100mg/dl - Aile.net

Hyperlipidemia
Saudi Diploma in Family Medicine
Center of Post Graduate Studies in Family Medicine
Presented by: Dr. Zekeriya Aktürk zekeriya.akturk@gmail.com
www.aile.net
1 / 29
Top 10 cause of Death in K.S.A.
Top 10 cause of Death in K.S.A.
30 %
• Cardiovascular diseases (CVD) are the main cause of morbidity and mortality among the Saudi population 1
• A significant proportion of hospital admissions is due to CVD, whether acute or chronic or to cardiac procedures including angiograms 2
1-Al Balla SR,. J Trop Med Hyg 1993;96:157-62
2-Bamgboye EA, Saudi Med J 1993;13(1):8-13. ] .
Prevalence of dyslipidemia in
Saudi Adults
• The overall prevalence of hypercholesterolemia
TC > 200 mg/ dL: 35.4% .
• The overall prevalence of hypertriglyceridemia
TG > 150 mg/ dL) : 49.6%.
• HDL Values in men and women
Men <40mg/dL: 74.8 %
Women <50mg/dL: 81.8
Al-Nozha MM.et al. Metabolic syndrome in Saudi Arabia. Saudi Med J 2005; 26 (12): 1918-1925
Hyperlipidemia
Michele Ritter, M.D.
Argy Resident – February, 2007
6 / 29
The story of lipids
• Chylomicrons transport fats from the intestinal mucosa to the liver
• In the liver, the chylomicrons release triglycerides and some cholesterol and become low-density lipoproteins (LDL).
• LDL then carries fat and cholesterol to the body’s cells.
• High-density lipoproteins (HDL) carry fat and cholesterol back to the liver for excretion.
7 / 29
The story of lipids (cont.)
• When oxidized LDL cholesterol gets high, atheroma formation in the walls of arteries occurs, which causes atherosclerosis.
• HDL cholesterol is able to go and remove cholesterol from the atheroma.
• Atherogenic cholesterol → LDL, VLDL,
IDL
8 / 29
Atherosclerosis
9 / 29
Causes of Hyperlipidemia
• Diet
• Hypothyroidism
• Nephrotic syndrome
• Anorexia nervosa
• Obstructive liver disease
• Obesity
• Diabetes mellitus
• Pregnancy
• Obstructive liver disease
• Acute heaptitis
• Systemic lupus erythematousus
• AIDS (protease inhibitors)
10 / 29
Dietary sources of Cholesterol
Type of Fat
Monounsaturated
Polyunsaturated
Saturated
Trans
Main Source
Olives, olive oil, canola oil, peanut oil, cashews, almonds, peanuts and most other nuts; avocados
Corn, soybean, safflower and cottonseed oil; fish
Effect on Cholesterol levels
Lowers LDL, Raises
HDL
Lowers LDL, Raises
HDL
Whole milk, butter, cheese, and ice cream; red meat; chocolate; coconuts, coconut milk, coconut oil , egg yolks, chicken skin
Raises both LDL and
HDL
Most margarines; vegetable shortening; partially hydrogenated vegetable oil; deepfried chips; many fast foods; most commercial baked goods
Raises LDL
11 / 29
Hereditary Causes of Hyperlipidemia
• Familial Hypercholesterolemia
• Codominant genetic disorder, coccurs in heterozygous form
• Occurs in 1 in 500 individuals
• Mutation in LDL receptor, resulting in elevated levels of LDL at birth and throughout life
• High risk for atherosclerosis, tendon xanthomas (75% of patients), tuberous xanthomas and xanthelasmas of eyes.
