Surgeon controlled factor - Orthopaedic Trauma Association
advertisement

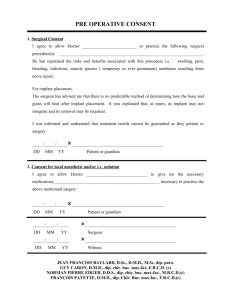
Intertrochanteric Fractures Presenter: Please look at notes to facilitate your talk— There is too much content for one sitting -edit to your needs— Unanswered clinical issues and audience questions at end of lecture Michael R. Baumgaertner, MD Original Authors: Steve Morgan, MD; March 2004; New Author: Michael R. Baumgaertner, MD; Revised January 2007 Revised December 2010 Lecture Objectives Review: Principles of treatment Understand & Optimize Variables influencing patient and fracture outcome Introduce: Recent Evidence- based med Suggest: Surgical Tips to avoid common problems Hip Fracture PATIENT Outcome Predictors Pre-injury physical & cognitive status Ability to visit a friend or go shopping Presence of home companion Postoperative ambulation Postoperative complications (Cedar, Thorngren, Parker, others) A public heath care cri$i$: 130,000 IT Fx / year in U.S. & will double by 2050… 4-12% fixation failure Even when surgery is “successful”: 1-2 units PRBC transfused 3-5+ days length of stay We must do better!! Preoperative Management the evidence suggests: “Tune up” correctable comorbidities Operate within 48°; avoid night surgery Zuckerman, JBJS(A) ‘95 Maintain extremity in position of comfort Buck’s traction of no value (RCT) Anderson, JBJS(B) ‘93 General versus spinal anaesthesia? Randomized, prospective trials (RCTs): no difference Davis, Anaesth & IntCare ‘81; Valentin, Br J Anaesth ‘86 Comprehensive Management excellent evidence based single source: Osteoporosis International “Preoperative Guidelines and Care Models for Hip Fractures” Volume 21, Supplement 4 December 2010 Intertrochanteric Femur Anatomic considerations Capsule inserts on IT line anteriorly, but at midcervical level posteriorly Muscle attachments determine deformity Radiographs Plain Films AP pelvis Cross-table lateral ER Traction view when in any doubt!! Factors Influencing Construct Strength: Uncontrolled factors Bone Quality Fracture Geometry Controlled factors Quality of Reduction Implant Placement Implant Selection Kaufer, CORR 1980 This lecture will examine each factor Uncontrolled factor: Fracture geometry “STABILITY” The ability of the reduced fracture to support physiologic loading Fracture Stability relates not only to the # of fragments but the fracture plane as well 31 AO / OTA Uncontrolled factor: Fracture geometry Stable Unstable Uncontrolled factor: Fracture geometry AO/OTA31A3: The highly unstable “pertrochanteric” fractures! Uncontrolled factor: Bone quality A 33 year old pt with intertrochanteric fracture following a fall from heightNote the dense, cancellous bone throughout the proximal femur; Not at all like a geriatric fracture Uncontrolled factor: Bone quality 83 yo white woman with unstable intertrochanteric fracture: Note the marked loss of trabeculae Uncontrolled factor: Bone quality Implants must be placed where the remaining trabeculae reside! Uncontrolled factor: Bone quality Can / Should we strengthen the bone-implant interface? PMMA 12 to 37% increase load to failure Choueka, Koval et al., ActaOrthop ‘96 CPPC 15% increased yield strength, stiffer Moore, Goldstein, et al., JOT ‘97 Elder, Goulet, et al., JOT ‘00 Clinical Factors in 2010 influence use delivery, cost, complications must be considered Hydroxy-apatite (HA) coated screws Reduced cut out in poorly positioned fixation Moroni, et al. CORR ‘04 Factors Influencing Construct Strength: Uncontrolled factors Fracture Geometry Bone Quality Surgeon controlled factors Quality of Reduction Implant Placement Implant Selection Kaufer, CORR ‘80 Kauffer, CORR 1980 Surgeon controlled factor Fracture Reduction When employing sliding hip screws… No role for displacement osteotomy RCT Desjardins, et al. JBJS (B) ‘93 RCT Gargan, et al. JBJS (B) ‘94 Limited role for reduction & fixation of trochanteric fragments (biology vs stability) Surgical goal: Biplanar, anatomic alignment of proximal & shaft fragments Mild valgus reduction for hinstability to offset shortening Surgeon controlled factor Fracture Reduction Discuss sequence of closed reduction steps Consider adjuncts to fracture reduction Crutch… elevator… joystick…. etc. Lever technique– read this article: Surgeon