The management of postoperative pain
advertisement

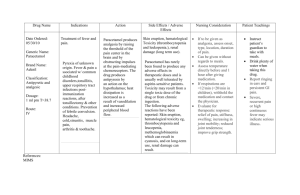
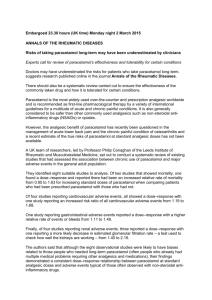
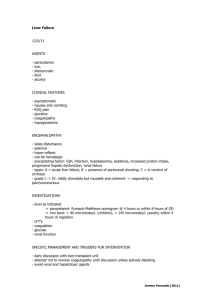
A New Molecule for Post Operative Pain Management Dr.P.Selvakumar M.D., Senior consultant Apollo Specialty Hospitals Madurai Clinical definition of pain1 “An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage... 1. IASP Pain Terminology. In Merskey H & Bogduk N eds. Classification of Chronic Pain, Second Edition, IASP Task Force on Taxonomy. IASP Press, Seattle 1994:209-14. Objectives Types of pain Pain physiology Multimodal analgesia Intravenous agents used for postoperative pain Conclusions Pain: Clinical Types Nociceptive pain Inflammatory pain Transient pain in response to noxious stimuli Spontaneous pain and hypersensitivity to pain in response to tissue damage and inflammation Neuropathic pain Spontaneous pain and hypersensitivity to pain in association with damage to or a lesion of the nervous system Woolf. Ann Intern Med. 2004;140:441-451. Nociceptive Pain Is responsive to NSAID’s, coxibs, paracetamol and opiates Noxious Peripheral Stimuli Pain-Autonomic Response Heat - Withdrawal Reflex Cold Intense Mechanical Force Nociceptor Sensory Neuron Brain Chemical Irritants Spinal Cord Woolf. Ann Intern Med. 2004;140:441-451. Inflammatory Pain Is responsive to NSAID’s,coxibs, paracetamol, and opiates Pain Inflammation Spontaneous Macrophage Mast Cell Neutrophil Granulocyte Pain Hypersensitivity -Allodynia -Hyperalgesia Nociceptor Sensory Neuron Brain Tissue Damage Spinal Cord Woolf. Ann Intern Med. 2004;140:441-451. Neuropathic Pain Spontaneous Pain Pain Hypersensitivity •May respond to • local anaesthetic • anticonvulsants • antidepressants Peripheral Nerve Damage •Less responsive to opioids Brain Stroke Spinal Cord Injury •No response to NSAID’s, coxibs, or paracetamol . Woolf. Ann Intern Med. 2004;140:441-451 Postoperative pain is nociceptive Perception Modulation Is responsive to NSAID’s,coxibs, paracetamol and opiates Transmission Transduction Reuben et al. J Bone Joint Surg. 2000;82:1754-1766. Consequences of Unrelieved Pain Acute Pain Increased sympathetic activity GI effects Splinting, shallow breathing Increased catabolic demands Anxiety and fear Peripheral/ central sensitization Myocardial O2 consumption GI motility Atelectasis, hypoxemia, hypercarbia Poor wound healing/muscle breakdown Sleeplessness, helplessness Available drugs Myocardial ischemia Delayed recovery Pneumonia Weakness and impaired rehabilitation Psychological Chronic pain Courtesy of Sunil J Panchal, MD Intensity of Pain After Discharge: 81% Report Moderate to Extreme Pain 8% 19% 21% 52% Pain Intensity Slight Moderate Apfelbaum et al. Anesth Analg. 2003;97:534-540. Severe Extreme Guidelines for optimising POP management1,2,3,4,5,6 Adequate and thorough patient information2,3,4,5,6 Use of written protocols1,3,4,5,6 Regular assessment of pain intensity1,2,3,4,5,6 Adequate medical and nursing staff training1,3,4,5,6 Use of balanced analgesia, PCA, and epidural drug administration1,2,3,4,5,6 1. The Royal College of Surgeons of England and the College of Anaesthetists. Commission on the provision of surgical services, report of the working party on pain after surgery. London, UK, HMSO.1990. 2. Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Services. Acute Pain Management in Adults: Operative Procedures. Quick Reference Guide for Clinicians. AHCPR Pub. No. 92-0019. Rockville, MD.1992. 3. International Association for the Study of Pain, Management of acute pain: a practical guide. In: Ready LB, Edwards WT, eds. Seattle, 1992. 4. Wulf H et al. Die Behandlung akuter perioperativer und posttraumatischer Schmerzen Empfehlungen einer interdisziplinaeren Expertenkommision. G. Thieme, Stuttgart, New York. 1997. 5. EuroPain. European Minimum Standards for the Management of Postoperative Pain.1998. 