• Familial Combined Hyperlipidemia
• Autosomal dominant
• Increased secretions of VLDLs
• Dysbetalipoproteinemia
• Affects 1 in 10,000
• Results in apo E2, a binding-defective form of apoE (which usually plays important role in catabolism of chylomicron and VLDL)
• Increased risk for atherosclerosis, peripheral vascular disease
• Tuberous xanthomas, striae palmaris
12 / 29
Checking lipids
• Nonfasting lipid panel
• measures HDL and total cholesterol
• Fasting lipid panel
• Measures HDL, total cholesterol and triglycerides
• LDL cholesterol is calculated:
– LDL cholesterol = total cholesterol – (HDL + triglycerides/5)
13 / 29
When to check lipid panel
• Two different Recommendations
– Adult Treatment Panel (ATP III) of the National Cholesterol
Education Program (NCEP)
– Beginning at age 20: obtain a fasting (9 to 12 hour) serum lipid profile consisting of total cholesterol, LDL, HDL and triglycerides
– Repeat testing every 5 years for acceptable values
– United States Preventative Services Task Force
– Women aged 45 years and older, and men ages 35 years and older undergo screening with a total and HDL cholesterol every 5 years.
– If total cholesterol > 200 or HDL <40, then a fasting panel should be obtained
– Cholesterol screening should begin at 20 years in patients with a history of multiple cardiovascular risk factors, diabetes, or family history of either elevated cholesteral levels or premature cardiovascular disease.
14 / 29
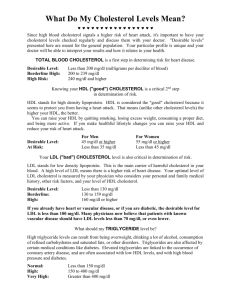
Goals for Lipids
• LDL
– < 100 →Optimal
– 100-129 → Near optimal
– 130-159 → Borderline
– 160-189→ High
– ≥ 190 → Very High
• Total Cholesterol
– < 200 → Desirable
– 200-239 → Borderline
– ≥240 → High
• HDL
– < 40 → Low
– ≥ 60 → High
• Serum Triglycerides
– < 150 → normal
– 150-199 → Borderline
– 200-499 → High
– ≥ 500 → Very High
15 / 29
Determining Cholesterol Goal
(LDL!)
• Look at JNC 7 Risk Factors
•
Cigarette smoking
•
Hypertension (BP ≥140/90 or on antihypertensives)
•
Low HDL cholesterol (< 40 mg/dL)
•
Family History of premature coronary heart disease (CHD) (CHD in first-degree male relative
<55 or CHD in first-degree female relative < 65)
•
Age (men ≥ 45, women ≥ 55)
16 / 29
Determining Goal LDL
• CHD and CHD Risk Equivalents:
– Peripheral Vascular Disease
– Cerebral Vascular Accident
– Diabetes Mellitus
17 / 29
LDL Goals
• 0-1 Risk Factors:
• LDL goal is 160
• If LDL ≥ 160: Initiate TLC (therapeutic lifestyle changes)
• If LDL ≥ 190: Initiate pharmaceutical treatment
• 2 + Risk Factors
• LDL goal is 130
• If LDL ≥ 130: Initiate TLC
• If LDL ≥ 160: Initiate pharmaceutical treatment
• CHD or CHD Risk Equivalent
• LDL goal is 100 (or 70)
• If LDL ≥ 100: Initiate TLC and pharmaceutical treatment
18 / 29
Treatment of Hyperlipidemia
• Lifestyle modification
– Low-cholesterol diet
– Exercise
19 / 29
Medications for Hyperlipidemia
Drug Class Agents
HMG CoA reductase inhibitors
Cholesterol absorption inhibitor
Lovastatin
Pravastatin
Ezetimibe
Nicotinic Acid
Fibric Acids Gemfibrozil
Fenofibrate
Bile Acid sequestrants Cholestyramine
Effects (% change)
LDL (18-55),
HDL (5-15)
Triglycerides (7-30)
LDL( 14-18),
HDL (1-3)
Triglyceride (2)
LDL (15-30),
HDL (15-35)
Triglyceride (20-50)
LDL (5-20),
HDL (10-20)
Triglyceride (20-50)
Side Effects
Myopathy, increased liver enzymes
Headache, GI distress
Flushing, Hyperglycemia,
Hyperuricemia, GI distress, hepatotoxicity
Dyspepsia, gallstones, myopathy
LDL
HDL
No change in triglycerides
GI distress, constipation, decreased absorption of other drugs
20 / 29
21 / 29
Case # 1
• A 55-year-old woman without symptoms of CAD seeks assessment and advice for routine health maintenance. Her blood pressure is 135/85 mm
Hg. She does not smoke or have diabetes and has been postmenopausal for 3 years. Her BMI is 24.