controlled factor Fracture of Reduction Double density of medial cortex is evidence of intussuscepted neck into shaft seen on lateral Traction will not reduce this “sag” but a lever into the fracture will Traction will not reduce this “sag” but a lever into the fracture will reduce it Surgeon controlled factor Fracture Reduction The AP view before and after lever redution: the medial cortex is restored Surgeon controlled factor: Implant position Apex of the femoral head Defined as the point where a line parallel to, and in the middle of the femoral neck intersects the joint Surgeon controlled factor: Implant position Screw Position: TAD Xap Tip-Apex Distance = Xlat Xap + Xlat Surgeon controlled factor: Implant position Baumgaertner, Curtin, Lindskog, Keggi JBJS (A) ‘95 Surgeon controlled factor: Implant position Probability of Cut Out Increasing TAD -> Baumgaertner, Curtin, Lindskog, Keggi JBJS (A) ‘95 Surgeon controlled factor: Implant position Logistic Regression Analysis Multivariate (dependent variable:Cut Out) Reduction Quality p = 0.6 Screw Zone p = 0.6 Unstable Fracture p = 0.03 Increasing Age Increasing TAD p = 0.0002 p = 0.002 Baumgaertner, Curtin, Lindskog, Keggi JBJS (A) ‘95 Surgeon controlled factor: Implant position Optimal Screw Placement Dead Center and Very Deep (TAD<25mm) Best bone No moment arm for rotational instability Maximum slide Validates reduction Surgeon controlled factor: Implant selection What’s the big deal? IM vs Plate Fixation IM Fixation Recent History: Theoretical Biologic Advantages Percutaneous Procedure EBL, Muscle stripping, Complications, Rehab time? Surgical wounds s/p ORIF with IM device GAMMA The First to Reach the Market Gamma Clinical Results Advantages : ± Complications : Bridle JBJS(B) '91 Boriani Orthopaedics '91 Lindsey Trauma '91 Halder JBJS(B) '92 +++ Williams Injury '92 LeungJBJS(B) '92 Aune ActOrthopScan '94 Surgeon controlled factor: Implant selection Gamma Nail vs. CHS 1996 Meta-analysis of ten randomized trials • Shaft fractures: Gamma 3 • Required Re-ops: Gamma 2 x CHS (p < 0.001) x CHS (p < 0.01) • IM fixation may be superior for inter/subtroch extension & reverse obliquity fractures • “ CHS is a forgiving implant when used by inexperienced surgeons, the Gamma nail is not” MJParker, Parker, International Orthopaedics '96 Gamma nails revisited (risk of shaft fracture….) Bhandari, Schemitsch et al. JOT 2009 No more increased risk with nails Surgeon controlled factor: Implant selection IM Fixation: Clinical Results RCT, IMHS vs CHS, N = 135 No difference for stable fxs Faster & less bloody for unstable fxs Fewer IM complications than Gamma Weaknesses: No stratification of unstable fractures Learning curve issues No anatomic outcomes, wide functional outcomes Baumgaertner, Curtin, Lindskog, CORR ‘98 Surgeon controlled factor: Implant selection IM Fixation: Clinical Results Well analyzed RCT, IMHS vs CHS, N = 100 Longer surgery, less blood loss Improved post-op mobility @ 1 & 3 months * Improved community ambulation @ 6 & 12 months * 45% less sliding, LLD* (* p < 0.05) Hardy, et. al JBJS(A) ‘98 Surgeon controlled factor: Implant selection IM IMFixation: Fixation:Mechanical MechanicalAdvantages Advantages ? ! Key point It is not the reduced lever arm that offers the clinically significant mechanical advantage, but rather the intramedullary buttress that the nail provides to resist excessive fracture collapse* * Reduced collapse has been demonstrated in most every randomized study that has looked at the variable The nail substitutes for the incompetent posteromedial cortex 31.A33 2 weeks 7 months The nail substitutes for the incompetent lateral cortex CHS: Unique risk of failure Palm, et al JBJS(A) ‘07 Iatrogenic, intraoperative lateral wall fracture 31% risk in A2.2&3 fxs 22% failure rate (vs. 3% overall) A2 to A3 fx! Surgeon controlled factor: Implant selection IM Fixation: Selected Clinical Results RCT, IMscrew vs CHS, N = 436 less sliding, shaft medialization* Ahrengart, CORR ‘02 RCT, IMscrew vs CHS, N = 46 5° in neck shaft angle @ 6 wks (all) shaft medialization @ 4mo * Pajarinen, Int Orth ‘04 RCT, IMscrew vs CHS, N = 108 Improved post-op mobility (4 months)* less sliding, shaft medialization* (* p < 0.05) Pajarinen, JBJS(B) ‘05 Surgeon controlled factor: Implant