Pulmonary Hypertension
advertisement

The Basics of Pulmonary
Hypertension
Lana Melendres-Groves
Assistant Professor of Medicine
Director, Adult Pulmonary Hypertension Program
Division Pulmonary & Critical Care Medicine
UNMHSC
Objectives
•
•
•
•
•
•
•
Definition of PH/PAH and pathophysiology
WHO groups
Natural history of PAH
Clinical presentation/PE/studies
Timing and type of work-up
Who gets therapy
Monitoring of therapy
Case #1
• 27yo woman with PMHx significant for
exercise induced asthma and anxiety
presenting to the ED after “almost passing
out”.
• She has a 10mnth old daughter and felt that
maybe she just hadn’t gotten into shape after
having the baby.
• SOB when she tries to jog or walk up her
stairs.
Case #2
• 29yo man with HIV presenting to the ED with
2 month h/o of worsening SOB on exertion
that has dramatically worsened over the past
week to the point that he is now having SOB
at rest and feeling dizzy when standing not on
any medications.
• Recently moved from California and has no
information in our system.
Case #3
• 42yo obese woman who doesn’t like doctors
that presented after she had worsening
fatigue and sob with minimal activity.
• She is a hairdresser and overall is upset that
she is overweight so never steps on a scale.
• She doesn’t take any medications.
• Has noticed swelling in her legs.
• TTE shows severe RV enlargement and PASP of
95mmHg with rt to left shunt seen.
Case #4
• 65yo woman with little PMHx presenting with
SOB and exhaustion. Has no medical problems
that she knows of, just retired from teaching for
the past 40years in California and relocated to
Ruidoso, NM.
• Previously playing 18 holes of golf, now only able
to walk 15ft before needing to stop and rest.
• Massive LEE and decreased mobility of her hands.
Case #5
• 83yo woman has been healthy her whole life now
presenting with worsening fatigue with exertion.
• Previously able to swim for 30 minutes a day and
walk for 30min, now sob with much less. Unable
to keep up with her friend.
• Experiencing palpitations and chest pressure
intermittently.
• TTE shows mild RA and RV enlargement with a
PASP of 55mmHg
Case #6
• 52yo man with ESRD on HD, htn, DM, CAD,
cirrhosis from hep C and prior ETOH abuse
and mild COPD, no longer smoking, admitted
after missing two HD appointments with
profound fluid overload.
• Also notes that he has had worsening SOB
over the past year and fluid retention.
Normal Cardiac Hemodynamics
Diagnostic Definition: Pulmonary
Hypertension
Rest:
- Mean PAP >25 mmHg
PAH = above + PCWP or LVEDP <15 mmHg
– + PVR >3 WU
Associated with adverse changes
- In the pulmonary vasculature (arteriopathy)
- At the level of the right ventricle (hypertrophy)
No longer part of the definition:
Exercise:
- Mean PAP > 30 mmHg
Gaine et al. The Lancet, 1998.
Aberrant Pathways in PAH
Loss of Biological “Balance” in PAH
Vasodilation
Apoptosis
Vasodilation
Apoptosis
Vasoconstriction
Proliferation
Vasoconstriction
Proliferation
The Pathobiology Of Pulmonary Hypertension
Endothelium
elastic
lamina
SMC
serum leak
injury
SMC PROLIFERATION
& MIGRATION
5th World Symposium: Classification of Pulmonary
Hypertension
(Nice, France 2013)
