Treatment of Pterygium
advertisement
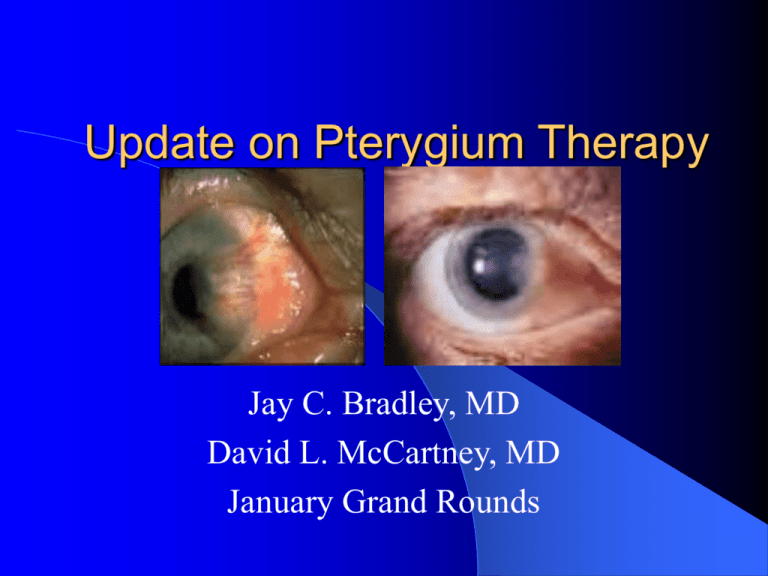
Update on Pterygium Therapy Jay C. Bradley, MD David L. McCartney, MD January Grand Rounds From the BCSC: Basics Often bilateral Almost always situated at the nasal or temporal limbus within palpebral fissure Associated with prolonged UV exposure UV-B limbal stem cell p53 mutation apoptosis / TGF- growth May be associated with dryness, inflammation, and exposure to wind and dust or other irritants Prevalence increases with proximity to equator Difficult to determine if race is independent risk factor due to confounding variables Albedo Hypothesis Researcher: MT Coroneo (Australia) Pterygia occur secondary to albedo concentration in the anterior eye Light entering the temporal limbus at 90 degrees is concentrated onto the medial limbus Related to corneal curvature Explains predominance of medial pterygia Ophthalmic surg. 1990 Jan;21(1):60-6. From BCSC: Basics Encroaches on cornea in wing-like fashion Overlying epithelium often thinned, but can be hyperplastic or dysplastic Nearly always preceded by pingueculae Induces astigmatism (usually “with-the-rule”) proportional to size Excision indicated if persistent irritation, vision distortion, significant (> 3-4 mm) and progressive growth toward visual axis, restricted ocular motility, and atypical appearance From the BCSC: Basics Elastotic degeneration – fragmentation and breakdown of stromal collagen Destruction of Bowman’s layer by advancing fibrovascular tissue resulting in corneal scarring From BCSC: Basics Recurrent pterygia – lack elastotic degeneration and are more accurately classified as an exuberant granulation tissue response Stocker’s line – a pigmented iron line in advance of pterygium Pterygium Excision Goal: Achieve a normal, topographically smooth ocular surface Dissect a smooth plane toward the limbus Some surgeons prefer specialized blunt pterygium blades (Tooke or Gills) while others prefer sharp blades Preferable to dissect down to bare sclera at limbus Bare sclera = remove loose Tenon’s layer and leave episcleral vessels intact Some surgeons avoid medial dissection to avoid bleeding from trauma to adjacent muscle tissue while other remove excessive fibrovascular tissue medially Light thermal cautery is applied for hemostasis Pterygium Recurrence Growth of fibrovascular tissue across the limbus onto cornea after initial removal Excludes persistence of deeper corneal vessels and scarring which may remain even after adequate removal Bunching of conjunctiva and formation of parallel loops of vessels, which aim almost like an arrowhead at the limbus, usually denotes a conjunctival recurrence Proposed Recurrence Grading System Grade 1 – normal appearing operative site Grade 2 – fine episcleral vessels in the site extending to the limbus Grade 3 – additional fibrous tissues in site Grade 4 – actual corneal recurrence Wound Closure Options: Bare sclera Simple closure Sliding flap Rotational flap Conjunctival graft Bare Sclera Closure No sutures or fine, absorbable sutures used to appose conjunctiva to superficial sclera in front of rectus tendon insertion Leaves area of “bare sclera” Relatively high recurrence rate with variable techniques of 5 – 68 % with primary / 35 – 82 % with recurrent) Simple Closure Free edges of conjunctiva secured together Effective only if defect is very small Can be used for pingueculae removal Reported recurrence rates from 45 – 69 % (one report of “barest” sclera, N=800 of 2 %) Few complications (dellen) Sliding Flap Closure An L-shaped incision is made adjacent to the wound to allow conjunctival flap to slide into place Reported recurrence rates from 0.75 – 5.6 % (poorly designed, retrospective) Few complications (flap retraction / cyst formation) Rotational Flap Closure A U-shaped incision is made adjacent to the wound to form tongue of conjunctiva that is rotated into place Reported recurrence of 4 % Few complications Conjunctival Graft Closure A free graft, usually from superior bulbar conjunctiva, is excised to correspond to wound and is then moved and sutured into place Can be performed with inferior conjunctiva to preserve superior conjunctiva Conjunctival Graft Closure Harvested tissue should be approximately 0.5 – 1 mm larger than defect Most important aspect in harvesting is to procure conjunctival tissue with only minimal or no Tenon’s included Graft is transferred to recipient bed and secured with or without incorporating episclera Some surgeons harvest limbal stem cells along with graft and orient graft to place stem cells adjacent to site of corneal lesion excision Conjunctival Graft Closure Topical antibiotic-corticosteroid ointment used for 4 – 6 weeks post-operatively until inflammation subsides (compliance with this regimen decreases recurrence) Used when extensive damage or destruction of limbal epithelial stem cells is NOT present Reduces recurrence to 2 – 5 % (up to 40 % in some reports) Ameliorates the restriction of extraocular muscle function Limbal Conjunctival Autograft Reported recurrence rates are variable (between 0 – 40 %) Few complications Further prospective studies in primary and recurrent pterygia are needed Lamellar Corneal Transplant Wound closed with piece of lamellar sclera or cornea Reported recurrence rates of 6 – 30 % Not performed often Can be used in conjunction with AMT for multiply recurrent pterygia with corneal scarring and limited available conjunctiva Method involves increased surgical complexity, the requirement of donor tissue, and risk of infectious disease transmission Adjunctive Beta Irradiation Most common dosage is 15 Gy in single or divided doses Reasonably acceptable recurrence rates (from 0 – 50 % with bare sclera or simple conj closure) Risk of corneal or scleral necrosis and endophthalmitis Adjunctive Thiotepa Most common dose is 1:2000 thiotepa given up to every 3 hours for approx. 6 weeks Usually used with bare sclera method Low reported recurrence rates of 0 – 16 % (poor study quality) Minimal complications (2 cases of scleral thinning) Adjunctive Mitomycin C Used with bare sclera or conj closure Most common dose is 0.02 % applied for 3 min during surgery Risk of aseptic scleral necrosis / perforation and infectious sclerokeratitis Used more often for recurrent cases Rate of recurrence between 3 – 25 % for intra-op / 5 – 54 % for post-op with most studies showing < 10 % recurrence Amniotic Membrane Graft Closure Useful for very large conjunctival defects as in primary doubleheaded pterygium or to preserve superior conjunctiva for future glaucoma surgeries Requires costly donor tissue Reported recurrence rate between 3 – 64 % for primary cases and 0 – 37.5 % for recurrent cases Other Methods: Pterygium head transplantation Split skin grafts Ruthenium adjunctive therapy Laser or thermal cautery Excimer laser treatment PDT (one report, N = 10) Intraoperative doxorubicin / daunorubicin 5-FU Serum-free derived cultivated conjunctival graft Recombinant epidermal growth factor ****Few studies with limited numbers of patients, poor follow-up, and variable recurrence rates Primary Pterygium Metanalysis Includes 5 studies with N=290 (BS+Mito=257/CAG=33) Comparison Bare sclera: mito C Bare sclera: CAG Odds Ratio 95 % CI 25:1 6:1 9.0 – 66.7 1.8 – 18.8 Sanchez-Thorin JC et al. Br J Ophthalmol 82:661-5, 1998. Conclusions: There is no clear-cut superior single treatment Bare scleral and simple conjunctival closure without adjunctive therapy have relatively high but variable recurrence rates Use of beta irradiation and antimetabolites can be used with appropriate caution Conjunctival transplants and flaps appear to have overall lower rate of recurrence but require more surgical time and unnecessary conj destruction Other treatment options need further adequate study prior to widespread implementation Any Questions?