Building a Strategy to Support Medical Device Integration and Alarm
advertisement

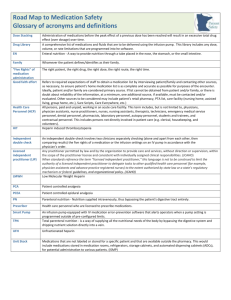
The World of Connectivity – Building a Strategy to Support Medical Device Integration and Alarm Management Presented by Izabella Gieras, MS, MBA, CCE Jennifer Jackson, MBA, CCE Huntington Memorial Hospital Cedars-Sinai Medical Center October 23, 2015 Huntington Hospital Courtesy of Huntington Hospital Huntington Hospital • • • • • • • • 625 licensed beds Bariatric & Stroke Center Magnet Recognition 3 Davinci Robotic Systems 18 Operating Rooms (4 MIS suites) Skills Labs 5 Cath Labs & IR Suites 9000 medical devices Courtesy of Huntington Hospital • • • • • • 280 applications 450 servers with 200+ TB storage 1000+ wireless access points 4500+ end user computing devices 300+ hospital owned smart phones 60 Clinical & Information Technology employees Agenda Background Healthcare Environment Healthcare Technology Management at Huntington Hospital & Cedars-Sinai Health System Medical Device Integration Alarm Management Background Healthcare Environment Regulatory Requirements Patient Environment Healthcare Technology Management in Medical Device Integration Medical Device Integration Connectivity – the physical interconnections between medical devices, the network, and the hardware and software required to capture data and make it available for use in the Electronic Health Record (EHR) or other clinical applications. www.diabetesmine.com ECRI Institute Top 10 Health Technology Hazards www.ecri.org 1. Alarm Hazards: Inadequate Alarm Configuration Policies and Practices 2. Data Integrity: Incorrect or Missing Data in EHRs and Other Health IT Systems IT systems AAMI Survey 2012 Survey of healthcare technology management professionals in 1,900 different U.S. hospitals placed interoperability issues top of the list AAMI’s list of Top 10 Medical Device Challenges: • Medical devices and systems on the IT network (cited by 72 % of respondents) • Integrating device data into electronic health records (EHRs) (cited by 65 % of respondents) www.aami.org WHI (West Health Institute) Report Improving interoperability between medical devices and EHRs in hospitals could save more than $30 billion a year while improving patient care and safety. • Increased capacity for treatment as a result of shorter lengths of stay ($18 billion) • Increased clinician productivity because of less time spent entering device data manually into EHRs ($12 billion) • Avoidance of redundant testing ($3 billion) • Reduction of adverse events ($2 billion). www.westhealth.org WHI Report continued • More than 90% of hospitals use six or more types of devices that could be integrated with EHRs. Examples: patient monitors, defibrillators, ECG machines, vital sign monitors, ventilators and infusion pumps. • Yet only a third of hospitals integrate any medical devices with EHRs, and those that do, on average, integrate only three types of devices. The cost of medical device integration can range from $6,500 to $10,000 per bed in one-time costs, plus up to 15% of that in annual maintenance costs. Business Case for Huntington Hospital Huntington’s EHR Implementation Vision Statement A clinical and operationally focused implementation that will integrate business and clinical information systems to support the goal of using technology to improve quality, patient safety, productivity and physician alignment. Business Case for Huntington Hospital continued Huntington’s EHR Partner Philosophy Create an environment where all devices are integrated and contextually aware to ensure the right data is present in the right format at the right time to improve health outcomes. Across the care continuum, medical devices contain life-critical information. It is essential for health care providers and patients to harness this information to make the best decisions regarding health. http://cerner.com/solutions/Medical_Devices/ Huntington Hospital Timeline 6/2012 – 2/2014 Implementation 2/2014 – 3/2014 Readiness & Go Live 3/2014 – 6/2014 Stabilization 6/2014 - Today Optimization Beyond Today IMPLEMENTATION EHR Implementation Scope Full EHR Implementation 40+ solutions Financial ERP Revenue Cycle Clinical Physician 6/2012–2/2014 Implementation Complete workflow re-design with new functionality House-wide CPOE & Physician Documentation Bar-coded Medication Administration Device Integration expansion (from ~30 to 200 beds) Imaging Voice Recognition Patient Portal Device Integration Scope Wired and Wireless Physiological Monitors PICU: 8 CCU: 30 Surgery:19 PACU:17 ED:56 Telemetry: 43 Endo:3 Anesthesia Gas Machines Main Surgery: 16 L&D: 3 Endo:1 Angio: 1 Cath Lab: 1 Fetal Monitors: 30 6/2012–2/2014 Implementation Device Integration Considerations Clinical needs assessment Device types Wireless vs Wired Software version Age of equipment Physical location Type of mounts Position 6/2012–2/2014 Implementation EMR Device Setup 6/2012–2/2014 Implementation Datalux device (workstation) CE (Connectivity Engine) device Device Integration Validation Liaison with the