1. Pulmonary Arterial Hypertension
1.1 Idiopathic PAH
1.2 Heritable
1.2.1. BMPR2
1.2.2. ALK1, ENG, SMAD9, CAV1, KCNK3
1.2.3 Unknown.
1.3 Drug- and toxin-induced
1.4 Associated with
1.4.1. Connective tissue disease
1.4.2 HIV infection
1.4.3 Portal hypertension
1.4.4 Congenital heart diseases
1.4.5 Schistosomiasis
1’ Pulmonary veno-occlusive disease (PVO) and/or
pulmonary capillary hemangiomatosis (PCH)
1’’ Persistent pulm hypertension of the newborn (PPHN)
2. Pulmonary hypertension due to left heart disease
2.1 LV Systolic dysfunction
2.2 LV Diastolic dysfunction
2.3 Valvular disease
2.3 Congenital/acquired left heart inflow/outflow
tract obstruction and congenital cardiomyopathies
3. Pulmonary hypertension due to lung diseases and/or
hypoxia
3.1 Chronic obstructive pulmonary disease
3.2 Interstitial lung disease
3.3 Other pulmonary diseases with mixed restrictive and
obstructive pattern
3.4 Sleep-disordered breathing
3.5 Alveolar hypoventilation disorders
3.6 Chronic exposure to high altitude
3.7 Developmental lung disease
4. Chronic thromboembolic pulmonary hypertension (CTEPH)
5. PH with unclear multifactorial mechanisms
5.1 Hematologic disorders: chronic hemolytic anemia
myeloproliferative disorders splenectomy.
5.2 Systemic disorders, sarcoidosis, pulmonary
Langerhans cell histiocytosis, lymphangioleiomyomatosis,
neurofibromatosis, vasculitis
5.3 Metabolic disorders: glycogen storage disease,
Gaucher disease, thyroid disorders
5.4 Others: tumoral obstruction, fibrosing mediastinitis,
chronic renal failure on dialysis.
Back to the Cases
• What do all the patients presented have in
common?
– Each patient was found to have pulmonary arterial
hypertension after full w/u and diagnosis by right
heart catheterization.
Pulmonary Arterial Hypertension
• Case #1: IPAH
• Case #2: PAH
associated with HIV
PAH
• Case #3: PAH assoc
with drugs/toxins
- The list gets longer and
longer
• Case #4: PAH assoc
with CTD
- Sometimes the PH presents
before other complications
of the disease
Drugs and Toxins Associated PAH
Definite
Possible
•
•
•
•
•
•
•
•
•
•
•
•
Aminorex
Fenfluramine
Dexfenfluramine
Toxic rapeseed oil
Benfluorex
SSRIs
Likely
•
•
•
•
Amphetamines
L-tryptophan
Methamphetamines
Dasatinib
Cocaine
Phenylpropanolamine
St John’s Wort
Chemotherapeutic agents
Interferon alpha/beta
Amphetamine-like drugs
Unlikely
• Oral contraceptives
• Estrogen
• Cigarette smoking
PAH
• Case #5: PAH assoc
with CHD
• Case #6: PAH assoc
with portal htn
Hemodynamic Classification of PH
(mean PAP >25 mm Hg)
Post-capillary PH
VC
RA
RV
PA
PC
Mixed
PH
Pre-capillary PH
Diagram courtesy of Teresa De Marco, MD, UCSF
PV
LA
LV
High-flow PH
(O2 sat run)
Ao
Hemodynamic Classification of PH
(mean PAP >25 mm Hg)
Post-capillary PH
PCWP>15 mm Hg; PVR normal
VC
RA
RV
PA
PC
PV
LA
LV
PVP LAP LVEDP
Diagram courtesy of Teresa De Marco, MD
Ao
Hemodynamic Classification of PH
(mean PAP >25 mm Hg)
Post-capillary PH
PCWP>15 mm Hg; PVR normal
MR
VC
RA
RV
PA
PC
PV
LA
LV
Ao
PVP LAP LVEDP
Systemic HTN
Myocardial Disease
AoV disease
Dilated CMP-ischemic/non-ischemic
Hypertrophic CMP
Restrictive/infiltrative CMP
Obesity related CMP
Pericardial disease
Diagram courtesy of Teresa De Marco, MD
Hemodynamic Classification of PH
(mean PAP >25 mm Hg)
Post-capillary PH
PCWP>15 mm Hg; PVR normal
VC
RA
RV
PA
PC
PV
LA
LV
PVP
PV Compression
Diagram courtesy of Teresa De Marco, MD
Ao
Hemodynamic Classification of PH
(mean PAP >25 mm Hg)
PAH
Lung diseases +/- hypoxemia
CTEPH
{
RA
RV
PA
PC
{
VC
Pre-capillary PH
PCWP <15 mm Hg;
PVR >3 woods units
Diagram courtesy of Teresa De Marco, MD
PV
LA
LV
Ao
5th World Symposium: Classification of Pulmonary
Hypertension
(Nice, France 2013)
