Trauma management
advertisement

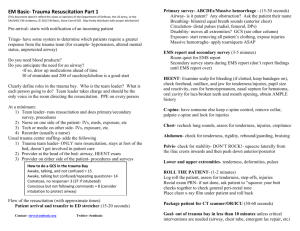
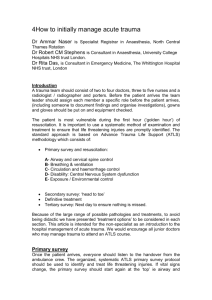
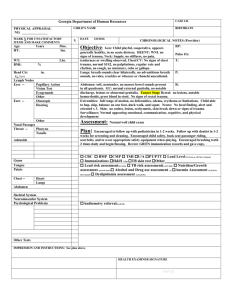
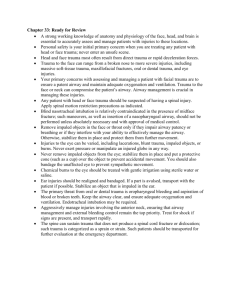
Management of patients with multiple trauma Prof. M K Alam MS; FRCS ILO’s Incidence of trauma Causes and types of trauma Timing and mode of death in trauma patients and its effect on trauma management. Pre-hospital care and triage Hospital care Primary survey and initial management Secondary survey Pathophysiology of common injuries Investigations during primary and secondary survey A brief outline of management of major injuries. Epidemiology • Trauma remains the most common cause of death between the ages of 1 and 44 years. • Affects a disproportionate number of young people- the burden to society in terms of lost productivity, premature death, and disability is considerable. • A major public health issue. Arab News 16th Feb. 2014 Arab News 3rd March 2014 Arab News 16th Feb 2014 • 20 deaths daily on the Kingdom's roads. • Last year- 707 amputations due to RTA. • Accidents increased by 78% in the KSA recently • Affecting mostly young between 18 and 22 years • Around 30% of those injured are permanently disabled. • The state has spent SR21 billion treating such patients Causes of trauma • • • • • • • • • RTA or MVA Pedestrian trauma Fall from height Assault Firearm injuries Knife Industrial accidents Natural disasters Explosions Types of trauma • Blunt trauma results of an impact from blunt object • Penetrating trauma results from an object piercing the body • Assessment and diagnosis of blunt injuries are more difficult than of penetrating injuries • Multi-trauma- injury affecting simultaneously different organ and body system Trimodal death in trauma • Immediate: Within seconds or minutes after injury- 50% of deaths due to injury to the aorta, heart, brainstem, or spinal cord or by acute respiratory distress. • Early: Within hours of injury- approximately 30% of deaths. Half of these deaths are caused by hemorrhage and the other half by central nervous system (CNS) injury. These patients can be saved by appropriate treatment (golden hour). • Late: peaks from days to weeks, mortality due to infection and multiple organ failure. Improvement in mortality • Early deaths: Prevention and control program by legislation and behavior modification • Later deaths: • • Trauma centers providing better care. Better understanding of pathophysiology of multiple organ failure and brain injury Pre-hospital care • Delivery to the hospital for definitive care as rapidly as possible- scoop and run • Only critical interventions at the scene • Airway established, hard collar, spine board, control any external hemorrhage • Infusion on way to the hospital Triage • Definition: Prioritizing victims into categories based on their severity of injury, likelihood of survival, and urgency of care. • Goals: – Identify high-risk injured patients who would benefit from the resources available in a trauma center. – Limit the excessive transport of non-severely injured patients so that the trauma center is not overwhelmed. Hospital care • ATLS approach • A well defined order • Primary survey- initial assessment and management • Treat the greatest threat to life • Immediate intervention as the threat to life is identified • Detailed history not essential • Re-evaluation of initial management • Secondary survey- a head to toe evaluation Primary survey • ABCDE • Airway & cervical spine protection • Breathing • Circulation • Disability (neurologic assessment) • Exposure and Environmental control Primary survey- a team approach • Simultaneous diagnosis and treatment by multiple providers • Reduces the time to assess and stabilize a multiple trauma patients • Team should be organized before patient arrival. • Leadership and unity of command are essential Primary survey-one clinician Do not perform subsequent steps in the primary survey until after addressing life-threatening conditions in the earlier steps. Part II A Airway & cervical spine • Verbal response: Salam! How are you? Airway is compromised if: • No response- unconscious , airway obstruction • Noisy breathing • Severe facial trauma • Oropharyngeal bleeding or foreign body • Patient agitated - hypoxia Airway & Cervical spine • Adequacy of airway- completed within seconds • Open the front of the collar for airway manipulation • Maintain manual stabilization by an assistant • Oropharyngeal airway/ bag valve mask ventilation • Oxygen supplement + pulse oximetry • Rapid-sequence endotracheal intubation • Frequent reassessment for airway compromise Difficult airway • Surgical airway when oral intubation cannot be accomplished: – Cricothyroidotomy –Surgical – Percutaneous needle technique- only temporary – Tracheostomy (laryngeal injury) B BREATHING Life threatening injuries to look for: • Tension pneumothorax • Open pneumothorax (open chest wound) • Flail chest with underlying pulmonary contusion • Massive hemothorax BREATHING • Dyspnoea • Unilateral diminished chest expansion • Bruising/ abrasion • Distended neck vein • Trachea deviated to the opposite side • Percussion: dull - haemothorax Hyper resonant - Pneumothorax • Diminished/ absent breath sound Tension pneumothorax Pathophysiology • Collapsed lung acts as a one-way valve • Each inhalation- additional air accumulate in the pleural space. • Normal negative intrapleural pressure becomes positive, depressing the ipsilateral hemidiaphragm, pushing the mediastinal structures into the contralateral chest • Contralateral lung is compressed, the heart is rotated about the superior and inferior vena cava, decreasing venous return and cardiac output while distending the neck veins Tension pneumothorax Clinical features & treatment • • • • • • • • Respiratory distress Tracheal deviation away from the affected side Lack of or decreased breath sounds Distended neck veins or systemic hypotension Subcutaneous emphysema, hyper resonance Treatment: x-ray confirmation not required Wide bore needle in 2nd inercost. space, mid clavicular Chest tube in 5th intercost. space, ant. axillary line Open pneumothorax or sucking chest wound Pathophysiology • Full-thickness loss of the chest wall: free communication between the pleural space and the atmosphere. • Collapse of the lung on the injured side • If the diameter of the injury is greater than the narrowest portion of the upper airway, air will preferentially move through the injury • impair ventilation on the contralateral side Open pneumothorax Management • Complete occlusion of the injury may result in converting an open pneumothorax into a tension pneumothorax. • Initial treatment: occlusive dressing, which is taped on three sides over the wound • Dressing permits effective ventilation, while the untaped side allows accumulated air to escape from the pleura • Definitive treatment: wound closure and tube thoracostomy Flail chest with pulmonary contusion Pathophysiology • Four or more ribs fractured in at least two locations • Paradoxical movement of free-floating segment may occasionally compromise ventilation. • More importantly, an underlying pulmonary contusion may compromise oxygenation or ventilation • Initial chest x-ray underestimates the degree of contusion. • The lesion evolve with time and fluid resuscitation. Flail chest with pulmonary contusion Management • Respiratory failure in these patients may not be immediate • Frequent re-evaluation is needed. • Intubation and mechanical ventilation is required Massive hemothorax • • • • • • • Accumulation of >1.5L of blood Disruption of large vessel Flat neck vein Dullness on percussion No breath sound Shock Management: Chest tube in 5th space, fluid resuscitation. Thoracotomy if significant bleeding continues. Part III C Circulation • Assessment of cardiovascular compromise and management • Is the patient in shock? • Is there any external bleeding source? • Any internal hemorrhage? Circulation Pathophysiology • Shock is secondary to hemorrhage in most trauma patients • Patient can be in shock before developing hypotension • Hypotension- a sign of decompensation (class III ) • 5 locations for major blood loss: Chest Abdomen Pelvis and retroperitoneum Multiple long bone fractures ( lower limb) External hemorrhage Pathophysiology of blood loss • • • • • Responses are compensatory Progressive vasoconstriction- skin, muscle, viscera