obesity paradox
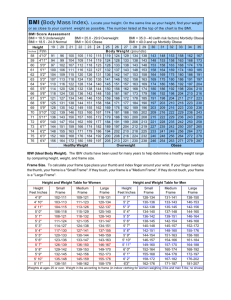
advertisement

Obesity and cardiovascular disease Risk factor,paradox and impact of weight loss Obesity has reached global epidemic proportions in both adults and children and is associated with numerous comorbidities, including hypertension (HTN), type II diabetes mellitus, dyslipidemia, obstructive sleep apnea and sleep-disordered breathing, certain cancers, and major cardiovascular (CV) diseases. Because of its maladaptive effects on various CV risk factors and its adverse effects on CV structure and function, obesity has a major impact on CV diseases, such as heart failure (HF) , coronary heart disease (CHD) , sudden cardiac death, and atrial fibrillation, and is associated with reduced overall survival. Recent evidence indicates that obesity is associated with more morbidity than smoking, alcoholism, and poverty, and if current trends continue, obesity may soon overtake cigarette abuse as the leading cause of preventable death in the world. Adverse Effects of Obesity A. Increases in insulin resistance 1) Glucose intolerance 2) Metabolic syndrome 3) Type 2 diabetes mellitus B. Hypertension C. Dyslipidemia 1) Elevated total cholesterol 2) Elevated triglycerides 3) Elevated LDL cholesterol 4) Elevated non-HDL cholesterol 5) Elevated apolipoprotein-B 6) Elevated small, dense LDL particles 7) Decreased HDL cholesterol 8) Decreased apolipoprotein-A1 D. Abnormal left ventricular geometry 1) Concentric remodeling 2) Left ventricular hypertrophy E. Endothelial dysfunction F. Increased systemic inflammation and prothrombotic state G. Systolic and diastolic dysfunction H. Heart failure I. Coronary heart disease J. Atrial fibrillation K. Obstructive sleep apnea/sleep-disordered breathing L. Albuminuria M. Osteoarthritis N. Cancers Despite this adverse association, numerous studies have documented an obesity paradox in which overweight and obese people with established CV disease, including HTN, HF, CHD, and peripheral arterial disease, have a better prognosis compared with nonoverweight/ nonobese patients. Obesity, HTN, and the obesity paradox METHODS: A total of 22,576 hypertensive patients with coronary artery disease (follow up 61,835 patient years, mean age 66±9.8 years) were randomized to blood pressure control according to the Sixth JNC targets. Patients were classified into 5 groups according to baseline BMI: less than 20 kg/m2 (thin), 20 to 25 kg/m2 (normal weight), 25 to 30 kg/m2(overweight), 30 to 35 kg/m2 (class I obesity), and 35 kg/m2 or more (class II-III obesity). The primary outcome was first occurrence of death, nonfatal myocardial infarction, or nonfatal stroke. RESULTS: With patients of normal weight (BMI 20 to 25 kg/m2) as the reference group, the risk of primary outcome was lower in the overweight patients (adjusted hazard ratio [HR] 0.77, 95% confidence interval [CI], 0.70-0.86, P<.001), class I obese patients (adjusted HR 0.68, 95% CI, 0.59-0.78, P<.001), and class II to III obese patients (adjusted HR 0.76, 95% CI, 0.65-0.88, P <.001). Class I obese patients had the lowest rate of primary outcome and death despite having smaller blood pressure reduction compared with patients of normal weight at 24 months (17.5±21.9 mm Hg/9.8±12.4 mm Hg vs 20.7±23.1 mm Hg / 10.6±12.5 mm Hg, P<.001). CONCLUSION: In a population with hypertension and coronary artery disease, overweight and obese patients had a decreased risk of primary outcome compared with patients of normal weight, which was driven primarily by a decreased risk of all-cause mortality. Body mass index and prognosis in elderly hypertensive patients: a report from the European Working Party on High Blood Pressure in the Elderly Jaakko Tuomilehto, M.D., European Working Party on High Blood Pressure ∗ Department of Epidemiology, National Public Health Institute, Helsinki, Finland In the current study of 800 elderly hypertensive patients randomly assigned to active treatment, the initial mean body mass index (BMI) was 26.7 kg/m2 in 560 women and 25.7 kg/m2 in 240 men. During the trial, total mortality and cardiovascular and noncardiovascular terminating events were highest in the patients at the leanest BMI quintile. The association between BMI and cardiovascular end points was U-shaped, whereas noncardiovascular mortality decreased with increasing BMI. The results in the women were similar to those in the total group. The U-shaped relation was confirmed with Cox's proportional hazards model, controlling for age, gender, systolic blood pressure, hemoglobin, serum