1. Pulmonary Arterial Hypertension
1.1 Idiopathic PAH
1.2 Heritable
1.2.1. BMPR2
1.2.2. ALK1, ENG, SMAD9, CAV1, KCNK3
1.2.3 Unknown.
1.3 Drug- and toxin-induced
1.4 Associated with
1.4.1. Connective tissue disease
1.4.2 HIV infection
1.4.3 Portal hypertension
1.4.4 Congenital heart diseases
1.4.5 Schistosomiasis
1’ Pulmonary veno-occlusive disease (PVO) and/or
pulmonary capillary hemangiomatosis (PCH)
1’’ Persistent pulm hypertension of the newborn (PPHN)
2. Pulmonary hypertension due to left heart disease
2.1 LV Systolic dysfunction
2.2 LV Diastolic dysfunction
2.3 Valvular disease
2.3 Congenital/acquired left heart inflow/outflow
tract obstruction and congenital cardiomyopathies
3. Pulmonary hypertension due to lung diseases and/or
hypoxia
3.1 Chronic obstructive pulmonary disease
3.2 Interstitial lung disease
3.3 Other pulmonary diseases with mixed restrictive and
obstructive pattern
3.4 Sleep-disordered breathing
3.5 Alveolar hypoventilation disorders
3.6 Chronic exposure to high altitude
3.7 Developmental lung disease
4. Chronic thromboembolic pulmonary hypertension (CTEPH)
5. PH with unclear multifactorial mechanisms
5.1 Hematologic disorders: chronic hemolytic anemia
myeloproliferative disorders splenectomy.
5.2 Systemic disorders, sarcoidosis, pulmonary
Langerhans cell histiocytosis, lymphangioleiomyomatosis,
neurofibromatosis, vasculitis
5.3 Metabolic disorders: glycogen storage disease,
Gaucher disease, thyroid disorders
5.4 Others: tumoral obstruction, fibrosing mediastinitis,
chronic renal failure on dialysis.
Natural History of PAH: NIH Registry1,2
Percent survival
69%
56%
46%
38%
Predicted survival
Years
Predicted survival*
NIH = National Institutes of Health.
Predicted survival according to the NIH equation. Predicted survival rates were 69%, 56%, 46%, and 38% at 1, 2, 3, and 4 years,
respectively. The numbers of patients at risk were 231, 149, 82, and 10 at 1, 2, 3, and 4 years, respectively. *Patients with primary
pulmonary hypertension, now referred to as idiopathic pulmonary hypertension.
1. Rich et al. Ann Intern Med. 1987;107:216-223. 2. D’Alonzo et al. Ann Intern Med. 1991;115:343-349.
Survival by PAH Etiology
Prognosis in Mixed Treated/Untreated Cohorts
Percent survival
100
80
CHD
CVD
HIV
PPH
PoPH
60
40
20
0
0
1
2
3
4
5
6
Years
CHD = congenital heart disease; CVD = collagen vascular disease; HIV = human immunodeficiency virus; PAH = pulmonary
arterial hypertension; PPH = primary pulmonary hypertension; PoPH = portopulmonary hypertension.
McLaughlin et al. Chest. 2004;126:78S-92S
Symptoms
•
•
•
•
•
•
•
•
Breathlessness
Chest pain
Dizziness
Syncope
Loss of energy
Edema
Dry cough
Raynaud’s phenomenon
Physical Exam Findings in PAH
•
•
•
•
•
•
•
Increased jugular venous pressure
Accentuated split S2
Presence S3
TR murmur- heard best LL sternal border
Edema and/or ascites
Hepatojugular reflux
Skin- telangiectasias, Raynaud’s, Sclerodactyly
CXR
CT Chest
Pulmonary Arterial Hypertension: Detection and Diagnosis
Is there a reason to suspect PAH
Clinical history (symptoms, risk factors, family Hs.),
Exam, CXR, ECG
yes
no
No further
evaluation
for PAH
no
Is PAH likely?