Lipoprotein analysis shows a total cholesterol level of 240 mg/dL, an HDL level of 55 mg/dL, a triglyceride level of 85 mg/dL and a LDL level is
180 mg/dL. The patient has no family history of premature CAD.
22 / 29
Case # 1 (cont.)
• What is the goal LDL in this woman?
• What would you do if exercise/diet change do not improve cholesterol after 3 months?
• How would your management change if she complained of claudication with walking?
23 / 29
Case # 2
• A 40- year-old man without significant past medical history comes in for a routine annual exam. He has no complaints but is worried because his father had a “heart attack” at the age of 45. He is a current smoker and has a 23-pack year history of tobacco use. A fasting lipid panel reveals a LDL 170 mg/dL and an HDL of 35 mg/dL. Serum Triglycerides were 140 mg/dL.
Serum chemistries including liver panel are all normal.
24 / 29
Case # 2 (cont.)
• What is this patient’s goal LDL?
• Would you start medication, and if so, what?
25 / 29
Case # 3
• A 65 year-old woman with medical history of
Type II diabetes, obesity, and hypertension comes to your office for the first time. She has been told her cholesterol was elevated in the past and states that she has been following a “low cholesterol diet” for the past 6 months after seeing a dietician.
She had a normal exercise stress test last year prior to knee replacement surgery and has never had symptoms of CHD. A fasting lipid profile was performed and revealed a LDL 130, HDL 30 and a total triglyceride of 300. Her Hgba1c is 6.5%.
26 / 29
Case # 3 (cont.)
• What is this patient’s goal LDL?
• What medication would you consider starting in this patient?
• What labs would you want to monitor in this patient?
27 / 29
HYPERLIPIDEMIA
Brian V. Reamy, MD, Colonel, USAF, MC
Chair – Department of Family Medicine
Uniformed Services University
28 / 29
Why Bother?
• Optimum treatment of lipids helps in the primary & secondary prevention of
ASCVD; still our nation’s #1 killer
29 / 29
Why Bother?
• ASCVD has been #1 cause of death every year since 1900 with exception of 1918.
• 50% of CVD diagnoses and 15% of CVD deaths are in patients < 65 years of age
• Many young adults have 2 or more risk factors that go unrecognized and untreated.
•
HUGE opportunity to prevent disease!!
30 / 29
NCEP/ATP III – 15 May 2001
• www.nhlbi.nih.gov
•
LDL goals lowered
•
Raised acceptable HDL to 40
•
Lowered TG goal to 150
•
Risk Factor assessment enhanced with the 10-yr Framingham risk calculator
•
Added the Metabolic Syndrome to Tx
31 / 29
NCEP/ATP III – 9 Steps
• Step 1: Obtain, complete & fasting lipids.
• Interpret: LDL < 100mg/dl optimal
LDL 100-129 near optimal
LDL 130-159 borderline high
LDL 160-189 high
LDL >190 very high
( mg/dl x 0.0259mmol/l = SI units)
32 / 29
NCEP/ATP III
• Step 2: Identify if patient has CAD or equivalent (PAD, DM, AAA, Carotid)
• Step 3:
Risk factor assessment (HTN, FHx,
Tob, Age & Sex, HDL<40 or >60)
• Step 4: If 2 or more risk factors; do
Framingham 10-yr risk assessment.
33 / 29
Framingham
Ten
Year Risk
Men Women
34 / 29
0
Framingham Ten Year Risk
35 / 29
0
3
0
Framingham Ten Year Risk
Non-Smoker
36 / 29
0
3
0
1
Framingham Ten Year Risk
HDL = 43
37 / 29
0
3
0
1
0
4
Framingham Ten Year Risk
SBP = 119, untreated
38 / 29
0
3
0
1
0
4
Framingham Ten Year Risk
39 / 29
NCEP/ATP III – Step 5
Risk
Category
LDL Goal Start
T.L.C.