cholesterol, blood glucose, and cardiovascular complications at entry. The BMI level with the lowest risk was 28 to 29 kg/m2 for total mortality and cardiovascular terminating events, 26 to 27 kg/m2 for cardiovascular mortality, and 31 to 32 kg/m2 for noncardiovascular mortality. BMI did not modify the favorable effects of drug treatment. Obesity, HF, and the obesity paradox. Body mass index and mortality in heart failure: A meta-analysis Antigone Oreopoulos, MSca, Raj Padwal, MD, MScb, , , Kamyar Kalantar-Zadeh, MD, MPH, PhDc, Gregg C. Fonarow, MD, FACCd, Colleen M. Norris, PhDe, Finlay A. McAlister, MD, MScb American Heart Journal Volume 156, Issue 1, July 2008, Pages 13–22 Background: In patients with chronic heart failure (CHF), previous studies have reported reduced mortality rates in patients with increased body mass index (BMI). The potentially protective effect of increased BMI in CHF has been termed the obesity paradox or reverse epidemiology. This meta-analysis was conducted to examine the relationship between increased BMI and mortality in patients with CHF. Methods: We searched the Cochrane Central Register of Controlled Trials, MEDLINE, EMBASE, Scopus, and Web of Science to identify studies with contemporaneous control groups (cohort, case-control, or randomized controlled trials) that examined the effect of obesity on all-cause and cardiovascular mortality. Two reviewers independently assessed studies for inclusion and performed data extraction. Results: Nine observational studies met final inclusion criteria (total n = 28,209). Mean length of follow-up was 2.7 years. Compared to individuals without elevated BMI levels, both overweight (BMI ∼25.0-29.9 kg/m2, RR 0.84, 95% CI 0.79-0.90) and obesity (BMI ∼≥30 kg/m2, RR 0.67, 95% CI 0.62-0.73) were associated with lower all-cause mortality. Overweight (RR 0.81, 95% CI 0.72-0.92) and obesity (RR 0.60, 95% CI 0.53-0.69) were also associated with lower cardiovascular mortality. In a risk-adjusted sensitivity analysis, both obesity (adjusted HR 0.88, 95% CI 0.83-0.93) and overweight (adjusted HR 0.93, 95% CI 0.89-0.97) remained protective against mortality. Conclusions: Overweight and obesity were associated with lower allcause and cardiovascular mortality rates in patients with CHF and were not associated with increased mortality in any study. An obesity paradox in acute heart failure: Analysis of body mass index and inhospital mortality for 108 927 patients in the Acute Decompensated Heart Failure National Registry Gregg C. Fonarow, MDa, , , Preethi Srikanthan, MDa, Maria Rosa Costanzo, MDb, Guillermo B. Cintron, MDc, Margarita Lopatin, MSd, for the ADHERE Scientific Advisory Committee and Investigators American Heart Journal Volume 153, Issue 1, January 2007, Pages 74–8 Methods: The Acute Decompensated Heart Failure National Registry was analyzed for acute HF hospitalizations in 263 hospitals in the United States from October 2001 through December 2004. Patients with documented height and weight were divided into BMI (measured in kilograms per square meter) quartiles. In hospital mortality by BMI quartile for all the patients and for those with reduced (n = 43 255) and preserved (n = 37 901) systolic function was assessed. Results: Body mass index quartiles in the 108 927 hospitalizations were QI (16.0-23.6 kg/m2), QII (23.7-27.7 kg/m2), QIII (27.8-33.3 kg/m2), and QIV (33.4-60.0 kg/m2). Patients in the higher BMI quartiles were younger, had more diabetes, and had a higher left ventricular ejection fraction. In hospital mortality rates decreased in a near-linear fashion across successively higher BMI quartiles. After adjustments for age, sex, blood urea nitrogen, blood pressure, creatinine, sodium, heart rate, and dyspnea at rest, BMI quartile still predicted mortality risk. For every 5-U increase in BMI, the odds of risk-adjusted mortality was 10% lower (95% CI 0.88-0.93, P < .0001). Obesity, CHD, and the obesity paradox Obesity plays a major role in adversely affecting major CHD risk factors, including HTN, dyslipidemia, and diabetes mellitus (DM), is the major component of metabolic syndrome, and is probably an independent risk factor for atherosclerosis and CHD events. Nevertheless, as with HTN and HF, many studies have also reported an obesity paradox in CHD, including in patients treated with revascularization. Association of bodyweight with total mortality and with cardiovascular events in coronary artery disease: a systematic review of cohort studies Abel Romero-Corral, MD, Victor M Montori, MD, Prof Virend K Somers, MD, Josef