selection CHS Improvements: 1975-2010 Trochanteric Stabilizing Plate (TSP) plate adjunct to limit shaft medialization major (≥20mm screw slide) collapse op time, blood loss ? complications, length of rehab Madsen, JOT '98 Su, Trauma ‘03 Bong, Trauma ‘04 Surgeon controlled factor: Implant selection IM Fixation: Best Indications Reverse Oblique Fractures Intertroch + subtrochanteric fractures Surgeon controlled factor: Implant selection Reverse Oblique Fractures Retrospective review of 49 consecutive R/ob. fractures @ Mayo: overall 30% failure rate Poor Implant Position: 80% failure Implant Type: Compression Hip Screw: 95° blade / DCS: 56% failure (9/16) 20% failure (5/25) IMHipScrew: 0% failure (0/3) Haidukewych, JBJS(A) 2001 Surgeon controlled factor: Implant selection Reverse Oblique Fractures PFN vs 95° sliding screw plate(DCS) RCT of 39 cases done by Swiss AO surgeons PFN (IM) vs Plate Open reductions Op-time All Significantly Blood tx reduced! Failure rate Major reoperations Sadowski,Hoffmeyer JBJS(A) 2002 Recovery room control X-ray shows loss of medial support, but nail prevents excessive collapse Surgeon controlled factor: Implant selection Intertroch/ subtrochanteric fxs Greater mechanical demands, poorer fracture healing Surgeon controlled factor: Implant selection Long Gamma Nail for IT-ST Fxs Barquet, JOT 2000 52 consecutive fractures; 43 with 1 year f/u 100% union 81 minutes, 370cc EBL The authors describe the key percutaneous reduction techniques that lead to successful management of these difficult fractures Reduction Aids Surgeon controlled factor: Implant selection Unstable Pertroch Fractures (OTA31A.3) 347 articles reviewed: 10 relevant; 5 RCTs* “Evidence-based bottom line:” Unacceptable failure rates with CHS Better results with 95° devices Best results with I M devices* Best “functional outcome” not known Kregor, et al (Evidence Based Working Group) JOT ‘05 CHS 31 AO / OTA Surgeon controlled factor: Implant selection Grossly displaced Stable (31A.1) fracture treated with ORIF Surgeon controlled factor: Implant selection There is no data to support nailing over sideplate fixation for A1 fractures CHS ???? 31 AO / OTA NAIL Surgeon controlled factor: Implant selection IM Fixation vs. CHS Randomized/prospective trial of 210 pts. Patients Utrilla, et al. JOT 4/05 All ambulatory, no ASA Vs Fractures Excluded inter/subtrochs fractures (31A.3) --excludes the fxs KNOWN to do best with IM Surgeons Only 4, all experienced Technique All got spinals, Closed reduction, percutaneous fixation All overreamed 2mm, all got 130° x 11mm nail, one distal interlock prn rotational instability (rarely used) Surgeon controlled factor: Implant selection IM Fixation vs. CHS Randomized/prospective trial of 210 pts. Results Utrilla, et al. JOT 4/05 • Skin to skin time unchanged • Fewer blood transfusions needed with IM • Better walking ability in Unstable fractures with IM No shaft fxs Fewer re-ops needed in IM group (1 vs 4) • • Conclusion • IM fixation or CHS for stable fxs • Unlocked IM for most Unstable fxs JBJS(A) 2010 No difference: • Transfusions • Hospital stay Re-ops Mobility Residence However…. Grossly underpowered (beta error) 300-500/arm needed Any patient eligible (age 42-99) Used Long Nails Outcome measures perfunctory No X-rays 32% mortality 21% phone /proxy only •This is gold? Surgeon controlled factor: Implant selection IM Hip Screws Author’s Opinion Data supports use for unstable fractures RCTs document improved anatomy and early function Iatrogenic problems decreased with current designs and technique Indicated only for the geriatric fracture Surgeon controlled factor: Implant selection IM Hip Screw: Contraindications young patients (excess bone removal) basal neck fxs (iatrogenic displacement) stable fractures requiring open reduction (inefficient) stable fractures with very narrow canals (inefficient) Technical Tips Patient Set-up Position for nailing: Hip Adducted Unobstructed AP & lateral imaging Fracture Reduced(?) Strong traction (without well leg countertraction) abducts fractured hip and prevents gaining proper entrance site Strong traction (without well leg countertraction) abducts fractured hip and prevents gaining proper entrance site The solution is the “Scissors position” for the extremities •Both feet