Start Drug
Treatment
CHD/10yr risk>20%
<100mg/dl >100mg/dl >100 –
129mg/dl
(high)
2+RF or
10yr<20%
(Medium)
<130mg/dl >130mg/dl >130 –
160mg/dl
0-1 risk factors (low)
<160mg/dl >160mg/dl >160 –
40 / 29 190mg/dl
NCEP/ATP III – Step 6
• Initiate Therapeutic Lifestyle Changes
(TLC)
– AHA Step 2 diet
– Soluble fiber 10-25gm/day
– Plant sterols/Sitostanol (Benecol®, Take
Control® margarines) - lower LDL 10%
– Increased exercise
– Weight management
41 / 29
NCEP/ATP III – Step 7
• Add drug therapy simultaneously to TLC in patients with CHD or equivalent. Add drugs after
3 months if TLC not effective in other risk categories.
• Best unbiased source for review of drug treatment:
“The Medical Letter: Choice of lipid regulating drugs” 43:2001,pp43-48 and 2003;1;77-79.
42 / 29
Drugs – Step 7 (cont.)
• Resins - (cholestyramine,colestid, colesevelam): lower LDL; adjunct to statins; GI side effects/malabsorption issues
• Niacin“miracle agent”, cheap & moves every parameter in the right direction. But, side effects problematic. NIASPAN® easier to tolerate. Need slow dose titration and pre-med with ASA.
Caution with Diabetes; can worsen glycemic control if HBA1C >7.5 at baseline. Most potent agent at increasing HDL.
43 / 29
Drugs – Step 7 (cont)
•
Fibrates
– (fenofibrate, gemfibrozil) lower
TG and raise HDL. Can combine with statins but caution re: hepatic side effects.
Cutting statin dose by ½ is good rule.
*Fenofibrate qd & less side effects, >$$
• If combining w/ a statin use fenofibrate; gemfibrozil has > rates of rhabdomyolysis
44 / 29
Newer Drugs – Step 7 (cont.)
•
Ezetimibe (Zetia®)new class that inhibits the intestinal absorption of cholesterol.
Lowers LDL 17%, TG 6%, increases HDL by 1.3%. Combined with a statin increases effects of statin by 10-15% w/o side effects.
VERY well tolerated at 10mg/d.
45 / 29
Newer Drugs – Step 7 (cont)
•
Lovastatin + Niacin (Advicor®)in fixed combos 20/500, 20/750, 20/1000. Increase dose monthly up to max 40/2000. Max dose w/ LDL decrease 45%, TG 42%, and HDL increase by 41%. Causes less flushing and hepatic effects than any niacin formulation.
Greater risk of myopathy than a statin alone.
46 / 29
Newer Drugs – Step 7
• Simvastatin(10/20/40/80) + Ezetimibe
10mg: VYTORIN®
• OMACOR: concentrated omega-3’s; 4 capsules = 12 OTC fish oil capsules
• Can interfere with clotting times; caution in folks on warfarin
47 / 29
Drugs – Step 7 (cont.)
• StatinsAll w/ anti-inflammatory effects. None safe in pregnancy. All are more potent by 10-15% with evening dosing.
- muscle pain = 1-5%
- hepatitis (transaminases>3x nl.) = 0.5%
- rhabdomyolysis = rare; incidence rates per million Rx’s
: pravastatin0.04, lovastatin0.19
atorvastatin 0.04, simvastatin 0.12.
( cerivistatin was 16-80x these rates!!)
48 / 29
Drugs – Step 7 (cont.)
