9 contraceptiveIII
advertisement

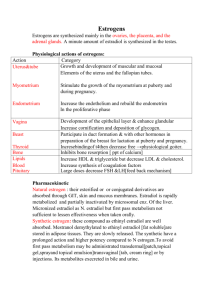
Contraceptive 326 Dr.Hazar Objectives List the drugs and mechanisms used to attenuate the actions of sex hormones. Ex. Gonadotrophines releasing hormones ;agonists &antagonists. Understand the Types ,MOA,S.E ,uses & C.I. of the hormonal contraceptive drugs. Understand the Types ,MOA,S.E ,uses & C.I. of the fertility drugs. Gonadotrophines releasing hormones agonists &antagonists. 1.danazol &danazol analogues 2.gonadorelines analogues 3.fertility drugs 1.danazol &danazol analogues Danazol 1.Gonadotropin inhibitor with antiestrogen ,progestational and androgenic properties 2.synthetic version of the male hormone testosterone 3.inhibits the release of FSH and LH by the pituitary gland 4.decreases estrogen levels similar to menopause, stops ovulation 5.shrink abnormal implants Danazol Indications: 1.Endometriosis 2. Mammary dysplasia (fibrocystic breast nodularity) 3. Menorrhagia ;(but not contraception). 4.Gynaecomastia. Danazol Side effects androgenic effects (deepening of the voice, abnormal hair growth, reduced breast size, water retention, acne, weight gain ;nearly all gain weight between 8-10 lbs.) hypoestrogenic reactions (flushing, sweating, vaginal dryness, irritation) amenorrhea irregular vaginal bleeding, muscle cramps Danazol analogues 1-Gestrinone is danazol agonist Ditto action –danazol Used only in Endometriosis 2-Cetrorelix-LHRH antagonist ↓FSH &LH used in infertility. 3-Ganirelix-ditto 2.Gonadorelines analogues Continuos use 1. ↓ Gonadotropines Receptors and sensitivity in the Pituitary ; Down regulation 2. ↓ LH,FSH ;estrogen level ↓ 3. No ovulation 4. ↓ endometrium Treatment Endometriosis Polycystic ovarian Disease Prostate Cancer Precocious Puberty Breast Cancer 2.Gonadorelines analogues Pulsatile use 1. Activation of natural Gonadotropines pituitary Receptors to stimulate release of FSH and LH Indication Induction of ovulation invitro fertilization Types of Gonadorelines analogues GnRH Analogues Nafarelin -nasal spray approved in 1990 -200x>potent than natural LHRH -relieves symptoms and shrinks implant or stops -them from growing -puts body into menopausal like state -side effects: hot flashes; vaginal dryness; lighter, less frequentor no menstruation; headaches; nasal irritation -should not be used in women who are pregnant, breast feeding, or have undiagnosed vaginal bleeding Goserelin · · · Made specifically for treatment of endometriosis in 1990 by decreasing the amount of estrogen in the body, the body is induced into a menopausal state may be administered by a subcutaneous implant which is placed in the abdominal wall Types of GnRH analogues+uses Types Endometriosis Prostate cancer IVF Buserelin + + Nafarelin + + Leuprolin + + Triptorolin + + Goserelin + + + Breast cancer + Contraceptives Objectives 1. Understand the mechanisms by which oral contraceptives prevent ovulation. 2. Know the potential adverse effects & containdication of oral contraceptive therapy . 3. Become familiar with the other type of contrceptives ( non oral ) REF 1. Katzung's. 2. Rang & Dale 3. Goodman and Gilman Types of Oral Contraceptives Types of preparations 1. Combinations - contain an estrogen and a progestin given continuously for three weeks (most widely used). a. High dose estrogen ≥ 0.05 mg (first generation) b. Low dose estrogen < 0.05 mg, usually 0.02 - 0.035 (second generation) c. Low dose estrogen with a lesser androgenic progestin (third generation) 2.Sequential Products a. monophasic b. biphasic c. triphasic Monophasic OC 3. Minipills-progestin only (block ovulation, slowing GnRH pulse generation decreased LH surge) For female with: Venous thromboembolism , smoker, DM, HT, migrain & lactation. 4. Morning-After Pill (administer within 72 hrs of coitus, continue 2x for 5 days) Emergency contraceptives drugs used for the prevention of pregnancy following unprotected intercourse or a known or suspected contraceptive failure to be effective these must be taken within 72 hours of intercourse two products are available: Plan B: 0.75 mg levonorgestrel Preven: 0.25 mg levonorgestrel and 0.05 mg ethinyl estradiol (this product includes a pregnancy test kit) Mechanism of Action Combination Inhibition of ovulation via continuous negative feedback on hypothalamic-hypophyseal axis (LH/FSH suppressed, no LH surge) Progesterone decreases the frequency of GnRH pulses Changes in the Endometrium Thickens cervical mucus- difficult sperm penetration Changes in the Fallopian Tube Prevent follicular maturation M.O.A Progestins alone 1.There is variable suppression of FSH, LH and ovulation. Menstruation may occur with irregular cycles. 