Hypercholesterolemia and Risk Stratifcation of Cardiovascular
advertisement
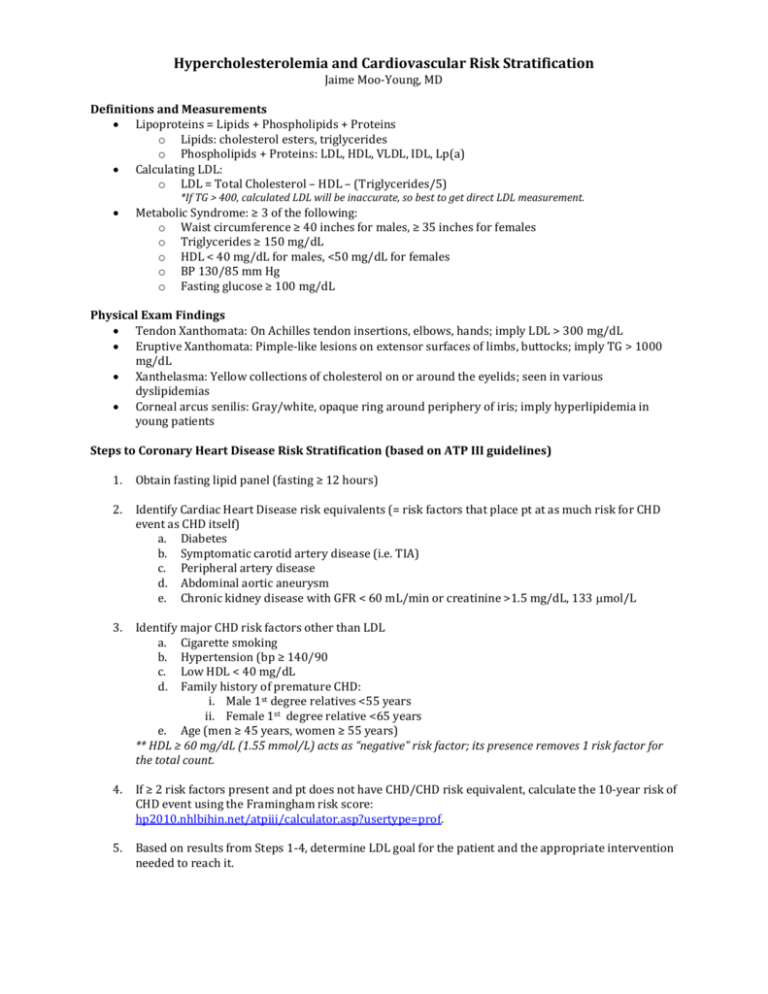
Hypercholesterolemia and Cardiovascular Risk Stratification Jaime Moo-Young, MD Definitions and Measurements Lipoproteins = Lipids + Phospholipids + Proteins o Lipids: cholesterol esters, triglycerides o Phospholipids + Proteins: LDL, HDL, VLDL, IDL, Lp(a) Calculating LDL: o LDL = Total Cholesterol – HDL – (Triglycerides/5) *If TG > 400, calculated LDL will be inaccurate, so best to get direct LDL measurement. Metabolic Syndrome: ≥ 3 of the following: o Waist circumference ≥ 40 inches for males, ≥ 35 inches for females o Triglycerides ≥ 150 mg/dL o HDL < 40 mg/dL for males, <50 mg/dL for females o BP 130/85 mm Hg o Fasting glucose ≥ 100 mg/dL Physical Exam Findings Tendon Xanthomata: On Achilles tendon insertions, elbows, hands; imply LDL > 300 mg/dL Eruptive Xanthomata: Pimple-like lesions on extensor surfaces of limbs, buttocks; imply TG > 1000 mg/dL Xanthelasma: Yellow collections of cholesterol on or around the eyelids; seen in various dyslipidemias Corneal arcus senilis: Gray/white, opaque ring around periphery of iris; imply hyperlipidemia in young patients Steps to Coronary Heart Disease Risk Stratification (based on ATP III guidelines) 1. Obtain fasting lipid panel (fasting ≥ 12 hours) 2. Identify Cardiac Heart Disease risk equivalents (= risk factors that place pt at as much risk for CHD event as CHD itself) a. Diabetes b. Symptomatic carotid artery disease (i.e. TIA) c. Peripheral artery disease d. Abdominal aortic aneurysm e. Chronic kidney disease with GFR < 60 mL/min or creatinine >1.5 mg/dL, 133 mol/L 3. Identify major CHD risk factors other than LDL a. Cigarette smoking b. Hypertension (bp ≥ 140/90 c. Low HDL < 40 mg/dL d. Family history of premature CHD: i. Male 1st degree relatives <55 years ii. Female 1st degree relative <65 years e. Age (men ≥ 45 years, women ≥ 55 years) ** HDL ≥ 60 mg/dL (1.55 mmol/L) acts as “negative” risk factor; its presence removes 1 risk factor for the total count. 4. If ≥ 2 risk factors present and pt does not have CHD/CHD risk equivalent, calculate the 10-year risk of CHD event using the Framingham risk score: hp2010.nhlbihin.net/atpiii/calculator.asp?usertype=prof. 5. Based on results from Steps 1-4, determine LDL goal for the patient and the appropriate intervention needed to reach it. LDL LEVEL AT WHICH RISK CATEGORY RISK PROFILE COMPONENTS High ≥1 CHD Equivalent or ≥ 2 Risk Factors + 10-yr risk >20% < 100 mg/dL < 70 if very high risk (ACS; CHD + met synd) ≥ 100 mg/dL ≥ 70 if v. high risk ≥ 130 mg/dL ≥ 100 if v. high risk Moderate High ≥ 2 Risk