Korinek, MD, Randal J Thomas, MD, Thomas G Allison, PhD, Farouk Mookadam, MD, Francisco Lopez-Jimenez, MD. The LANCET Volume 368, Issue 9536, 19–25 August 2006, Pages 666–678 Methods: We selected cohort studies that provided risk estimates for total mortality, with or without cardiovascular events, on the basis of bodyweight or obesity measures in patients with CAD, and with at least 6 months' follow-up. CAD was defined as history of percutaneous coronary intervention, coronary artery bypass graft, or myocardial infarction. We obtained risk estimates for five predetermined bodyweight groups: low, normal weight (reference), overweight, obese, and severely obese. Findings: There were 40 studies with 250,152 patients that had a mean follow-up of 3·8 years. Patients with a low body-mass index (BMI) (ie, <20) had an increased relative risk (RR) for total mortality (RR=1·37 [95% CI 1·32–1·43), and cardiovascular mortality (1·45 [1·16–1·81]), overweight (BMI 25–29.9) had the lowest risk for total mortality (0·87 [0·81–0·94]) and cardiovascular mortality (0·88 [0·75–1·02]) compared with those for people with a normal BMI. Obese patients (BMI 30– 35) had no increased risk for total mortality (0·93 [0·85–1·03]) or cardiovascular mortality (0·97 [0·82–1·15]). Patients with severe obesity (≥35) did not have increased total mortality (1·10 [0·87–1·41]) but they had the highest risk for cardiovascular mortality (1·88 [1·05–3·34]). Objectives: This study goal was to determine the impact of lean mass index (LMI) and body fat (BF) on survival in patients with coronary heart disease (CHD). Methods : We studied 570 consecutive patients with CHD who were referred to cardiac rehabilitation, stratified as Low (25% in men and 35% in women) and High (25% in men and 35% in women) BF and as Low (18.9 kg/m2 in men and 15.4 kg/m2 in women) and High LMI, and followed for 3 years for survival. Results: Mortality is inversely related to LMI (p ‹ 0.0001). Mortality was highest in the Low BF/Low LMI group (15%), which was significantly higher than in the other 3 groups, and lowest in the High BF/High LMI group (2.2%), which was significantly lower than in the other 3 groups. In Cox regression analysis as categoric variables, low LMI (hazard ratio [HR]: 3.1; 95% confidence interval [CI]: 1.3 to 7.1) and low BF (HR: 2.6; 95% CI: 1.1 to 6.4) predicted higher mortality, and as continuous variables, high BF (HR: 0.91; 95% CI: 0.85 to 0.97) and high LMI (HR: 0.81; 95% CI: 0.65 to 1.00) predicted lower mortality. Conclusions: In patients with stable CHD, both LMI and BF predict mortality, with mortality particularly high in those with Low LMI/Low BF and lowest in those with High LMI/High BF. Determination of optimal body composition in primary and secondary CHD prevention is needed. The aim of this study was to investigate the impact of morbid obesity (body mass index ≥40 kg/m2) on inhospital mortality and coronary revascularization outcomes in patients presenting with acute myocardial infarctions (AMI). 413,673 patients hospitalized with AMIs in 2009 were reviewed. Morbidly obese patients constituted 3.7% of all patients with AMIs. Analysis of the unadjusted data revealed that morbidly obese patients compared with those not morbidly obese were more likely to undergo any invasive cardiac procedures when presenting with either ST-segment elevation myocardial infarction (97.4% vs 93.8%, p <0.0001) or noneST-segment elevation myocardial infarction (85.5% vs 80.6%, p <0.0001). The unadjusted mortality rate for morbidly obese patients with AMIs was 3.5%, compared with 5.5% of those not obese (p <0.0001). After adjustment, lower odds of mortality in those morbidly obese compared to those not morbidly remained. In conclusion, patients with morbid obesity had lower odds of in-hospital mortality, compared to those not morbidly obese, consistent with the phenomenon of the “obesity paradox.” BACKGROUND: An “obesity paradox,” in which overweight and obese individuals with established cardiovascular disease have a better prognosis than normal weight subjects, has been reported in a number of clinical cohorts, but little is known about the effects of weight loss on the obesity paradox and its association with health outcomes. METHODS: Weight was determined in 3834 men at the time of a clinically referred exercise test and again during a clinical evaluation a mean of 7 years later. The associations among weight changes, baseline fitness, and other risk markers with cardiovascular and all cause mortality were determined by Cox