• Atorvastatin – great LDL & TG lowering
• Lovastatin: take w/ food; generic version
• Pravastatin: least drug interactions due to different elimination pathway; take on empty stomach
• Simvastatin: lots of prevention data, potent
• Fluvastatin: less potent; poor prevention data
• Rosuvastatin: most potent; 5 - 40 mg
(CRESTOR®); may raise HDL a bit more & lower TG. Caution w/ CrCl<30cc/min and in
Asian subpopulations at higher doses.
49 / 29
Statin Pearls
• Elevated transaminases on statins; (unless reaching 3x normal), are not a reason to stop the statin – they are are a reason to watch closely.
• Statin side effects are often agent specific, not always class specific.
• Unexplained myalgias may occur on statins without CK elevation. Try a different statin.
50 / 29
Statin Pearls
• Rhabdomyolysis is uncommon unless CK is elevated to 10 x normal. Usually occurs in patients with multiple co-morbidities.
• Unless you enjoy driving yourself nuts; do not check CK serially in patients on statins.
Remember vigorous yard work will bump your
CK! Some think a baseline CK may be helpful.
• But – what about the PROVE-IT study? (NEJM 8
April 2004)
51 / 29
PROVE-IT Trial
• Designed to “PROVE” that 80mg atorvastatin was no better than 40 mg pravastatin in secondary prevention.
• But, atorvastatin was superior as early as 30 days of therapy . In just 24 mths the atorvastatin group (meanLDL=62) had 16% less of all CV events. 28% less mortality than pravastatin group (meanLDL=95)
52 / 29
PROVE-IT Trial
• WOW!
• Evidence from mammalian species had shown that atherogenesis stops & reverses at an LDL <80 – now some clinical outcome data.
53 / 29
NCEP Update 13 July 2004
• Circulation 13 July 2004:227-239
• Added the results of PROVE-IT, HPS, PROSPER,
ALLHAT, ASCOT
• Confirmed ATP-III and added that in very high risk an LDL goal <70 was optional
• For patients at moderately high risk = 10-20%
Framingham risk; LDL <100 new goal
• Felt that drug treatment should aim for at least a
30-40% LDL reduction.
54 / 29
Updated ATP-III Guidelines
RISK LDL TLC DRUGS
HIGH
>20% 10yr
Mod. High
10-20%
Moderate
<10% 10yr
LOW
<70mg/dl
Optional
< 100mg/dl
Optional
>
>
100mg/dl
130mg/dl
> or <100mg
>
100mg/dl
130mg/dl or 100-130
<130mg/dl >130mg/dl >160mg/dl
<160mg/dl >160mg/dl >190mg/dl
55 / 29
TNT Study
“Treat to New Targets”
• NEJM 7 April 2005: Prospective trial at lowering LDL well below 100mg/dl in adults with CHD (secondary prevention)
• 10,001 patients; 2 groups for 4.9 years with mean LDL = 99mg/dl before study
– 10 mg atorvastatin (mean LDL=101mg/dl)
– 80 mg atorvastain (mean LDL=77mg/dl)
56 / 29
TNT - Results
• Side Effects: increased LFT’s in 0.2% of patients on low dose and 1.2% on high dose. No change in rhabdomyolysis risk.
• Results: Relative risk reduction of 22% and absolute risk reduction of 2.2% in major cardiovascular events for group with LDL
<80 versus group with LDL=101.
• More evidence to lower our LDL goals…
57 / 29
NCEP/ATP III – Step 8
• Identify Metabolic Syndrome: (3 of 5)
– SBP>130, FBS>110, TG>150, HDL<40 in men and <50 in women, waist>40”men, 35”women
Aggressively:
– Treat underlying causes of overweight and physical inactivity.
– Treat HTN, use ASA for CHD patients
58 / 29
NCEP/ATP III – Step 9
• Treat elevated TG (>150mg/dl)
– First lower LDL; if TG still >200 consider adding/increasing drug therapy
– But, if TG >500mg/dl, first lower triglycerides to prevent pancreatitis. When they are <500 then return to LDL lowering
– Treat HDL <40 after lowering LDL.
59 / 29
CASES
• All real cases. No “perfect answers”.
• All present real Family Practice dilemmas.
