Dyslipidemia
advertisement

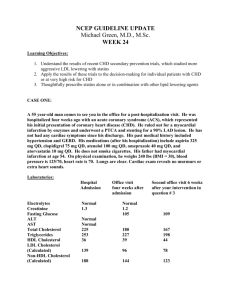
Dyslipidemia: What Every Resident Should Know Med Study • Lipoproteins – Chylomicrons, VLDL, IDL, LDL, & HDL • Hyperlipoproteinemia – Familial syndromes • Evaluation of hyperlipidemia • Treatment of hyperlipidemia – Guidelines, diet, & drugs MKSAP • Physiology & metabolism • Diagnosis – Secondary causes • Management – Increased LDL – Increased triglycerides – Decreased HDL Pathways of Lipid Transport Knopp, R. H. N Engl J Med 1999;341:498-511 Primary Lipoprotein Disorders Amenable to Treatment with Diet and Drug Therapy Knopp, R. H. N Engl J Med 1999;341:498-511 Pathophysiologic Events Culminating in the Clinical Syndrome of Unstable Angina Yeghiazarians, Y. et al. N Engl J Med 2000;342:101-114 JAMA 2001; 285: 2486-2497 NCEP Reports • ATP I (1988) – Prevention of CHD among patients with high LDL (160) or borderline high LDL (130-159) with multiple (2) risk factors • ATP II (1994) – Intensive management of LDL (100) among patients with established CHD • ATP III (2001) – Prevention of CHD among high-risk patients • DM as a CHD risk equivalent • Use of Framingham risk score • Therapeutic lifestyle changes NCEP - ATP III JAMA 2001; 285: 2486-2497 Question #1 • How often should the average adult patient have his or her lipids measured? Routine Testing • Adults ≥ 20 yo should have a fasting lipid panel measured every 5 years • If the specimen is non-fasting, then only the TC and HDL values can be used – Obtain a fasting lipid panel if… • TC ≥ 200 mg/dl, or • HDL ≤ 40 mg/dl JAMA 2001; 285: 2486-2497 Question #2 • What is the formula for calculating LDL from total cholestrol (TC), HDL, & triglycerides (TG)? Calculation of LDL • LDL = TC – [HDL + (TG 5)] – TC = HDL + LDL + VLDL – (TG 5) is an estimate of VLDL • Formula is not reliable if TG > 400 mg/dl Question #3 • What are 5 potential causes of “secondary dyslipidemia” that should be ruled out before to initiating lipid-lowering therapy? Secondary Dyslipidemia • • • • • Diabetes mellitus Hypothyroidism Obstructive liver disease Chronic renal failure Drugs – Anabolic steroids, corticosteroids, progestins, thiazides, protease inhibitors, Cyclosporine, Sertraline (Zoloft), Isotretinoin (Accutane) JAMA 2001; 285: 2486-2497 Secondary Dyslipidemia • Increased LDL – – – – – – Obesity Hypothyroidism Nephrotic syndrome Biliary cirrhosis Thiazide diuretics Pregnancy • Increased triglycerides – – – – – – – – Obesity Diabetes Hypothyroidism Chronic kidney disease Alcohol Thiazide diuretics Corticosteroids Nonselective blockers – Estrogen – Pregnancy MKSAP 13 Question #4 • According to ATP III, what are the 3 categories of risk that modify LDL goals? Categories of Risk • CHD and CHD risk equivalents • Multiple (2+) risk factors • Few (0-1) risk factors Question #5 • According to ATP III, which conditions are considered to be CHD risk equivalents? CHD Risk Equivalents • Other forms of atherosclerotic disease – Peripheral arterial disease – Abdominal aortic aneurysm – Symptomatic carotid artery disease • Diabetes mellitus • Multiple risk factors that confer a 10-year risk for CHD >20% – Framingham point score Question #6 • According to ATP III, what are the 5 major CVD risk factors that modify LDL goals? Major Risk Factors • Age – Men 45 yo – Women 55 yo • Family history of premature CHD – Males < 55 yo – Females < 65 yo • Cigarette smoking • Hypertension (>140/90 mmHg or on meds) • Low HDL (< 40 mg/dl) Question #7 • For which of the following patients should you calculate a Framingham point score in order guide your lipid-lowering therapy? – – – – A 50 yo man with CHD A 60 yo woman with diabetes mellitus A 50 yo man who smokes cigarettes A 60 yo woman without any other risk factors Multiple Risk Factors • Patients with 2 risk factors • Framingham point score • Ten-year risk for CHD – > 20% – 10-20% – < 10% Question #8 • According to ATP III, what is the LDL goal for each of the 3 categories of risk? – CHD or CHD risk equivalent – Multiple (2+) risk factors – Few (0-1) risk factors LDL Goals JAMA 2001; 285: 2486-2497 LDL Goals • Diabetes mellitus – LDL < 100 – ADA Guidelines (2005) • Chronic kidney disease – LDL < 100 – KDOQI Guidelines (2003) Question #8 • According to ATP III, what are the LDL cutpoints for initiating therapeutic lifestyle changes and drug therapy for each category of risk? – CHD or CHD risk equivalent – Multiple (2+) risk factors – Few (0-1) risk factors LDL Cutpoints JAMA 2001; 285: 2486-2497 Question #10 • According to ATP III, which therapeutic lifestyle changes (TLC) should physicians recommend to patients with dyslipidemia? Therapeutic Lifestyle Changes • Low-fat diet – Refer to a nutritionist – www.nutrition.gov • Increased physical activity – www.fitness.gov • Weight reduction – www.nhlbi.nih.gov/health/public/heart/obesity/l ose_wt/index.htm JAMA 2001; 285: 2486-2497 Model of Steps in Therapeutic Lifestyle Changes (TLC) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults, JAMA 2001;285:2486-2497. Copyright restrictions may apply. Question #11 • Which of the following classes of drugs can lower LDL the most? – – – – Bile acid sequestrants Fibric acids Nicotinic acid Statins (HMG CoA reductase inhibitors) LDL Lowering-Drugs • Statins 18-55% – Atorvastatin (Lipitor) & Simvastatin (Zocor) • Bile acid sequestrants 15-30% – Cholestyramine (Questran) & Colestipol (Colestid) • Nicotinic acid 5-25% – Niacin ER (Niaspan) • Fibic acid 5-20% – Fenofibrate (Tricor) & Gemfibrozil (Lopid) Characteristics of Statins Knopp, R. H. N Engl J Med 1999;341:498-511 Circulation 2004; 110: 227-239 Progression of Drug Therapy in Primary Prevention Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults, JAMA 2001;285:2486-2497. Copyright restrictions may apply. Circulation 2004; 110: 227-239 Recent Clinical Trials • HPS – Lancet 2002; 360: 7-22 • PROSPER – Lancet 2002; 360: 1623-1630 • ALLHAT-LLT – JAMA 2002; 288: 2998-3007 • ASCOT-LLA – Lancet 2003; 361: 1149-1158 • PROVE IT – TIMI 22 – N Engl J Med 2004; 350: 1495-1504 Heart Protection Study • 20,536 adults age 40-80 yo with CHD, PAD, or diabetes mellitus • Simvastatin (Zocor) 40 mg qd v placebo • Follow-up = 5 years • LDL 132.6 to 89.7 mg/dl • Primary outcomes – All-cause mortality – Vascular mortality – CHD mortality RR 13% (12.9% v 14.7%) RR 17% (7.6% v 9.1%) RR 18% (5.7% v 6.9%) Lancet 2002; 360: 7-22 Prospective Study of Pravastatin in the Elderly at Risk • • • • • 5,804 adults age 70-82 yo with, or at risk of, CVD Pravastatin (Pravachol) 40 mg qd v placebo Follow-up = 3.2 years LDL 148.2 to 97.8 mg/dl Primary outcome – Composite of CHD death, non-fatal MI, and fatal or nonfatal stroke – RR 15% (14.1% v 16.2%) Lancet 2002; 360: 1623-1630 Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial – Lipid-Lowering Trial • 10,355 adults ≥ 55 yo with HTN and ≥ 1 other CHD risk factor • Pravastatin (Pravachol) 40mg qd v placebo • Follow-up = 4.8 years • LDL 145.6 to 104 mg/dl • No difference in the primary outcomes – All-cause mortality – CVD death • CHD events and stroke 9% (stat. nonsignif.) JAMA 2002; 288: 2998-3007 Anglo-Scandinavian Cardiac Outcomes Trial – Lipid-Lowering Arm • • • • • 10,305 adults aged 40-79 yo with HTN Atorvastatin 10mg po qd v placebo Follow-up = 3.3 years LDL 132.6 to 90.5 mg/dl Primary outcome – Composite of fatal CHD and nonfatal MI – RR 36% (6% v 9.4%) Lancet 2003; 361: 1149-1158 Pravastatin or Atorvastatin Evaluation and Infection Therapy • 4,162 adults ≥ 18 yo hospitalized for ACS • Atorvastatin (Lipitor) 80mg qd v Pravastatin (Pravachol) 40 mg qd • Follow-up = 2 years • LDL values – Atorvastatin – Pravastatin 106 to 62 mg/dl 106 to 95 mg/dl • Primary outcome – Composite of all-cause mortality, MI, unstable angina, revascularization, and stroke – RR 16% (22.4% v 26.3%) N Engl J Med 2004; 350: 1495-1504 Circulation 2004; 110: 227-239 Lancet 2005; 366: 1267-1278 CTT (2005) • 14 RCTs of statins published 1994-2004 • 90,056 subjects – 55% had HTN – 47% had CHD – 21% had DM • Mean follow-up = 4.7 years • Mean baseline LDL = 147.8 mg/dl • Mean decrease in LDL after 1 yr = 42.5 mg/dl Lancet 2005; 366: 1267-1278 CTT (2005) CTT (2005) • Risk reduction per 1 mmol/L (39 mg/dl) decrease in LDL cholesterol: – – – – – – All-cause mortality