Factors + 10-yr risk 10-20% < 130 mg/dL ≥ 130 mg/dL > 130 mg/dL Moderate ≥ 2 Risk Factors + 10-yr risk < 10 % < 130 mg/dL ≥ 130 mg/dL ≥ 160 mg/dL Low 0-1 Risk Factors < 160 mg/dL ≥ 160 mg/dL ≥ 190 mg/dL LDL GOAL TO INITIATE LIFESTYLE CHANGES LDL LEVEL AT WHICH TO INITIATE MEDICAL THERAPY Lipid-lowering Therapy General Principles o For every 39 mg/dL (1 mmol) decrease in LDL 21% decrease in risk of major cardiovascular events o Also reasonable to target TG <400 and HDL > 40, though less clinical data available. Statins o Most potent drugs for lowering LDL (20-60%). Also lower TGs (10-25%) o Mechanism of action: HMG-CoA reductase inhibitorinhibits cholesterol synthesis by liver o Side effects: elevated transaminases, myalgias (+/- CK elevation), myositis, rhabdomyolysis o Rosuvatatin, Atorvastatin the most potent. o Pravastatin has most benign side effect profile. Ezetimibe o Used as adjuct to statins in order to lower LDL at a lower statin dose, but no data to show it improves morbidity/mortality o Mechanism of action: Inhibits cholesterol absorption at intestinal brush border o Side effects: steatorrhea, myalgias, transaminitis Fibrates (ex: fenofibrate, gemfibrozil) o Lower TGs, raise HDL . Mostly used for hypertriglyceridemia o Mechanisms of action: Upregulate fatty acid metabolism; decrease hepatic TG synthesis o Side effects: myopathy, especially if used w statin; gallstones, GI upset Niacin o Raises HDL; also lowers LDL at doses > 1.5-2.0 grams/day o Mechanisms of action: inhibits fatty acid release from adipose tissue; inhibits hepatic synthesis of fatty acids and TGs o Side effects: flushing, nausea, pruritus, gout flare, hyperglycemia, hepatic failure (rare) o Flushing mitigated by aspirin and extended-release forms of niacin Bile Acid Sequestrants (ex: cholestyramine) o Lowers LDL moderately. Used alone in pts with contraindication to statin, but also in addition to statin in pts with very high LDL. o Mechanism of action: Bind to bile acids in intestine more bile acid excretion in stool liver makes more bile acids to replace those lost in stool more cholesterol converted into bile acidsless cholesterol in blood o Side effects: bloating, diarrhea, abdominal pain Omega-3 Fatty Acids (fish oil, canola oil) o Lowers triglycerides o Mechanism of action: anti-inflammatory properties may contribute to decreased atherosclerosis formation o Side effects: dyspepsia, diarrhea, prolonged bleeding time References: 1. National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106:3143. 2. www.uptodate.com 3. Sabatine et al. Pocket Medicine, Fourth Edition. Wolters Kluwer, Lippincott Williams & Wilkins, 2010.