Echo
Rationale
TRV to measure RVSP; RVE; RAE; RV Dysfunction:
yes
Is PAH due to LH disease?
Echo
yes
Dx LV systolic, diastolic dysfunction; valvular disease:
Appropriate treatment and further evaluation
if necessary, including R&LHC
no
Is PAH due to CHD?
Echo with contrast
yes
no
Is PAH due to CTD, HIV?
Serologies
yes
Dx abnormal morphology; shunt:
Surgery. Medical treatment of PAH or evaluation for
further definition or other contributing causes,
including R&LHC if necessary
Dx Scleroderma, SLE, other CTD, HIV: Medical
treatment of PAH and further evaluation for
other contributing causes, including RHC
no
Is chronic PE suspected?
VQ scan
McGoon et al. Chest 2004;126:14S-34S
Pulmonary Arterial Hypertension: Detection and Diagnosis
Is chronic PE suspected?
VQ scan
no
yes
Is chronic PE confirmed and operable?
Pulmonary angiogram
yes
VQ normal
no
Is PAH due to lung disease
or hypoxemia?
PFTs, arterial saturation
yes
Anatomic definition (CT, MRI may provide additional useful
but not definitive information):
Thromboendarterectomy if appropriate or medical
treatment; clotting evaluation; a/c
Dx parenchymal lung disease, hypoxemia, or sleep disorder:
Medical treatment, oxygen, positive pressure breathing
as appropriate, and further evaluation for other
contributing causes, including RHC if necessary
no
What limitations are caused by
the PAH?
Functional class; 6-minute walk
test
What are the precise pulmonary
hemodynamics?
RHC
Document exercise capacity regardless of cause of PH:
Establish baseline, prognosis and document progression/
response to treatment with serial reassessments
Document PA and RA pressures, PCWP (LV or LA pressure
if PCWP unobtainable or uncertain), transpulmonary gradient
CO, PVR, SvO2, response to vasodilators:
Confirm PAH, or IPAH if no other cause identified
Discuss genetic testing and counseling of IPAH
McGoon et al. Chest 2004;126:14S-34S
NYHA Classification
Right Heart Catheterization is the
Diagnostic Gold Standard
•
Saturations
– Rule Out Shunts
• Intra-cardiac
• Intra-Pulmonary
•
Hemodynamics
– RAP
– mPAP
– PCWP
• Rule out left sided heart disease
– CO/CI
– PVR
•
Angiography
•
Vasodilator Response
– Vessel properties
– CTEPH
RHC can also Prognosticate!
Rich et al. WHO Symposium on PPH. Evian, France,1998.
Therapeutic Pathways
Therapies
• The only groups that have been approved for
the specialized medications for pulmonary
hypertension are Group 1 (pulmonary arterial
hypertension/PAH) and Group 4 (CTEPH)
• The other groups require treatment of the
underlying condition causing the elevated
pressures.
Therapeutic Options for PAH
Traditional therapies
• Supplemental O2
• Diuretics
• Oral vasodilators
– (CCB)
• Anticoagulants
– warfarin
• Inotropic agents
– Digitalis
FDA approved for PAH
• Prostanoids
–
–
–
–
Epoprostenol (flolan/veletri)
Treprostinil (IV/SQ/Inhaled)
Inhaled Iloprost
Oral treprostinil (Orenitram)
• ERA’s
– Bosentan
– Ambrisentan
– Macitentan
• PDE-5 Inhibitors
– Sildenafil
– Tadalafil
• Guanylate Cyclase Stimulator
– Riociguat
PAH Treatments ― a Historical
Overview
IV treprostinil
CCB, anticoagulation,
digitalis, diuretics
Riociguat
Macitentan
Orenitram
sildenafil
SC treprostinil
ambrisentan
epoprostenol
bosentan
Iloprost
veletri
<1995 1995 1996 1997 1998 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 2011 2012 2013
tadalafil
Inhaled treprostinil
Prostanoids
• Prostacyclin (PGI2)- member of the
eicosanoids family, inhibits platelet activation
and effective vasodilator.