• Will use the evidence to help formulate a
“best” answer.
• Use cases to convey cutting edge info.
60 / 29
Case # 4 – “Middle-of the Road”
• 45 year old woman who on a routine lipid screen has the following values:
• TC = 203 HDL=48 TG = 155 LDL = 124
• PMHx: negative, smoker
• Meds: daily vitamin
• FHx: MI in F age 60, M age 64
• PE: 65” 130lbs P=72 BP=118/68
61 / 29
Case #4 – “Middle of the Road”
• Risk Factors: 2 ; Framingham = 5% risk
• NCEP/ATP III says that she is at her LDL goal; e.g. <130
• But, concerns remain: FHx, Smoking, HDL is <50 & TG >150; both less than ideal.
• What do you do with this “middle-of-theroad” risk profile?
62 / 29
Case# 4 – Middle of the Road
• Consider a new idea: measure her hs-CRP
• Facts: CRP is a marker of inflammation.
• ASCVD is a disease of inflammation
• Multiple prospective epidemiological (vs. interventional studies) have shown that CRP can predict MI,CVA, PAD, sudden cardiac death.
63 / 29
Case #4 – Middle of the Road
• Hs-CRP assays are now widely available; can check non-fasting, anytime of day.
• < 1mg/l = low risk
• 1-3mg/l = moderate risk
• >3mg/l = high risk
•
>10mg/l = invalid for cardiac risk prediction;consider 1° inflammatory disease, trauma, serious infection.
64 / 29
Case #4 – Middle of the Road
• PRINCE (PRavastatin INflammation/Crp
Evaluation trial; JAMA 2001:286;64-70.
And other trials have proven that Statins lower CRP 15-25% within 6 weeks of initiation.
• Weight loss, exercise and smoking cessation also lower CRP.
65 / 29
Case # 4 – Middle of the Road
• CARE & AFCAPS/TEXCAPS both suggest that the benefit of statin therapy among those with low
LDL but high CRP may be as large as those with overt hyperlipidemia.
• How to answer this ?
• 2003: 15,000 patients with LDL<130 but CRP above 2.0mg/l (JUPITER). All will be put on
CRESTOR® for prevention. What will happen?
66 / 29
Case # 4 – Middle of the Road
• What does this mean for our patient?
• CRP is most useful in those judged at intermediate risk and in primary prevention.
• Review; 45 yr old woman with an
LDL<130 but +FHX and other borderline risks…eg a 5% Framingham risk
• HOW about checking an hs-CRP to further assess her risk ?
67 / 29
Case # 4 – Middle of the Road
• CRP = 3.2mg/l HIGH risk
• Studies have proven she is in fact at risk; more than her LDL would tell us. What to do?
• Smoking cessation will lower CRP
• Statins will lower her CRP
• But, no prospective proof that this will change her outcome. It is your call, Doctor!
68 / 29
Other Novel Risk Factors
• EBCT (coronary Ca++ score)
• Lp (a) lipoprotein, Apo B, LDL particle size
• Homocysteine
• Plasma Adiponectin
69 / 29
EBCT/Coronary Ca++ scores
• Coronary Ca++ occurs due to ASCVD
• Normal score=0-10; 11-100 = mild disease, 101-
400 = non-obstructive disease, >400 = obstructive
• Significant false positives and poor data in women and younger patients
• It may not provide incremental information above that obtained with conventional risk factor assessment; it is an alternative.
70 / 29
EBCT
• Like with hs-CRP, it is not very useful in low risk or very high risk patients. It significantly correlates w/ cheaper hs-CRP.
• Best used in intermediate risk folks where it might change treatment approach.
• In patients w/ intermediate risk an EBCT score >80 has a sensitivity of 85% and a specificity of 75% for the risk of events.
71 / 29
EBCT/Coronary Ca++ Scores
• USPSTF: Feb 2004; “D” recommendation for adults at low risk. “absence of evidence that detection ultimately results in improved health outcomes, and because false positive tests are likely to cause harm…”
• “I” recommendation for those at high risk
72 / 29
Homocysteine
• High plasma homocysteine may be directly related to atherosclerosis development.