6. SFAR. Conférence de consensus. Prise en charge de la douleur postopératoire chez l’adulte et l’enfant. Ann Fr Anesth Réanim 1998;17:445-61. Effective pain management may improve outcomes1,2,3 Effective analgesia included in a comprehensive postoperative rehabilitation programme1,2 Improved patient comfort and satisfaction Decreased postoperative morbidity Faster recovery Shorter hospital stay1,2,3 Very favourable cost/benefit ratio2 Low cost of analgesic techniques and drugs2 1. Kehlet H. Br J Anaesth 1994;72(4):375-8. 2. Jayr C. In Les Aspects Economiques de l’Anesthésie. JEPU 2000:131-8. 3. D’Amours RH et al. JOSPT 1996;24(4):227-36. Physiology & pharmacological management of postoperative pain Pain pathway and modulation1 Ascending nociceptive pathways Interpretation in cerebral cortex: pain Stimulation of nociceptors (A and C fibers) / Release of neurotransmitters and neuromodulators (i.e. PG) Descending inhibitory controls / Diffuse noxious inhibitory controls Activation of serotoninergic and noradrenergic pathways Release of serotonin, noradrenalin and enkephalins at spinal level Injury 1. Adapted from: Bonica JJ. Postoperative pain. In Bonica JJ, ed. The management of pain. Philadelphia: Lea and Febiger;1990:461-80. Modes of action of analgesics1,2,3,4 Paracetamol Inhibition of central Cox-3 (?) (Inhibition of PG synthesis) Opioids Activation of opioid receptors Paracetamol Interaction with serotoninergic descending inhibitory pathway NSAIDs / Coxibs Inhibition of peripheral and central Cox-1 / Cox-2 (Inhibition of PG synthesis) 1. D’Amours RH et al. JOSPT 1996;24(4):227-36. 2. Piguet V et al. Eur J Clin Pharmacol 1998;53:321-4. 3. Pini LA et al. JPET 1997;280(2):934-40. 4. Chandrasekharan NV et al. PNAS 2002;99(21):13926-31. Multimodal and Preemptive Approaches to Managing Postoperative Pain The concept and benefits of balanced analgesia “The rationale for multimodal analgesia is achievement of sufficient analgesia due to additive or synergistic effects between different analgesics, with concomitant reduction of side effects, due to resulting lower doses of analgesics and differences in side -effect profiles” 1. Kehlet H et al. Anesth Analg 1993;77:1048-56. Patients’ Preferences for Acute Pain Treatment Patients prefer avoiding side effects over complete pain control Side-Effect Severity 19% Pain Control 41% 47% Setting and Route of Administration 12% Gan et al. Br J Anaesth. 2004;92:681-688. Side-Effect Type 28% Proportion of Patients Experiencing Adverse Events Adverse Event (AE) Total % Constipation 50 Mental cloudiness/dizziness 82 Itching 54 Nightmares/hallucinations 32 Mood changes/alterations 34 Nausea 70 Sleep disorders 48 Vomiting 32 Gan et al. Br J Anaesth. 2004;92:1-8. Preventive Multimodal Analgesia Significant improvement in Pain reduction Opioid use Opioid-related AEs Recovery or day ward length of stay Unplanned admission to the hospital Reuben et al. Acute Pain. 2004;6:87-93. “Real World”: Multimodal Analgesia Opioids Potentiation NSAIDs, coxibs, paracetamol, nerve blocks Kehlet et al. Anesth Analg. 1993;77:1048-1056 (B). Reduced doses Improved pain relief Reduce severity of AEs Earlier discharge Decreased costs Intravenous agents for multimodal analgesia IV morphine Intermittent IV bolus doses Is best method for acute pain Optimal doses and dose intervals not established 2-3 mg doses at 5 minute intervals appears effective Continuous infusion Compared with PCA there is a 5-fold increase in respiratory depression IV paracetamol - premise “Is more effective & has a faster onset than oral paracetamol” Means of pain intensity differences (VAS) Onset of action is fast and effective – within 5 minutes Sindet-Pedersen S. Br Jr Anesth 2005. 94 (5): 642-8 Paracetamol: clinical pharmacology Paracetamol: a well known analgesic agent First proper account of clinical use in 1894 Analgesic effect formally demonstrated in 1948 (Flinn and Brodie) Recommended first-line analgesic therapy: (Hinsberg and Treupel)1 - for the treatment of osteoarthritis since 2000 - for musculoskeletal pain in elderly since 2002 - for patients with renal disease since 1996 4 5 1. Prescott LF. Am J Therapeut 2000;7(2):143-7. 2. EULAR recommendations. Pendleton A et al. Ann Rheum Dis 2000;59(12):936-44. 3. American College of Rheumatology Subcommittee on osteoarthritis guidelines. Arthritis Rheum 2000;43(9):1905-15. 