Anesthesiologists and clinicians 6/2012–2/2014 Implementation Device Validation Tool Spreadsheet with collected data to enable repeatability Test every device and every data element Schedule for testing Overnight or early hours in Surgery CE device and adapter tweaking Testing workstation Cheat sheet binder Close collaboration between CT (Clinical Technology), IT and end users Testing Station in CT 6/2012–2/2014 Implementation Device Integration Validation 6/2012–2/2014 Implementation READINESS & GO LIVE Go Live Readiness End user training 2/2014 – 3/2014 Readiness & Go Live Completion of Final Testing Mock Go Lives and Detailed Walk through of Cutover Multiple layers of Readiness Assessments Departmental Leader Readiness Assessment Go No Go Decision Steering Committee Board Downtime the Night of Go Live Downtime was scheduled for 2 ½ hours 2/2014 – 3/2014 Readiness & Go Live Downtime was actually 6 ½ hours due to issues encountered EHR Login issue PACS & Pyxis Conversion Communication Plan Posters, Memo, and Tray liners (Patients & Visitors) Team Shirts – Teal (staff) and Grey (physician) Shift Change Meetings (Super users & Technical Staff) Leadership Touch base Regular Project Newsletter Daily Reminders to Staff SharePoint Communication site Hot Sheets – Color Coded by Discipline 2/2014 – 3/2014 Readiness & Go Live STABILIZATION Stabilization Clinical Technology support Proper training to all CT staff Sign off before go live Service work flow Response time Logging calls Collaboration between IT, Nursing Informatics and end users Spare par level Configured datalux device Downtime procedures 3/2014 – 6/2014 Stabilization Service Workflow 3/2014 – 6/2014 Stabilization OPTIMIZATION Optimization Evaluating capability for integration for all new Clinical Technology purchases Questions added for the procurement of equipment Assessment of available applications from EMR vendor for overall consolidation Upgrades every 12-18 months 6/2014 - Today Optimization BEYOND TODAY Updated Timeline Beyond Today 2010 - 2011 Early Pilot • Wired CCU Monitors 2012-2014 Strategy & Phase I • Wired & Wireless Monitors (Critical Care Areas) • Anesthesia Gas Machines • Fetal Monitors • Blood Gas Analyzers • Lab Instruments • Point of Care Alarm Mgmt Building the Foundation 2015 Phase I optimization 2015 Planning for Future • Expand Wired &Wireless Monitors • Vents Alarm Mgmt Implementation • Pumps • Balloon Pumps • EKG Machines • Vital Sign Monitors • Other Devices? HEALTHCARE TECHNOLOGY MANAGEMENT IN ALARM MANAGEMENT Alarm Mgmt – Building the Foundation and Beyond What Huntington Has Done 2003 - Committee was formed in response to the initial TJC SEA on Clinical Alarms 2013 - Formation of Clinical Alarms Management Committee 2014 - Alarms survey - Preliminary data collection (labor intensive process) - Invited “middleware” vendors for presentations to evaluate strengths and shortcomings of each system - Evaluated medical equipment inventory with clinical alarms - Invited to the AAMI National Alarms Coalition What Huntington Has Done cont. 2015 (completed and in progress) - Changed alarm settings on two nursing units (case study) - Defined critical equipment with critical alarms - Completed a Risk Assessment tool on critical equipment - Reviewed alarm settings for each critical equipment - Performed a short alarm management model survey - Update the hospital policy (addressed many 2016 deliverables) Upgrade of all central stations/servers to PicIx Evaluate a middleware vendor for alarm management solutions Create and deploy educational initiatives Prioritized technologies (monitors, vents, infusion pups, etc) Updated alarm default settings Rhythm Asystole VTach Default 4 seconds (adjustable) Rate >150 > 3 PVCS Rhythm Non Sustained VT Ventricular Rhythm Run PVCs Pair PVCs R on T PVCs Ventricular Bigeminy Ventricular Trigeminy PVCs Multiform PVCs Pacer Not Capture Pacer Not Pace Missed Beat Pause SVT AFib Irregular HR Cannot Analyze ECG Default On On, >14 PVCS On, > 2 PVCs (not adjustable) On On On On On, >10/minute On On On On 2 seconds On, > 150/minute, > 5 SVBs On On On Recommended Change None None Recommended Change Off On >20 PVCS Off Off Off Off Off Off Off Off Off Off None None None None None Courtesy of Huntington Hospital Izabella Gieras, MS, MBA, CCE Director, Clinical Technology Izabella.Gieras@huntingtonhospital.com Jennifer Jackson: Introduction Biomedical Engineer Clinical Engineer Hospital CE-IT Leader Medical Device Interoperability Advocate ACCE 2015 Professional Achievement in Technology Award/Professional Development Award CIMIT Edward M. Kennedy Award for Health Care Innovation in 2007 as member of the Medical Device “PnP” Interoperability Team Cedars Sinai: Leading the Quest Established in 1902, Cedars-Sinai Medical Center is renowned for: • Providing the highest quality patient care • Expanding scientific and medical knowledge through research that benefits patients • Educating healthcare professionals for the future • Improving the health status of the community Overview of Cedars Sinai Established in 1902 and