Tachycardia to preserve cardiac output Increased peripheral resistance- catecholamines Venous return preserved in early stage by reduced blood volume in venous system • Continued bleeding- shock develops • Inadequate tissue perfusion, metabolic acidosis Classes of hemorrhagic shock Class I Class II Class III Class IV Blood loss Up to 750 (ml) 750- 1500 1500- 2000 > 2000 Pulse <100 >100 >120 >140 BP Normal Normal Decreased Decreased Circulation Indicators of shock in trauma patients • • • • • Tachycardia* Agitation Tachypnea Sweating Cool extremities • Weak peripheral pulse • Decreased pulse pressure • Hypotension • Oliguria Circulation Cardiogenic shock • Tension pneumothorax- most common cause, Pericardial tamponade(penetrating trauma), Myocardial contusion • Beck’s triad- hypotension, distended neck vein (raised CVP >15 cm H2O), muffled heart sound • CVP: Hemorrhagic <5 cmH2O • Dysrhythmias in contusion • Ultrasonography : helpful in diagnosis • Treatment: fluid resuscitation, pericardiocentesis Circulation Neurogenic shock • Loss of sympathetic tone due to cord injury • Hypotension, warm well perfused limbs, diminished/absent motor function • Bradycardia • Management: IV fluid, vasopressor, corticosteroids Circulation Septic shock • • • • • • • Delayed arrival Penetrating abdominal injuries Early septic shock- normal circulating volume Tachycardia Warm skin Systolic close to normal, Wide pulse pressure Circulation Initial management • External haemorrhage- compression dressing • IV access- two peripheral catheters • ECG monitoring • Blood sample- typing and lab. investigations • Initial resuscitation:1-2L of Ringer's lactate or NS • Packed red blood cells if no response • Foley’s catheter: urine output is .5 mL/kg/hour in adult Circulation Initial management Search for any source of blood loss: • CXR, X-ray pelvis, FAST (focused abdominal sonography in trauma) • If fracture pelvis is found pneumatic antishock garment or a bed sheet wrapped around the pelvis may be applied Evaluation of fluid resuscitation • • • • • BP and pulse rate Urine output (0.5ml/kg/hour) Mental status and skin color/temperature CVP Acid/base status Management decisions Rapid responders • Hemodynamics return to normal after fluid resuscitation • Hemodynamics remain stable even after reducing infusion to maintenance rate. • Probably bleeding has stopped spontaneously • Continued evaluation for source of bleeding • May still need surgery Management decisions Transient responders • Decompensate once fluid resuscitation is slowed down • There is ongoing bleeding or inadequate resuscitation • Increase fluid resuscitation and blood transfusion (type specific or O negative) • ?Surgical intervention Management decisions Non-responders • Fail to respond to fluid and blood resuscitation • Major blood loss (>40%) & ongoing loss • Immediate surgical intervention • ? Non-hemorrhagic shock (cardiogenic) • Echocardiography • CVP Part IV D Disability Neurologic evaluation • Level of consciousness measured by the Glasgow Coma Scale (GCS) • If the GCS is used in intubated and paralyzed patients, record should be made • Pupillary response can still be assessed in a paralyzed patient Glasgow Coma Scale (GCS), Total = 15 Eye response Vocal response Motor response Spontaneous 4 Oriented 5 Obeys commands 6 To voice 3 Confused 4 Purposeful movement to pain 5 To pain 2 Inappropriate words 3 None 1 Incomprehensible words 2 Flexion to pain 3 None Extension to pain 2 None 1 *** *** 1 *** Withdraw from pain 4 Head injury severity • Mild • Moderate • Severe GCS ≥ 13 GCS 9- ≤ 12 GCS ≤ 8 E Exposure/ Environment control • Completely undress the patient • Perform a rapid head-to-toe examination • Identify any injuries to the back, perineum, or other areas that are not easily seen in the supine position • Unexpected injuries may be discovered • Once assessment completed, cover the patient with blanket ( prevent cold exposure) Secondary Survey • Only after completion of primary survey(ABCDE) • Life threatening injuries have been dealt • Normalization of vital signs • A head to toe evaluation • Detailed history and examination • Continuous reassessment of vital signs • Additional lab. & radiological tests and