2. Altered endometrial structure may prevent implantation and heavy cervical mucus may prevent sperm penetration. 3. Continuous use lends itself to long-acting preparations intramuscular, subcutaneous, or intrauterine depots (medroxyprogesterone acetate, levonorgestrel). Names Combinations Estrogens: Ethinyl estradiol ,Mestranol Progestins : levonorgestrel , Norethindrone Progestins-only Levonorgestrel , norethindrone, ethynodiol diacetate Morning-After Diethylstilbestrol Norethindrone Ethinyl estradiol + levonorgestrel Postcoital IUD contain Cu (best) Other oral preparations: Ethinyl estradiol + norethindrone Ethinyl estradiol + ethynodiol diacetate Ethinyl estradiol + norethynodrel Ethinyl estradiol + levonorgestrel Adverse effects Estrogen-related 1.Cardiovcascular Disease a. Deep vein thrombosis b. Thromboembolism Thromboembolic disorders due to effects on clotting factors and platelet aggregation properties; myocardial infarction; stroke • • • • • • • • • • • • Nausea, vomiting Edema (weight gain, breast engorgement) due to salt and water retention Headaches, dizziness Hypertension resulting from salt and water retention and increased hepatic secretion of angiotensinogen Breakthrough bleeding Urinary tract infection Folic acid deficiency Increased serum triglycerides Dysmennorrhea Ocular changes Chloasma Gall bladder disease related to increased cholesterol precipitation due to a decrease in bile flow • Decreased glucose tolerance via lowered sensitivity to insulin; possibly related to estrogen-stimulated release of insulin-antagonistic hormones (e.g., GH, T3+4, cortisol). • Carcinogenesis a. breast b. endometrial c. ovarian d. cervical e. hepatic Progestin-related Depression - possibly related to increased MAO activity Headaches Loss of hair and/or hirsutism, acneassociated with 19-norsteroids Yeast infections Contraindications to Oral Contraceptive Use Current or past history of deep vein thrombosis, stroke, coronary artery disease, or hypertension Cancer of the breast Strong family history of the above Active liver disease Heavy cigarette smoking Stroke - smokers over 35 Types of non oral contrceptives 1.Barrier-condom 2.Devices-IUD – (levonorgestrel,Cu),Cap. 3.Spermicidal-Nonoxinol (creams and gels). 4.Injections Monthly injectable – medroxyprogesterone1/12 Norethisterone 8/52 5.Vaginal ring - ethinyl estradiol + etonorgestrel 6.Patch - ethinyl estradiol + norelgestromin 7. Levonorgestrel implants . Levonorgestrel Intrauterine Device Releases 20 µg levonorgestrel each day Indicated for contraception 80%–90% reduction in menstrual blood loss (not associated with copper-T IUD) Also effective in treating menorrhagia, endometriosis Use up to 5 years Side effects: breakthrough bleeding, ovarian cysts, acne Cost effective Levonorgestrel-releasing intra uterine system Progesterone releasing IUD Superior to oral progesterones reduces MBL by 96% 64% women cancelled hysterectomy compared to 14% on medical treatment, effective contraceptive Suppresses development of endometrium but does not suppress ovulation Effective for 5 years 90% women menorrhagia cured in 3 months Infertility Ovulatory Dysfunction Causes of ovulatory dysfunction: polycystic ovary syndrome hypothalamic anovulation hyperprolactinemia premature and age-related ovarian failure luteal phase defect Polycystic Ovarian Syndrome Oligomenorrhea/amenorrhea and hyperandrogenism Prevalence: 5%. Among women with O.D., 70% have PCOS. Clinical evidence: hirsutism, acne, obesity Lab evidence: elevated testosterone, elevated DHEA-S. PCOS: Treatment Approach Weight loss if BMI>30 Clomiphene to induce ovulation If DHEA-S >2, clomiphene + glucocorticoid (dexamethasone) If clomiphene alone unsuccessful, try metformin + clomiphene. Endometriosis Medical Treatments Oral Contraceptives Progestins Danazol D.O.C NSAIDs GnRH analogues