in txn •Fx: flexed & add •Well leg extended & abducted • Lateral Xray: a little different, but adequate Guide Pin Insertion Guide Pin Insertion (Usually by hand…) Ostrum, JOT 05: The entrance is at the trochanteric tip or slightly MEDIAL Ream a channel for implant! (don’t just displace the fracture as you pass reamer through it) Medial directed force prevents fracture gapping during entrance reaming Achieve a Neck-Shaft Axis > 130° Use at least a 130° nail Varus Corrections Advance nail Increase traction ABDUCT extremity!! (adduction only necessary of nail insertion) at time Postoperative Management Allow all patients to WBAT Patients “self regulate” force on hip No increased rate of failure Koval, et. al,JBJS(A)’98 X-rays post-op, then 6 & 12 weeks Epilogue: intertrochs (Questions without good answers) Unanswered questions Where’s the evidence?? Minimally invasive PLATE fixation ?? 2 hole DHS Bolhofner Dipaola PCCP Gotfried Which nail design is best ?? Proximal diameter? Nail Length? Distal interlocking? Proximal screw ? Sleeve or no sleeve? Loch & Kyle, JBJS(A)‘98 One or two needed ? Nobody knows! Proximal fixation: 1 or 2 screws? Kubiak, JOT ‘04 IMHS vs Trigen in vitro (cadaveric) testing Results: No difference in fx sliding or collapse No difference in rigidity or stability Trigen with higher ultimate strength @ failure Clinical significance?? Nobody knows! Small Screws protect lateral wall Gotfried, CORR ‘04 Im, JOT ‘05 Only relevant for plate fixation? Small Screws protect lateral wall from fx Gotfried, CORR ‘04 Im, JOT ‘05 Only relevant for plate fixation? But… the “Z effect” 7/70, 10% Werner-Tutschku, Unfall ’02 5/45 11% Tyllianakis Acta Orthop Belgica ‘04 Long vs.short nails? Thigh pain from short, locked nails? Periprosthetic fracture: Still an issue? Anterior cortex perforation with long nails? 6% impinge/ 2% fx Robinson, JBJS(A) 05 Cost/ benefit? -Nobody knows- Just when you think you know whats best-- Don’t forget Ex-Fix! ? RCT n=40 Exfix +HA vs DHS Faster ops, fewer txfusions, no comps Moroni, et al. JBJS(A) 4/05 Ex-fix (HApins) vs DHS Randomized/prospective trial of 40 pts. Patients Moroni, et al. JBJS(A) 4/05 65yo+ walking women with osteoporosis Results Faster operations with Fewer transfusions Less post op pain, similar final function No pin site infxs, no increased post op care Increased pin torque on removal @ 12 wks One nonunion Conclusions: Remember Kaufer’s Variables Uncontrolled factors Fracture Geometry Bone Quality Surgeon controlled factors Quality of Reduction Implant Placement Implant Selection Conclusions: Implants have different traits-choose wisely Position screw centrally and very deep (TAD≤20mm) Conclusions: Things change Healing is no longer “success” Deformity & function matter Perioperative insult counts Audience Response Questions! (save 5-8 minutes for these) 81 y.o. female slipped & fell 3 part IT fx Discuss: Did the surgeon do a good job? Yes or No Post-op X-rays Did the surgeon do a good job? Yes No Answer before advancing. Now, consider specifically: A.The reduction is satisfactory B. The TAD (screw position) is OK C. Both are satisfactory D. Neither are satisfactory …Choose Best Answer 6 months 3months Post op The TAD was acceptable but the reduction was grossly short Did the surgeon do a good job? Yes No 27yo jogger struck by car, closed, isolated injury 27yo jogger struck by car I’d reduce & fix with: A. 95° blade B. DCS plate C. “Recon” Nail D. DHS E. Intramedullary hip screw (PFN, TFN, IMHS, GAMMA) A.The reduction is satisfactory B. The TAD is satisfactory C. Both are satisfactory D. Neither are satisfactory * * Progressive pain 11-14 weeks (varus + plate is rarely good) I’d Bonegraft & revise with: A. 95° blade B. DCS plate C. “Recon” Nail D. DHS E. IMHS F Other 95° DCS + autoBG 71 yo renal txplnt pt c CHF What to do?? If my patient, I would use: 1. Hip screw and sideplate 2. Hip screw and IM nail (TFN) 3. Reconstruction Nail (2 proximal medullary-cephalic screws) 4. Blade Plate 5. Other percutaneous reduction Uneventful Healing, WBAT 6wks 12wks If you would like to volunteer as an author for the Resident Slide Project or recommend updates to any of the following slides, please send an e-mail to ota@aaos.org E-mail OTA about Questions/Comments Return to Lower Extremity Index