OB Review 2
advertisement
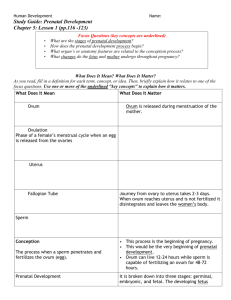
OB Review 2 February 2009 True Labor Contractions produce progressive dilatation and enfacement of the cervix. Occur regularly and increase in frequency, duration, and intensity. The discomfort of true labor contractions usually starts in the back and radiates around to the abdomen Not relieved by walking. FACTORS THAT MAY EXTEND OR INFLUENCE THE DURATION OF LABOR - 4 Ps Passage: Birth Passage: size and morphology of true pelvis, uterus, cervix, vagina, and perineum. Parity of woman. The True Pelvis is a primary concern when a vaginal delivery is expected. Passenger: Presentation of the fetus “part of the fetus that enters the pelvis first” (breech, transverse). Size of the fetus, moldability of the fetal skull. Powers: Quality, force and frequency of uterine contractions Psyche: mother’s attitude toward labor and her preparation for labor. Culture, Anxiety/Fear Passenger Fetal Presentation – Referred to the fetal presenting part. Part of the fetus that enters the pelvis first: Cephalic –presentation of any part of the fetus head during labor - Vertex Breech Shoulder. Fetal attidude – Relationship of fetal parts to one another: all joints in flexion Fetal lie – Relationship of cephalocaudal axis (spinal column) of fetus to the cephalocaudal axis of mother- transverse, parallel The fetal head normally engages in the maternal pelvis in an occiput transverse position, the vertex is formed by four bones of the Skull: the frontal bone, the 2 parietal bones and the occipital bone. In a vertex position when the occiput bone is the presenting part it refers to an occiput position. Vertex Presentation is a normal presenting position Left occiput anterior Positioning During Labor Assist the patient in turning from side to side. Side-lying promotes uteroplacental blood flow. Elevate the head of the bed 30 degrees; this makes it easier for the patient to breathe. May result in pressure of the enlarged uterus on the vena cava, reduces blood supply to the heart, decreases blood pressure, and reduces blood circulation to the uterus and across the placenta to the fetus. The best position for the patient is on her left side since this increases fetal circulation. Characteristics of Contractions Frequency: How often they occur? They are timed from the beginning of a contraction to the beginning of the next contraction. Regularity: Is the pattern rhythmic? Duration: From beginning to end - How long does each contraction last? Intensity: By palpation mild, moderate, or strong. 3/15/2016 8 Average Length of Labor . Latent Active Transition Second stage Primigravida 8 – 10 hours 6 hours 2 hours 1 hour Multigravida 5 hours 4 hours 1 hour 15 minutes Assessment of Contractions Palpation: Use the fingertips to palpate the fundus of the uterus Mild: Uterus can be indented with gentle pressure at peak of contraction – feels like tip of nose Moderate: Uterus can be indented with firm pressure at peak of contraction - feels like chin Strong: Uterus feels firm and cannot be indented during peak of contraction – feels like the forehead 3/15/2016 10 Impending signs of Birth Impending Signs of birth Bulging of the perineum. Crowning Dilatation of the anal orifice. Complaints of severe discomfort. Dilatation and effacement – complete - patient is instructed to push with each contraction to bring the presenting part down into the pelvis Amniotomy Artificial rupture of membranes performed at or beyond 3 cm dilation. May cause changes in the FHR ( accelerations or bradycardia). Assess and monitor FHR for one full minute Normal amniotic fluid is straw-colored and odorless. Stage 1 Latent: ends 4 cm Active: begins 4 cm ends 8 cm Transition: begins 8 cm ends 10 cm Stage 1 - Transition Phase Begins when cervix is dilated 8 cm, ends when cervix is dilated 10 cm. Contractions occur every 2 to 3 minutes Duration of 60 to 90 seconds. The intensity of contractions is strong. Completion of this phase marks the end of the first stage of labor. Urge to push or to have a BM 2nd Stage: Birth of the Baby Begins when cervical dilatation is complete and ends with birth of the baby. Dilatation and effacement – complete - Patient is instructed to push with each contraction to bring the presenting part down into the pelvis Third Stage of Labor The period from birth of the baby through delivery of the placenta. Dangerous time because of the possibility of hemorrhaging. Signs of the placental separation a. The uterus becomes globular in shape and firmer. b. The uterus rises in the abdomen. c. The umbilical cord descends three inches or more further out of the vagina. d. Sudden gush of blood. 