush syndrome • compartment syndrome Quaternary blast injury Not caused by primary, secondary or tertiary blast injury • Fire (burn) • Inhalation injury • Asphyxia Quinary blast injury • • • • Toxic fume Chemical injury Radiation Biological agents Part I Scene Management For EMS personnel Scene management • • • • Scene sized up (scene safety) Scene triage Scene treatment Evacuation ICS in bombing event • • • • • Commander Security Search and rescue Treatment team Evacuation team Scene sized up Recognition of specific hazards with bombing • • • • Secondary device Environmental hazards (fires, toxin) Structural instability Other threat; sniper Safe distance? Scene Triage • MASS triage • START triage MASS Triage M: Move A: Assess S: Sort S: Send • Presence of threat MOVE • • • • Quickly evacuate all patients from scene Move unresponsive patients first Use of appropriate stabilization and equipment Stretcher or SKED MASS triage ASSESS • According to Pre-Hospital Trauma Life Support (PHTLS) protocol by assess life threatening injury first Abv. Extend Action A Airway and C-spine protection Open & clear airway, C-collar B Breathing (chest injury) O2 supplement by face mask with bag, Rx for tension PTX C Circulation (hemorrhagic shock) Stop bleeding, initiate iv fluid D Disability (neurologic status) Check A-V-P-U E Environmental control Keep warm MASS triage SORT Categorize and tag patients into groups for Rx and evacuation Color code RED-immediate Severity Life threatening injury Type of injuries - Airway obstruction - Chest injury - Hemorrhagic shock YELLOW-delayed - Potential life threatening - Fracture - Limb threatening injury - mild abdominal injury - PTSD* GREEN-minimal Minor injury Wounds BLACK or BLUE Expectant Obvious signs of death - Severe injury - Extensive wounds MASS triage SEND • • • • Expedient patients to appropriate resources Trauma center En route care: monitors Proper stabilization MASS triage START Triage Simple Triage And Rapid Treatment START triage Scene Sized up Ask patients to walk to your voice Unable to walk Able to walk Ask patients to raise hand or leg GREEN (minimal) Walk to assigned area START Triage (cont.) Ask patient to raise hand or leg No response Assess breathing Breathing 5 /min or more Obey command No breathing YELLOW BLACK or BLUE RED Delayed Rx possibility Supportive treatment with limited resources Immediate AW treatment Initial management • Treat life threatening injuries • Prevent disability Abv. Extend Action A Airway and C-spine protection Open & clear airway, C-collar B Breathing (chest injury) O2 supplement by face mask with bag, Rx for tension PTX C Circulation (hemorrhagic shock) Stop bleeding, initiate iv fluid D Disability (neurologic status) Check A-V-P-U E Environmental control Keep warm START triage Evacuation • • • • Expedient patients to appropriate resources Trauma center En route care: monitors Proper stabilization START triage Part II Emergency Department Management For clinicians, nurses Emergency department management • Triage and Patient categorization • Treatment zones by color code • follow Advance Trauma Life Support (ATLS) protocol Primary blast injury treatment System Blast lung CXR in all cases* Blast GI Possible injury Immediate Rx consultation Tension PTX Needle thoracocentesis, follow by ICD insertion and support ventilation - Trauma surgeon - CVT surgeon Air embolism Support ventilation Intensivist Pulmonary contusion Support ventilation Intensivist Intra abdominal bleeding iv fluid infusion, investigation Trauma surgeon Bowel perforation Investigation, observe Trauma surgeon Blast brain Brain concussion, ICH Check GCS, lateralizing sign Blast ear TM perforation Ear exam in all cases Blast eye Globe rupture Eye examination Neurosurgeon ENT Opthalmologist Secondary blast injury treatment Injury Immediate Rx Definitive Rx consultation Explore lap. Trauma surgeon Penetrating injury - Bleeding control - iv fluid replacement - Film for foreign body Amputation - Bleeding control - Tourniquet if necessary - iv fluid replacement Surgical - Trauma surgeon debridement - Orthopedist and control bleeding Laceration - Bleeding control - iv fluid replacement - Film for foreign body Debridement and suture Opened fracture - Immobilization - Distal neurovascular check - Debridement - Bone realignment Trauma surgeon Orthopedist Tertiary blast injury treatment Injury Blunt chest / abdominal injury Immediate Rx Definitive Rx consultation - Bleeding control - iv fluid replacement - FAST / DPL Explore lap. Trauma surgeon Crush syndrome - iv fluid load to force diuresis - Alkalinize urine - ECG monitoring - Dialysis if necessary - Looking for compartment syndrome Trauma surgeon Compartment syndrome - Trauma surgeon - Orthopedist Fasciotomy Quaternary blast injury treatment Injury Immediate Rx Inhalation injury - Airway management - Oxygen supplement Asphyxia - Airway management - Oxygen supplement Burn - Keep warm - Wound care - iv fluid resuscitation Definitive Rx - Wound debridement - Grafting for skin coverage Quinary blast injury treatment Injury Immediate Rx Definitive Rx Toxic fume Airway and ventilation support Antidote? Chemical injury Decontamination Wound care Radiation Supportive treatment same Biological agents - Isolation - Medical personnel PPE Antibiotics ? Special consideration • ‘upside down’ or ‘reverse’ triage • Estimated incoming patient Total number of patient = Number in first hour x 2 Special consideration CBRNE event • Decontamination • Personal Protective Equipment EMS personnel preparation Decontaminating station Thank you Comments and question are welcome Three suspected