• Prostacyclin released by healthy endothelial
cells.
• Deficiency in PAH patients
• Several routes of administration:
– IV/parenteral, SQ, Inhaled, oral
IV Prostanoids
• Epoprostenol- Flolan and Veletri
– Half-life approximately 2-5min
• Treprostinil- Remodulin
– Half-life several hours
– Both administered in ng/kg/min
– Dosing never changes even if weight does, start
weight remains the same throughout duration of
therapy.
Single Lumen
Hickman
Catheter
• Never stop
infusion
• Never draw
labs from line
• Never flush
CADD Legacy Pump
SQ Prostanoids
• Treprostinil
(Remodulin) SQ
– Small catheter placed
in SQ tissue of the
abdomen
– Site changed every 35 weeks
Inhaled Prostanoids
• Iloprost (Ventavis)
– 6-9 treatments per day
– Fewer systemic effects than IV
• Treprostinil (Tyvaso)
– QID and dosed as breaths
• e.g. 3 breaths each inhalation that is increased by
increments of 3 up to 9.
• Single person nebulizer
– Pt must bring in machine from home if hospitalized
Inhaled Prostanoids
Tyvaso
Ventavis
Oral Prostacyclin
• Treprostinil (Orinetram)
– Antiplatelet and vasodilatory actions, including
pulmonary vasodilation
– FREEDOM-M trial (only study of 3 that met
endpoint)
– Available as 0.125mg, 0.25mg, 1mg, 2.5mg ER BID
• Starting dose 0.25mg bid and titrated Q3d as tolerated
• Only showed improved 6MWD as monotherapy
Endothelin Receptor Antagonist
• Endothelian-1 (ET-1) levels are increased in PAH and
found in the precapillary pulmonary microvasculature
which is the site of the increased vascular resistance in
PAH.
– Two G protein-coupled receptors for ET-1 have been
described: “ETA” and “ETB”
• Bosentan- dual antagonist
– 62.5 to 125mg BID
• Ambrisentan- Selective ETA receptor
– 5-10mg daily
• Macitentan- Dual but with increased selectivity for ETA
– 10mg daily
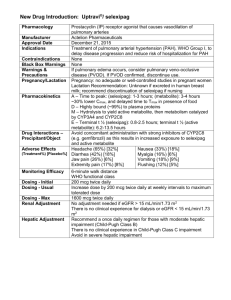
Phosphodiestrase-5 Inhibitors
• PDE5 Inhibitor- blocks the degradative action
of phosphodiesterdase type 5 on cyclic GMP
in smooth muscle cells resulting in
vasodilation of the vessels.
• Sildenafil- 20-80mg TID
• Tadalafil- 20-40mg daily
Guanylate Cyclase Stimulator
• Riociguat has a dual mode of action
– Synergist with endogenous nitric oxide
– Directly stimulating guanylate cyclase
independent of NO availability
• Phase 3 trial in the NEJM: 12 wk double-blind
randomized placebo-controlled trial at 124
centers in 30 countries for PAH patients
showed improved walk distance and
improvement in secondary end-points.
Cost per Year
•
•
•
•
•
Ambrisentan (Letairis)- $76,047.60
Bosentan (Tracleer)- $76,543.20
Tadalafil (Adcirca)- $18,316.80
Epoprostenol (Flolan)- $34,170
Oral Treprostinil (Orinetram)- $500,000
Triple therapy can be over $130, 000/yr just for
specialty medications.
Ongoing Management
• Standard of care is for PAH patients to be
established with a PH center for ongoing care.
– Multidisciplinary approach to care
• Patients on advance therapies to be seen
every 3 months if not more frequently
• Ongoing escalation of care, more evidence
coming out showing the importance of
combination therapies.
Questions?