4. AGS Panel on Persistent Pain in Older Persons. JAGS 2002;50:S205-24. 5. Henrich WL et al. Am J Kidney Dis 1996;27(1):162-5. 2,3 1 Paracetamol – how does it work? Paracetamol is a centrally acting agent It selectively inhibits nervous system PG synthesis probably via COX-3 2,3 Other central mechanisms of action depend on the bulbo-spinal serotoninergic pathway 4,5 1. Piguet V et al. Eur J Clin Pharmacol 1998;53:321-4. 2. Carlsson KH et al. Pain 1988;32:313-26. 3. Flower RJ et al. Nature 1972;240:410-1. 4. Tjølsen A et al. Eur J Pharmacol 1991;193:193-201. 5. Pélissier T et al. JPET 1996;278:8-14. Objective R-III reflex threshold changes expressed as a percentage of difference from baseline Paracetamol clinically demonstrates central activity1 1. Piletta P et al. Clin Pharmacol Ther 1991;49(4):350-4. What were the challenges? 1. Making paracetamol soluble Use of hydrophilic ingredients (mannitol and disodium phosphate) 2. Ensuring its stability in solution - By controlling hydrolysis Use of a pH buffer (disodium phosphate and sodium hydroxide) - By preventing oxidation Addition of cysteine hydrochloride Oxygen-free manufacturing process Indications Phase III clinical trials1,2 VS. placebo Similar overall incidence of adverse events Similar incidence of local adverse events No clinically significant changes in vital signs or laboratory tests IV paracetamol as safe as placebo 1. Lange-Møller P. Anesth Analg 2005;101:90 –6 2. Sinatra RS. Anesthesiology 2005; 102:822–3 India Prescribing Information No difference in adverse events vs placebo Oral surgery Lange-Møller P. Anesth Analg 2005;101:90 –6. No difference in adverse events vs placebo Orthopaedic surgery % Sinatra RS. Anesthesiology 2005; 102:822–3 Hepatic safety at therapeutic doses1 Paracetamol hepatotoxicity was found to be very rare (<1 / 2,500)1 It was always related to misuse and overdose (>4g / day)1 Good hepatic safety 1. Whitcomb DC et al. JAMA 1994;272(23):1845-50. Renal safety Up to 4g / day, paracetamol has an excellent renal safety profile1 No evidence exists for the development of chronic nephropathy with paracetamol2 Recommended by the National Kidney Foundation as the non-narcotic analgesic of choice in patients with underlying renal disease 3 Good renal tolerance 1. Whelton A. Am J Therapeut 2000;7(2):63-74. 2. Blantz RC. Am J Kidney Dis 1996;28(1):S3-6. 3. Henrich WL et al. Am J Kidney Dis 1996;27(1):162-5. Paracetamol safety benefits in POP No centrally mediated side-effects1 (e.g. sedation, constipation, nausea, vomiting, respiratory depression) No effect on platelet aggregation, bleeding, or uric acid excretion2 3 No gastrointestinal side effects Good renal4 and hepatic5 safety Few contra-indications and drug interactions 1. Lechat P et al. Thérapie 1989;44:337-54. 2. Insel PA. Analgesic-antipyretic and antiinflammatory agents and drugs employed in the treatment of gout. In: Goodman & Gilman eds. The pharmacological basis of therapeutics. McGraw Hill, 9th edition, 1996:617-57. 3. Singh G. Am J Therapeut 2000;7(2):115-21. 4. Whelton A. Am J Therapeut 2000;7(2):63-74. 5. Whitcomb DC et al. JAMA 1994;272(23):1845-50. How to use Perfalgan Perfalgan is ready-to-use • No reconstitution Saves nurses time1 Reduces use of ancillary products1 Reduces risk of dosage error1 Reduces risk of contamination1 1. Schmitt E et al. Pharm Hosp 2001;36(147):9-18. 1. Take the cap off 2. Link the bottle to a drip with an air intake 3. Hook the bottle with the built-in calliper Perfalgan infusion Where ? How? • First administration in the OR 15-minute infusion every 4 to 6 hours Dosing schedule: - Adolescents and adults weighing more than 50kg: 1 g / 4 times a day Storage Shelf life is 2 years Do not store above 30°C Do not refrigerate or freeze Conclusions Perfalgan is a fast-acting analgesic, as effective as morphine 10mg1 Perfalgan is a proven opioid-sparing agent2 Perfalgan is well tolerated in all types of patients Perfalgan is ready-to-use and cost-effective3 1. Van Aken H. 1991. Anesth Analg 2004; 98: 159-65 2. Peduto VA et al. Acta Anaesthesiol Scand 1998;42:293-8. 3. Schmitt E et al. Pharm Hosp 2001;36(147):9-18.