located in Los Angeles, California By the Numbers, from our 2014 Community Report: 886 licensed beds, Level I Trauma Center 251,803 Patient days 630,269 Outpatient visits Approximately 690 per day Approximately 1730 per day 85,305 Emergency Department visits Approximately 235 per day $43.4 million in research funding from NIH and other federal sources $652.6 million in total quantifiable community benefits, including the unreimbursed cost of caring for Medicare patients Primary service area includes 3.3 million people Cedars Sinai: Not All Our Heroes Practice Medicine From the HIMSS Analytics Press Release: "Cedars-Sinai is one of the most fully deployed and automated facilities we have encountered in the HIMSS Analytics Stage 7 program. With all of their progress on device integration, including fully integrated smart pumps, Cedars-Sinai has approached a new level of patient safety, even among stage 7 facilities.” -John Hoyt, executive vice president of HIMSS Analytics CEDI Mission Statement In close collaboration with clinicians, administrators, and other technology groups, Clinical Engineering and Device Integration (CEDI) promotes quality patient care through the appropriate and safe use of medical device technology. Clinical Engineering and Anesthesiologists meeting to discuss the hardware mounting related to CSLink Anesthesia Record implementation. Clinical Engineering and nursing working together to plan out unit closures for the nurse call replacement. We strive to be a center of excellence for innovative and robust solutions that promote leadership in delivering healthcare related services. The Clinical Engineering & Device Integration Team •Biomedical Equipment Technicians •Image Guided Systems Technicians •Clinical Systems Specialists •Clinical Systems Engineers •Project Specialists •Administrative Staff What Makes Us Different in the way we manage medical device systems Unique organizational structure Independent department within IT Work side-by-side with applications and technical teams Unique job roles Image Guided Systems Technicians Much more clinical than a ‘typical’ BMET, working side by side with surgeon during procedures to ensure the technology is properly aligned and functioning Clinical Systems Specialists Stronger IT skill set than a ‘typical’ BMET More of the technical lifecycle within one department Building device records in the EHR Testing and maintaining orders/results interfaces Project management Technical support System optimization Reporting up into IT…and we are thriving… CIO Manager EIS Finance Chief Technology Officer Director, Clinical Engineering Chief Application Officer Director, R&D Servers, SAN Device Integration EPIC Application support Wearables integration Security Clinical Communication PACS/VNA Systems Integration Network Nurse Call/RTLS Mobile device team Clinical Engineering New technology evaluation OR Clinical Engineering clinical and operational benefits of technology interoperability, 48 Director, Research Computing IRB collaboration Director, Business Systems CMMS Peoplesoft Snapshot of CSMC Medical Device Connectivity Infusion Pumps •1523 Infusion pump brains wirelessly communicate • Within infusion pump system: used to push datasets and download logs • With EHR: bidirectional interface; order goes to pump, flow rate and volume goes to patient chart Patient Monitoring •~255 telemetry patients’ data imported to EHR (288 max – will increase in 2016) •690 multi-parameter monitoring devices imported to EHR •120 terminal servers in critical care areas for connection to ventilators, urimeters, CCO monitors, BIS monitors, etc.. •85 anesthesia machine ‘systems’ •Mobile vital signs collection – data validated instantly •Currently trialing wireless pulse oximetry devices with integration to alarm management and EHR Snapshot of CSMC Medical Device Connectivity Cardiology •35 EKG carts are wireless •Orders/results for cath lab hemodynamic systems •Ambulatory blood pressure system integrated (PDF report uploaded) •Pacemaker reporting system integrated (PDF report uploaded) Fetal monitoring •24 Fetal monitors (LDR + Prenatal Clinic) interfaced with fetal monitoring system, then to EHR •Additional integration with smartphone application for near-real time remote monitoring Alarms/Alerts •Nurse Call alarms/patient requests– sent to smartphones •Pulse Oximetry and some cardiac monitoring – sent to smartphones •Medical Device (“aux”) jack in each room for technologies not ready for network connectivity (i.e. chair exit alarm devices) •Tele monitor based alarms managed through central monitoring, filtered Additional Supporting Evidence on the Need for Device Integration For Device Integration in OR/Procedure Areas Anesthesia Information Management Systems: A Review Of Functionality And Installation Considerations JM Ehrenfeld et all (2011) Called out benefits with device integration with anesthesia information management systems • Specific to Positive Impact on Patient Safety • • • • • Provision of real-time intraoperative decision support Allows the anesthesia care