proportional hazards analysis. RESULTS: During the follow-up period, 314 subjects died (72 of cardiovascular causes). In a multivariate analysis (including baseline weight, weight change, exercise capacity, and cardiovascular disease), weight gain was associated with lower mortality and weight loss was associated with higher mortality (4% higher per pound lost per year, P.001) compared with stable weight. For all-cause mortality, the relative risks for the no change, weight gain, and weight loss groups were 1.0 (referent), 0.64 (95% confidence interval, 0.50-0.83), and 1.49 (95% confidence interval, 1.17-1.89), respectively (P.001). Those who died and exhibited weight loss had a significantly higher prevalence of deaths due to cancer and cardiovascular causes. CONCLUSION: Weight loss was related to higher mortality and weight gain was related to lower mortality when compared with stable weight. background: We sought to investigate the impact of body mass index (BMI) on long-term all-cause mortality in patients following first-time elective percutaneous coronary intervention (PCI). They used the Scottish Coronary Revascularisation Register to undertake a cohort study of all patients undergoing elective PCI in Scotland between April 1997 and March 2006 inclusive. they excluded patients who had previously undergone revascularization. There were 219 deaths within 5 years of 4880 procedures. Compared with normal weight individuals, those with a BMI 27.5 and ,30 were at reduced risk of dying (HR 0.59, 95% CI 0.39–0.90, 95%, P : 0.014). There was no attenuation of the association after adjustment for potential confounders, including age, hypertension, diabetes, and left ventricular function (adjusted HR 0.59, 95% CI 0.39–0.90, P : 0.015), and there were no statistically significant interactions. The results were unaltered by restricting the analysis to events beyond 30 days of follow-up. Among patients undergoing percutaneous intervention for coronary artery disease, increased BMI was associated with improved 5 year survival. OBJECTIVE: To find out the severity of coronary atherosclerosis and its relationship to body structure and adiposity in severely obese people with body mass index (BMI) ≥35.0 kg/m2 and to examine the incidence and characteristic features of myocardial infarction and other fatal coronary events in this population. SUBJECTS: Forensic autopsy cases (n =166) with a BMI ≥35.0 kg/m2 examined in 1992 – 1998 were collected from the files of the Department of Forensic Medicine, University of Oulu, Finland. DESIGN: Autopsy reports were analyzed, including data on age, height, weight, abdominal subcutaneous fat thickness, heart weight, coronary atherosclerosis, histopathology and toxicology. Myocardial collagen and arteriolar structure were examined by computerized image analysis. RESULTS: In a large number of the severely obese individuals, the coronary arteries were either lesion-free or only fatty streaks were observed (38% of men, 44% of women) and coronary thrombosis was rare (3.8% of men and 1.6% of women). Cardiac causes of death predominated, cardiomyopathy being the commonest. Myocardial infarction was the immediate cause of death in 14.4% of men and 12.9% of the women, and it was associated with increased heart size in men. Coronary atherosclerosis without any infarction had been determined as the cause of death in 8.6% of the men and 8.1% of the women. Abdominal subcutaneous fat thickness had a significant negative association with the severity of coronary atherosclerosis in the women, and a decrease in the arteriolar media=lumen ratio with increasing BMI was observed in the men. CONCLUSIONS: A considerable number of severely obese people have only fatty streaks and no marked stenosis in their coronary arteries, even at an advanced age. The large amounts of subcutaneous adipose tissue in obese women may provide some protection against coronary lesion development, which could be an estrogen effect. Myocardial infarction in severely obese men is associated with cardiac hypertrophy. From 409 United States hospitals, 130,139 hospitalizations for CAD were identified with documented height and weight. Patients were stratified by BMI, with 3,305 (2.5%) underweight (BMI <18.5 kg/m2), 34,697 (27%) of healthy weight (BMI 18.5 to 24.9 kg/m2), 47,883 (37%) overweight (BMI 25 to 29.9 kg/m2), 37,686 (29%) obese (BMI 30 to 39.9 kg/m2), and 6,568 (5%) extremely obese (BMI >40 kg/m2). As BMI increased, patients were significantly younger but more likely to be men and have hypertension, diabetes, and