CHD death Major coronary events Coronary revascularization Ischemic stroke Major vascular events 12% 19% 23% 24% 19% 21% • No significant increase in the risk of cancer or rhabdomyolysis Lancet 2005; 366: 1267-1278 Question #12 • What is the incidence of elevated liver transaminase levels with statin use? Hepatotoxicity • PROSPER: ALT & AST > 3X ULN – Pravastatin 0.0003% v placebo 0.0003% • HPS: ALT > 2X ULN – Simvastatin 1.8% v placebo 1.6% • PROVE IT: ALT > 3X ULN – Atorvastatin 3.3% v Pravastatin 1.1% Question #13 • What is the incidence of skeletal muscle toxicity with statin use? – Myalgias – Elevated creatinine kinase (CK) – Rhabdomyolysis Myotoxicity • Myalgias – PROSPER: Prava. 0.01% v placebo 0.01% – PROVE IT: Atorva. 3.3% v Prava. 1.1% • Elevated CK > 4X ULN – HPS: Simva. 0.30% v placebo 0.19% • Elevated CK > 10X ULN – PROSPER: Prava. 0% v placebo 0% • Rhabdomyolysis – HPS: Simva. 0.05% v placebo 0.03% – PROSPER: Prava. 0% v placebo 0% – PROVE IT: Atorva. 0% v Prava. 0% Question #14 • According to ATP III, what are the five clinical features of the metabolic syndrome? JAMA 2001; 285: 2486-2497 Question #13 • Which of the following classes of drugs can lower triglycerides (TG) the most? – – – – Bile acid sequestrants Fibric acids Nicotinic acid Statins (HMG CoA reductase inhibitors) TG-Lowering Drugs • Fibic acid 20-50% – Fenofibrate (Tricor) & Gemfibrozil (Lopid) • Nicotinic acid 20-50% – Niacin ER (Niaspan) • Statins 7-30% – Atorvastatin (Lipitor) & Simvastatin (Zocor) • Bile acid sequestrants No change – Cholestyramine (Questran) & Colestipol (Colestid) Question #14 • Which of the following classes of drugs can raise HDL the most? – – – – Bile acid sequestrants Fibric acids Nicotinic acid Statins (HMG CoA reductase inhibitors) HDL-Raising Drugs • Nicotinic acid 15-35% – Niacin ER (Niaspan) • Fibic acid 10-20% – Fenofibrate (Tricor) & Gemfibrozil (Lopid) • Statins 5-15% – Atorvastatin (Lipitor) & Simvastatin (Zocor) • Bile acid sequestrants 3-5% – Cholestyramine (Questran) & Colestipol (Colestid) JAMA 2001; 285: 2486-2497 Lipid-Lowering Medications and Effects on HDL Cholesterol Levels Ashen, M. D. et al. N Engl J Med 2005;353:1252-1260 Question #15 • What is the role of Ezetimibe (Zetia) in lipid-lowering drug therapy? Role of Ezetimibe • Inhibits intestinal absorption of cholesterol • Dose = 10 mg po qd • Ezetimibe alone LDL 18-20%, whereas Ezetimibe + Simvastatin LDL 44-61% – J Am Coll Cardiol 2002; 40: 2125-2134 – Mayo Clin Prac 2004; 79: 620-629 • Ezetimibe added to statin therapy helped 71% of patients achieve their target LDL – Mayo Clin Prac 2005; 80: 587-595 • No RCTs with clinical outcomes Question #14 • What is “intensive” statin therapy? Intensive Statin Therapy • PROVE IT – TIMI 22 – N Engl J Med 2004; 350: 1495-1504 • REVERSAL – JAMA 2004; 291; 1071-1080 • A to Z – JAMA 2004; 292: 1307-1316 • IDEAL – JAMA 2005; 294: 2437-2445 • TNT – N Engl J Med 2005; 352: 1425-1435 Treating to New Targets • • • • 10,001 adults aged 35-75 yo with CHD Atorvastatin (Lipitor) 10 mg qd v 80 mg qd Follow-up = 4.9 years LDL values – 10 mg – 80 mg 98 to 101 mg/dl 99 to 77 mg/dl • Primary outcome 22% – Composite of CHD death, nonfatal MI, resuscitation from cardiac arrest, and fatal or nonfatal stroke N Engl J Med 2005; 352: 1425-1435 References • “Executive Summary of the Third Report of the National Cholesterol Education Panel (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III).” JAMA 2001; 2486-2497. • http://www.nhlbi.nih.gov/guidelines/cholesterol/index.htm • Grundy SM, et al. “Implications of Recent Clinical Trials for the National Cholesterol Education Program Adult Treatment Panel III Guidelines.” Circulation 2004; 110: 227-239. • Cholesterol Treatment Trialists’ Collaborators. “Efficacy and Safety of Cholesterol-Lowering Treatment: Prospective Meta-analysis of Data from 90,056 Participants in 14 Randomized Trials of Statins.” Lancet 2005; 366: 1267-1278. References • Knopp RH. “Drug Treatment of Lipid Disorders.” N Engl J Med 1999; 341: 498-511. • Ashen MD, Blumenthal RS. “Low HDL Cholesterol Levels.” N Engl J Med 2005; 353: 1252-1260.