collecting results • Additional tubes, lines and monitoring devices • Priorities and plan definitive management of all injuries Head injury • Traumatic brain injury (TBI)- the leading cause of death in trauma patients- 50% of all traumatic deaths. • Primary injury- the anatomic and physiologic disruption that occurs as a direct result of trauma • Secondary injury- extension of the primary injury, result from local swelling, increased ICP, hypoperfusion, hypoxemia, or other factors. • Aim- detection and treatment of primary injury and prevention of secondary injury Head injury- management • Maintain BP >90 mmHg, PaO2 >60 mmHg • Assess GCS and lateralizing signs- pupil and motor function • Pupillary asymmetry >1 mm suggests intracranial injury • Larger pupil is on the side of the mass lesion • Extremity weakness- detected by testing motor power • CT scan head- accurate localization of the lesion • Epidural or subdural hematoma causing mass effect evacuated • Diffuse axonal injury- maintain cerebral perfusion and prevent rise in ICP Spinal cord injuries • Intensive hospital care, long-term rehabilitation, life-long care. • Initial care- strict immobilization of the spine • Complete neurologic assessment • Steroid therapy must be initiated within a few hours of injury • Injuries above C3- are apneic, need intubation • between C3 and C5 – may need intubation later • Complete transection- poor prognosis • Preservation of remaining function Thoracic injuries • Life-threatening : tension pneumothorax, massive hemothorax, open pneumothorax, flail chest, and cardiac tamponade • Rib fractures, sternal fracture, lung contusion, Injuries to trachea, bronchi, heart, diaphragm, esophagus, thoracic aorta • Diagnostic modalities: CXR, ultrasonography, chest CT, esophagography, esophagoscopy, bronchoscopy, and angiography Part V Abdominal injuries • 25% of all trauma victims require abdominal exploration. • Physical examination- inadequate to identify intraabdominal injuries • Diagnostic modalities- CXR, FAST, DPL,CT & laparoscopy • Blunt trauma: • Hemodynamically stable- CT scan , • Hemodynamically unstable- FAST Diagnostic peritoneal lavage (DPL) • Insert catheter below umbilicus under LA and full asepsis and saline (1L NS) infusion into peritoneum • Returning fluid is bloody- +ve lavage • Rapid and safe • Bloody aspirate- laparotomy • Do not determine origin of blood • Too sensitive • Does not evaluate retroperitoneal injury • Replaced by FAST and CT scan FAST- focused abdominal sonography in trauma • Superseded DPL in assessment of abdominal trauma • 98% sensitivity for hemoperitoneum Abdominal injuries (penetrating) • All gun shot injuries- urgent surgery • Stab (knife) injury: Hemodynamically stable- CT scan, surgery only if intra-abdominal injuries found Hemodynamically unstable- surgery Splenic injury • Most frequently injured in blunt trauma (personal series) • History of injury to the left side of the chest, flank, or left upper part of the abdomen • Bruising, pain tenderness- lower chest and upper abdomen on left side • Diagnosis- CT in hemodynamically stable patients FAST or exploratory laparotomy in an unstable patients Splenic injury Non-surgical management (70%) • Hemodynamically stable patients: • FAST, CT for diagnosis • No other intra-abdominal injury requiring operation • Admission to ICU for continuous monitoring • Serial Hb. , & repeated abdominal assessment • If hypotension develops - taken for surgery Splenic injury Surgical management • Hemodynamically unstable • FAST: splenic injury, free fluid (hemoperitoneum) • Surgery- splenectomy • Polyvalent pneumococcal vaccine (pneumovax) Liver injury- pathophysiology • Susceptible to injury due to large size(1200-1600 g) • Covered by bony thoracic cage • Injury frequency - only 2nd after spleen( personal series) • Highly vascular- only 4% of body weight but 28% of total body blood flow • Double blood supply- portal vein & hepatic artery • Draining hepatic veins- short and thin walled Liver injury • Spontaneous hemostasis- 50% of small lacerations • Profuse bleeding from deep hepatic lacerationsa formidable challenge • Mortality rate 8%- 10%, morbidity rate from 18%-30%, • Diagnosis: FAST in