hyperlipidemia. Unadjusted in-hospital mortality was highest in the underweight group (10.4%) and significantly lower in the healthy weight (5.4%), overweight (3.1%), obese (2.4%), and extremely obese (2.9%) patients. Higher BMI was associated with increased use of standard medical therapies such as aspirin, blockers, inhibitors of the renin-angiotensin system, and lipidlowering therapy in the hospital and at discharge. In adjusted analyses, compared with the healthy-weight group, overweight and obese patients were more likely to undergo invasive procedures and had lower mortality (p <0.01 for all odds ratios). In conclusion, increasing BMI appears to be associated with better use of guideline-recommended medical treatment and invasive management of CAD, which may explain the observed lower rates of in-hospital mortality. Methods: We assessed 105 consecutive PH patients for clinical and hemodynamic parameters, focusing on the possible association between Body Mass Index (BMI) and mortality. Follow-up period was 19 ±13 months. Results: Sixty-one patients (58%) had pre-capillary PH and 39 patients (37%) out-of-proportion post-capillary PH. During follow-up period, 30 patients (29%) died. Death was associated with reduced functional-class, inverse-relation with BMI, higher pulmonary artery and right atrial pressures, pulmonary vascular resistance and signs of right ventricular failure. In multivariate analysis, obesity (BMI 30 kg/m2), was the variable most significantly correlated with improved survival [H.R 0.2, 95% C.I 0.1e0.6; p = 0.004], even after adjustment for baseline characteristics. Obese and very-obese (BMI ≥ 35 kg/m2) patients had significantly less mortality rates during follow-up (12% and 8%, respectively) than nonobese patients (41%), p = 0.01. Obesity paradox Background: Most studies that have evaluated the association between the body-mass index (BMI) and the risks of death from any cause and from specific causes have been conducted in populations of European origin. Methods: We performed pooled analyses to evaluate the association between BMI and the risk of death among more than 1.1 million persons recruited in 19 cohorts in Asia. The analyses included approximately 120,700 deaths that occurred during a mean follow-up period of 9.2 years. Results: In the cohorts of East Asians, including Chinese, Japanese, and Koreans, the lowest risk of death was seen among persons with a BMI (the weight in kilograms divided by the square of the height in meters) in the range of 22.6 to 27.5. The risk was elevated among persons with BMI levels either higher or lower than that range — by a factor of up to 1.5 among those with a BMI of more than 35.0 and by a factor of 2.8 among those with a BMI of 15.0 or less. A similar U-shaped association was seen between BMI and the risks of death from cancer, from cardiovascular diseases, and from other causes. Background: Weight loss is associated with short-term amelioration and prevention of metabolic and cardiovascular risk, but whether these benefits persist over time is unknown. Methods: The prospective, controlled Swedish Obese Subjects Study involved obese subjects who underwent gastric surgery and contemporaneously matched, conventionally treated obese control subjects. We now report follow-up data for subjects (mean age, 48 years; mean body-mass index, 41) who had been enrolled for at least 2 years (4047 subjects) or 10 years (1703 subjects) before the analysis (January 1, 2004). The follow-up rate for laboratory examinations was 86.6 percent at 2 years and 74.5 percent at 10 years. Results: After two years, the weight had increased by 0.1 percent in the control group and had decreased by 23.4 percent in the surgery group (P<0.001). After 10 years, the weight had increased by 1.6 percent and decreased by 16.1 percent, respectively (P<0.001). Energy intake was lower and the proportion of physically active subjects higher in the surgery group than in the control group throughout the observation period. Two- and 10-year rates of recovery from diabetes, hypertriglyceridemia, low levels of highdensity lipoprotein cholesterol, hypertension, and hyperuricemia were more favorable in the surgery group than in the control group, whereas recovery from hypercholesterolemia did not differ between the groups. The surgery group had lower 2- and 10-year incidence rates of diabetes, hypertriglyceridemia, and hyperuricemia than the control group; differences between the groups in the incidence of hypercholesterolemia and hypertension were