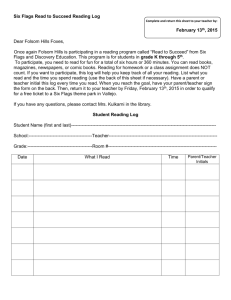
Mechanical Low Back Pain (PEN)
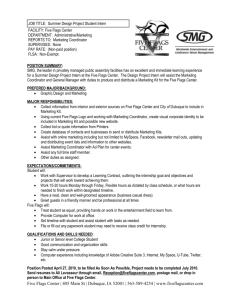
advertisement

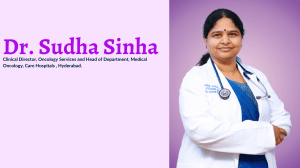
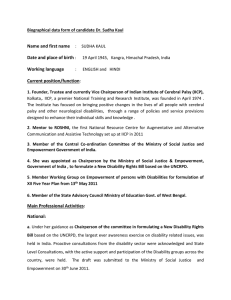
Mechanical Low Back Pain (PEN) Case 2: Sudha www.pspbc.ca Faculty/Presenter Disclosure with Faculty’s Name: Faculty’s Name: Faculty’s Name: 2 Disclosure of Commercial Support . . Mitigating potential bias N/A N/A N/A 3 Objectives When working with CPP, you will be able to: Identify the yellow flags in the patient history to indicate increased risk of developing chronicity List 3 assessment tools that may be useful Provide appropriate referral for rehabilitation therapy 4 Mechanical Low Back Pain “Sudha”, 51 year old female, Legal Assistant, presenting with 6 month history of persistent low back pain She has complained of 3 recurrent episodes of low back pain lasting 2-3 weeks over the last 5 years but the most recent episode started 6 months ago and has persisted without relief She has tried OTC medications, heat and ice and she has tried to remain active with daily walks She is feeling very discouraged and would like to know what else can be done to alleviated her pain. 5 What are your Key Questions? How do you determine if this is mechanical back pain ? 6 What are your Key Questions? How do you determine if this is mechanical back pain ? How do you identify Yellow Flags ? 7 On History, we found… Pain is constant and located in the bilateral back and buttock area. She rates her pain as 9/10 and it radiates to the bilateral lateral thigh area intermittently Her pain is worse with bending and is present with extension. Morning stiffness is 30 minutes There are no changes in his bowel and bladder habits 8 How would Sudha rate her functional abilities? 9 Physical Exam What physical examination techniques would you use? We found: Flexion aggravated low back pain Extension caused pain also but not as much as flexion Strength testing was inconsistent with giving way Normal Neurological exam SLR reproduces low back pain Palpation tenderness of Para spinal muscles Hip Range of motion tight bilaterally with a stretch sensation 10 Psychosocial History What would you want to know? We found: Lives with husband and 23 year old daughter in Lower Mainland College education as Legal Assistant, worked for last 10 years Previously liked doing craft work and hiking Has not done any hobbies in last 6 months due to pain Mood is “anxious and stressed” Concerned that she will not be able to keep working due to pain Has had 40 sick days in the last 6 months. Saddened that husband has to do all domestic chores for family Denies alcohol No prior mental health diagnoses 11 How would you interpret her yellow flag risk ? 12 How can you screen for depression? 13 PHQ9 – Patient Health Questionairre 14 Pain Medication History Sudha initially found that she was in so much pain that she needed Acetominophen with Codeine 4-5 times a day, totally 6-8 tablets. Her pain has continued to escalate and she now takes a muscle relaxant for spasm 3 x day. She has had trouble sleeping in the last month, so is taking some of her husband’s sleeping pills most nights of the week. 15 How would you manage her medication ? 16 Goal: Decrease Pain, Increase Function 17 Management Tools How would you approach Self Management with this patient ? We used: a) What is it about your current health that worries you? b) How do you feel about this ? c) What can you do about this issue? 18 Facilitating your patient to set Goals 19 How do you assess Confidence Levels ? 20 Providing information accurately when asked 21 Clinical Impression Pattern 1 – PEN Back dominant and prone extension negative Positive Yellow flags identifying risk of chronicity She is anxious and showing signs of sadness Her pain management includes self prescribed medications at inappropriate dosing She requires some education on best recovery She needs the opportunity to engage in self management 22 Key Clinical Information What are the key criteria of yellow flag identification? Fear of Activity Sadness and anxiety Dependency on others How do you engage in Self Management ? Patient identifies issues and feelings Facilitation of goal setting Self rating of confidence 23 Summary When working with Mechanical Back Pain, it is important to: 1.Take a targeted history 2.Do a movement examination even if pain is reproduced. 3.Identify assessment tools that may be helpful 4.Promote patient education on activation and recovery. 5.Facilitate Patient Self Management 24 References January 2013, Current Clinical Care, Low Back Pain White paper on Self Management New Zealand Yellow Flags Guideline 25