team to focus on the patient, rather than recording vital signs Better legibility and availability of historical records More precise recording of intraoperative data & patient responses to anesthesia Specific to positive impact on Anesthesia Practice • • • • • • Provides precise, high-resolution records which can be used for educational purposes Enables researchers to rapidly find rare events or specific occurrences across a large number of cases Facilitates individual provider performance tracking Allows better quality assurance functionality through the creation of more complete and precise records Integration with other hospital databases can allow assessment of short and long term patient outcomes Provision of additional legal protection via the availability of unbiased, precise information For More Automated Medication Administration Executive Summary: the State of the Science on Safe Medication Administration symposium. KG Burke (2005) Provides great summary of the problem •It’s estimated that five medication errors occur per 100 medication administrations. •Adverse drug events (ADEs) occur at an estimated rate of 6.5 per 100 hospital admissions. •One of every three ADEs related to medication errors occurs during administration. •It has been estimated that 56% of medication errors are related to prescriptions. •IV medications and infusion pumps are also being increasingly viewed as safety concerns. Quite simply put: “Currently available smart pumps will fail to generate meaningful improvements in patient safety until they can be interfaced with other systems such as the electronic medical record, computerized prescriber order entry, bar coded medication administration systems, and pharmacy information systems.” For More Automated Medication Administration The impact of traditional and smart pump infusion technology on nurse medication administration performance in a simulated inpatient unit. P Trbovich (2010) Discusses benefits of smart pumps • Pre-defined drug library uploaded to each pump • Each drug has a set of limits • Provides feedback to nurse • Dose or infusion rate is too high or too low for that medication • Intended to catch majority of potential programming errors • Can catch estimated 58% of potential medication errors Also discusses the opportunities for error • Current state can catch only estimated 58% of potential medication errors • Nurse can still bypass using the library (time-saving) • Still allows for programming errors within the set limits Anesthesia Information System & IV Pump Integration IMPLEMENTATION ACROSS THE ENTERPRISE: TWO CASE STUDIES Device Integration in the OR/Procedure Areas •91 anesthesia machines converted •Devices integrated per machine: o o o o o o Philips monitor Anesthesia machine BIS monitor CCO monitor INVOS monitor Tangent o Neuron (as the data concentrator) •Total devices integrated/communication with EPIC – 490 o 4 different configurations were created for the different areas All stakeholders involved with configuration and developing technical support model Clinical and Technical support during Supporting complex technology integrations Pump Integration IV Pump Integration went into production at Cedars-Sinai on June 7, 2014. • All adult inpatient locations using barcoded medication administration protocols as of January 2014 • Considered an improvement to patient safety: • Improved our compliance with drug library use • Reduced the frequency of reprogramming or editing the pump program before starting an infusion From CS-Link to IV Pump: Drug Name, Dose, Flow Rate From IV Pump to CS-Link: Flow Rate, Volume Infused Pump Integration Workgroup Structure New pump deployment Interfaces Drug Dataset alignment EPIC 2012 integration Workflow analysis Testing Steering Committee Training Workflows, workflows, workflows Training and assessment clinical and operational benefits of technology interoperability, 61 6/7/2014 6/9/2014 6/11/2014 6/13/2014 6/15/2014 6/17/2014 6/19/2014 6/21/2014 6/23/2014 6/25/2014 6/27/2014 6/29/2014 7/1/2014 7/3/2014 7/5/2014 7/7/2014 7/9/2014 7/11/2014 7/13/2014 7/15/2014 7/17/2014 7/19/2014 7/21/2014 7/23/2014 7/25/2014 7/27/2014 7/29/2014 7/31/2014 8/2/2014 8/4/2014 8/6/2014 8/8/2014 8/10/2014 8/12/2014 8/14/2014 8/16/2014 Total Number of In-Scope Medication Orders 12,500 93% 93% 12,000 11,000 92% 91% Pump Integration Go-Live June 7, 2014 91% 92% 92% 92% 92% 92% 92% 91% 91% 11,500 90% 89% 88% 88% 10,500 87% 86% 10,000 85% Number of medication adminitrations initiated using Pump Integration (% of total in scope) Cedars-Sinai Pump Integration Utilization shown as % of in-scope medication orders 94% My “one-liner” about medical device integration Medical Device Integration standardizes clinical and technical workflows. If done right, you’ve spent more time defining the nontechnical processes than talking about the technology itself. Jennifer Jackson Director, Clinical Engineering & Device Integration jennifer.jackson@cshs.org @giengiakson THANK YOU AND QUESTIONS clinical and operational benefits of technology interoperability,