hemodynamically unstable, CT scan in hemodynamically stable • Management based on hemodynamic status Liver injury Non-operative management • • • • • • • Hemodynamically stable patients CT scan No other indications for abdominal exploration ICU admission for close observation Serial hemoglobin estimation Transfusion requirements of <2 units of blood Surgery- if become unstable Liver injury Surgical management • Principles of surgical management: control of bleeding, removal of devitalized tissue, and adequate drainage. • Bleeding vessels & biliary radicles are individually ligated • Pringle’s maneuver • Perihepatic packing- when fail to control hemorrhage • Packs removed in 48 hours Pancreatic injuries • • • • • • Pancreatic injury is rare Caused by penetrating injury or direct blow Diagnosis is difficult to make CT scan, elevated serum amylase may help No duct injury: simple drainage Ductal injury: distal resection Bowel injuries • Mostly due to penetrating trauma • Also seen after blunt trauma • Features of peritonitis • CT scan free air in peritoneum/ contrast leak • Small bowel: Suture repair • Colon: suture repair± proximal colostomy Renal injuries • Minor- renal contusion (85%) Conservative management • Major: Deep medullary injuries with extravasation Vascular injuries Surgical repair Thank you! Part VI Case for discussion • An ambulance is bringing a young man who was riding a motor bike. He was thrown from the speeding motor bike on a bending road. He was not wearing a safety helmet. His left leg appears grossly deformed. • The ambulance has informed ER before bringing him. • You are the only doctor in ER • What to do? Preparation before patient arrival • Airway equipment, cervical collar, pulse oximetry, ECG monitor, oxygen • Laryngoscope, Needles, chest tubes, under-water seal, • Minor op. set, local anaesthetic, • IV fluids at room temp. • Blood sample tubes • Splints • Radiologist and technician • Foley catheter and urine bag Management in a hospital • Patient arrives in hospital • Patient is on a spinal board • Deformed left lower limb with blood stain on cloth? • What to do next? Primary survey • • • • • A B C D E Assessment of airway • Talk to the patient Danger signs • Not talking • Oro-facial bleeding • Confused • Agitated • Neck hematoma Airway management • • • • • • • • Clearing oral cavity Oropharyngeal / bag valve mask Chin lift / jaw thrust Oral endotracheal intubation Surgical methods Adjuncts: oximetry, oxygen Cervical collar if not applied during transport Manual in-line support by an assistant Breathing • Patient continues to be dyspnoeic? • Oxygen saturation not improving? • Chest injuries to look for and manage 1. 2. 3. 4. Tension pneumothorax Massive hemothorax Flail chest Open chest wound pO2 and respiratory rate improves Circulation • • • • • • • Pulse, BP,RR Any external bleeding? Look at his deformed limb 2 IV line, blood samples RL or NS 1-2 L as bolus rapidly Quick response: slow down iv to maintenance Transient response: BT ?bleeding No response: ?Major bleeding ? Inadequate resuss. ?non- hemorrhagic shock ( cardiogenic, spinal, septic) Hemorrhagic vs Non-hemorrhagic shock • Neck vein • Pulse (rhythm, volume, rate) • Heart sound • ECG • CVP Later : Spinal injury Late presentation with abdominal injury Major bleeding sources • Chest: massive hemothorax • Abdomen: hemoperitoneum • Pelvis: pelvic & retroperitoneal hematoma • Lower limb fractures Investigations for bleeding source • • • • • CXR* FAST DPL CT X-ray pelvis* *X-ray c spine- the only other x-ray allowed during Primary survey Disability & Exposure • GCS • Full exposure including the blood mark on his lower limb. • Splint the limb- if not already done during assessment for external hemorrhage • Cover patient with a blanket • Reassess ABCD Secondary survey • Only after completion of primary survey(ABCDE) • Life threatening injuries have been dealt • Normalization of vital signs • A head to toe evaluation • Detailed history and examination • Continuous reassessment of vital signs • Additional lab. & radiological tests and collecting results • Additional tubes, lines and monitoring devices • Priorities and plan definitive management of all injuries Thank you!