• Homocysteine may enhance inflammation
& thrombosis.
• There may be no causal association between elevated homocysteine and CV disease risk.
• New Evidence!!
73 / 29
Homocysteine
• NEJM; 13 April 2006; 2 studies re: homocysteine lowering
• #1: Secondary prevention: 5522 patients: placebo vs 2,5mg Folate+B6+B12: did not reduce the risk of cardiovascular event, more pts in Tx had unstable angina.
• #2: 3749 pts post-MI: “treatment with Bvitamins did not lower risk of recurrent CV disease. A harmful effect of B-vitamin Tx was suggested.”
74 / 29
Lipid Sub-fractions & other markers
• Lipoprotein a, Apolipoprotein B, LDL particle size
– All have predictive value for CHD, indeed LDL particle size is more precise than LDL alone.
But not widely available, expensive, less reproducible and still no outcome studies.
75 / 29
Case # 5 – The Unreachable Goal
• 60 yr old male returns to see you 3 months after a
4vCABG. He feels great. At his last visit with his
CT surgeon he was told; “follow-up with your family doctor to get your cholesterol in control”
• PMHX: HTN x 20 yrs, BPH, ED, mild OA
• MEDS: ASA, Metoprolol 50 mg po bid, Viagra®,
Simvastatin 20 mg po qd
• FHX: F with CVA at 68
76 / 29
Case # 5 – The Unreachable Goal
• PE: 70” 160lbs P=60 BP=124/76
• Cor: RRR, no m/r/g, no jvd, healed median sternotomy scar
• Ext: no edema
Lungs: slight dec. breath sounds
• TC=180, HDL=42 TG=100 LDL=118
77 / 29
Case # 5 – The Unreachable Goal
• Risk Assessment = he has CHD; 2° prev.
• Goal LDL is <100 per ATP III (<70-80 TNT trial data and ATP update)
• At this level atherogenesis seems to arrest
• At an LDL of 80 in mammalian species atherogenesis reverses. Also the PROVE-IT trial shows that an LDL of 62 was superior to an LDL of 95.
78 / 29
Case #5 – The Unreachable Goal
• You decide to increase the simvastatin to
40mg po qd.
• 6 weeks later; TC= 170 TG=105 HDL=42
LDL=107
• What do you do?
79 / 29
Case # 5 – The Unreachable Goal
• Many options: 1)increase simvastatin to 80 mg or change to atorvastatin or rosuvastatin.
• PROBLEM: inc risk of side effects and less
LDL lowering effect as you inc statin doses.
For every doubling of dose, LDL decreases by only 6 %. A threefold higher dose by
12% and a fourfold increase lowers LDL cholesterol by only 18%.
80 / 29
Case # 5 – The Unreachable Goal
• 2.) Add Ezetimibe 10 mg po qd: less chance of side effects; should help to reach goal
LDL easily.
• 3.) Intensify diet; Ornish Plan; add soluble fiber, add soy, add omega-3 fatty acids.
• 4.) Be satisfied and await more trials…
81 / 29
Summary
•
8 Points to make you strong
• 1) 1° & 2° prevention of
ASCVD are possible!
2) NCEP/ATP III at www.nhlbi.nih.gov
is useful.
3) The key step is risk assessment & then tailoring treatment to individual risk.
82 / 29
Summary – 8 Points
• 3) Better medication options are a help:
Ezetimibe, Advicor®, new statins and a cleaner understanding of statin side effects
• 4)Attack the metabolic syndrome!! A multi-modal treatment plan is best.
• 5) Don’t ignore a chance for prevention because your patient is >70 or <35.
83 / 29
Summary – 8 Points
• 6) hs-CRP is a powerful new tool to predict risk; especially in those at intermediate risk.
But, we need prospective proof that lowering it will help reduce ASCVD endpoints.
7) Try to get to goal; anticipate new ATP-IV guidelines.
84 / 29
Thanks for your Attention!
85 / 29