undetectable. conclusions As compared with conventional therapy, bariatric surgery appears to be a viable option for the treatment of severe obesity, resulting in long-term weight loss, improved lifestyle, and, except for hypercholesterolemia, amelioration in risk factors that were elevated at baseline. Background: Although gastric bypass surgery accounts for 80% of bariatric surgery in the United States, only limited long-term data are available on mortality among patients who have undergone this procedure as compared with severely obese persons from a general population. Methods: In this retrospective cohort study, we determined the long-term mortality (from 1984 to 2002) among 9949 patients who had undergone gastric bypass surgery and 9628 severely obese persons who applied for driver’s licenses. From these subjects, 7925 surgical patients and 7925 severely obese control subjects were matched for age, sex, and body-mass index. We determined the rates of death from any cause and from specific causes with the use of the National Death Index. Results: During a mean follow-up of 7.1 years, adjusted long-term mortality from any cause in the surgery group decreased by 40%, as compared with that in the control group (37.6 vs. 57.1 deaths per 10,000 person-years, P<0.001); cause-specific mortality in the surgery group decreased by 56% for coronary artery disease (2.6 vs. 5.9 per 10,000 person-years, P = 0.006), by 92% for diabetes (0.4 vs. 3.4 per 10,000 person-years, P = 0.005), and by 60% for cancer (5.5 vs. 13.3 per 10,000 person-years, P<0.001). However, rates of death not caused by disease, such as accidents and suicide, were 58% higher in the surgery group than in the control group (11.1 vs. 6.4 per 10,000 person-years, P = 0.04). Conclusions Long-term total mortality after gastric bypass surgery was significantly reduced, particularly deaths from diabetes, heart disease, and cancer. However, the rate of death from causes other than disease was higher in the surgery group than in the control group. Background: Obesity is associated with increased mortality. Weight loss improves cardiovascular risk factors, but no prospective interventional studies have reported whether weight loss decreases overall mortality. In fact, many observational studies suggest that weight reduction is associated with increased mortality. Methods: The prospective, controlled Swedish Obese Subjects study involved 4047 obese subjects. Of these subjects, 2010 underwent bariatric surgery (surgery group) and 2037 received conventional treatment (matched control group). We report on overall mortality during an average of 10.9 years of follow-up. At the time of the analysis (November 1, 2005), vital status was known for all but three subjects (follow-up rate, 99.9%). Results: The average weight change in control subjects was less than ±2% during the period of up to 15 years during which weights were recorded. Maximum weight losses in the surgical subgroups were observed after 1 to 2 years: gastric bypass, 32%; verticalbanded gastroplasty, 25%; and banding, 20%. After 10 years, the weight losses from baseline were stabilized at 25%, 16%, and 14%, respectively. There were 129 deaths in the control group and 101 deaths in the surgery group. The unadjusted overall hazard ratio was 0.76 in the surgery group (P = 0.04), as compared with the control group, and the hazard ratio adjusted for sex, age, and risk factors was 0.71 (P = 0.01). The most common causes of death were myocardial infarction (control group, 25 subjects; surgery group, 13 subjects) and cancer (control group, 47; surgery group, 29). Conclusions: Bariatric surgery for severe obesity is associated with long-term weight loss and decreased overall mortality. No obesity paradox for morbid obese patients Methods: We examined the prevalence of morbid obesity (body mass index [BMI] 40 kg/m2) among 227,044 patients undergoing PCI and enrolled in the Blue Cross Blue Shield of Michigan Cardiovascular Consortium registry from 1998 to 2009. Results : The proportion of morbidly obese patients undergoing PCI increased from 4.38% in 1998 to 8.36% in 2009. Compared with overweight patients (BMI 25 to 30 kg/m2), these patients had significantly increased vascular complications (adjusted odds ratio [OR]: 1.31; 95% CI: 1.17 to 1.47; p < 0.0001), contrast-induced nephropathy (adjusted OR: 1.89; 95% CI: 1.70 to 2.11; p < 0.0001), nephropathy requiring dialysis (adjusted OR: 4.08; 95% CI: 2.98 to 5.59; p < 0.0001), and mortality (adjusted OR: 1.63; 95% CI: 1.33 to 2.00; p < 0.0001).