4th stage Period from the delivery of the placenta until the uterus remains firm on its own. Uterus makes its initial readjustment to the non-pregnant state. The primary goal is to prevent hemorrhage from the uterine atony and the cervical or vaginal lacerations. Atony is the lack of normal muscle tone. Uterine atony is failure of the uterus to contract. Fourth Stage of Labor Referred as the Recovery Stage First 4 hours after the birth. Blood loss is usually between 250 mL and 500 mL. Uterus should remain contracted to control bleeding, positioned in the midline of the abdomen, level with the umbilicus. Mother may experience shaking chills. Intrathecal Block Injected into the subarachnoid space Rapid onset Less sedation No hypotension or motor block Precipitated Birth Suddenly occurring and unexpectedly without a physician or midwife to assist. Nursing intervention: Stay with mother Call for assistance Remain calm Open emergency birth pack Scrub if time permits As head crowns instruct mom to pant Suction newborn’s mouth and nose to prevent aspiration UMBILICAL PROLAPSE CORD 1. Cord is protruding from the vagina. Goal is prevention of fetal anoxia. Management includes positioning the mother on the left side in trendelenberg or in a knee-chest position and administering 100% oxygen. If the cord is exposed, cover it with saline moistened sterile gauze. STAT C-section is performed. Insert 2 fingers into the vagina with sterile gloves, and put pressure on the presenting part to relieve the compression of the cord. Oxytocin Infusion Safety Discontinue infusion with oxytocin if the following occur: Contractions are more frequent than every 2 minutes or duration is more than 90 seconds Uterus resting tone is more than 20 mm hg Fetal monitor shows: repeated late decelerations, prolonged decelerations or no variability Birth of an infant through an incision in the abdomen and uterus. Scheduled or unscheduled. When C/Section is unscheduled: the nurse needs to review with the client events before the C/Section to ensure the client understands what happened CESAREAN BIRTH The Postpartum Period Puerperium: Term 1st 6 weeks after the birth of an infant Neonate–newborn from birth to 28 days. Family adaptation to neonate: Bonding– rapid process of attachment during 1st 30 to 60 minutes after birth Mother, father, siblings, grandparents Uterine Involution Uterine Involution: return of the uterus to its prepregnancy size and condition. Normal postpartum uterus is firm and at midline Uterine fundal descent: uterus size of grapefruit immediately after birth Fundus rises to the umbilicus stays for 12 hours Descends 1 cm (fingerbreadth) each day for about 10 days Lochia Assessment Lochia–vaginal discharge after childbirth. It takes 6 weeks for the vagina to regain its prepregnancy contour. Lochia: scant-moderate, rubra, serosa or alba Assessment of lochia includes noting color, presence and size of clots and foul odor. Day 1- 3 - lochia rubra (blood with small pieces of decidua and mucus) Day 4-10 – lochia serosa (pink or pinkish brown serous exudate with cervical mucus, erythrocytes and leukocytes) Day 11- 21 - lochia alba (yellowish white discharge) Episiotomy Pain Relief Instruct Mother: Tighten her buttocks and perineum before sitting to prevent pulling on the episiotomy and perineal area and to release tightening after being seated. Rest several times a day with feet elevated. Practice Kegel exercise many times a day to increase circulation to the perineal area and to strengthen the perineal muscles. Breast Assessment Breasts: Soft, engorged, filling, swelling, redness, tenderness. Nipples: Inverted, everted, cracked, bleeding, bruised, presence of colostrum or breastmilk. Colostrum–yellowish fluid rich in antibodies and high in protein. Engorgement occurs by day 3 or 4. Due to vasoconstriction as milk production begins Lactation ceases within a week if breastfeeding is never begun or is stopped. Postpartum Psychosis A very serious type of PPD illness that can affect new mothers. Begin 2-3 weeks post delivery Fatigue, restlessness, insomnia, crying liable emotions, inability to move, irrationally statements incoherence confusion and obsessive concerns about the infant’s health Psychiatric emergency Nipple soreness is a portal of entry for bacteria - breast infection (Mastitis). Maternal after pains: may be due to breastfeeding and multiparity (loss of uterine tone) Always stay with the client when getting out of bed for the first time – hypotension effect and excess bleeding When assessing fundal height, if you notice any discrepancies in fundal height have patient void and then reassess. Postpartum Cesarean Incision site…redness swelling, discharge. Intact? Abdomen soft, distended? Bowel sounds heard all 4 quadrants Flatus? Lochia is less amount than in normal spontaneous vaginal delivery (NSVD) because uterus is wiped with sponges during c/section. If lochia indicates excessive bleeding, combine palpation and pain management measures. Auscultate breath sounds Fluid intake and output Pain? Assessment of Edema & Homan’s Sign Assess legs for presence and degree of edema; may have dependent edema in feet and legs. Assess for Homan’s sign- thromboembolism Negative Homan’s Sign is with No PAIN If there is pain then it is positive (+) and the nurse needs to report this finding immediately to the health care provider. Press down gently on the patient’s knee (legs extended flat on bed) ask her to flex her foot (dorsiflex) RhoGAM It is given to an Rh- mother within 72 hours after delivery of an Rh+ infant or if the Rh is unknown. Most people have Rh-positive blood. (Rh Factor) An inherited protein found on the surface of RBCs. A minority of individuals lack the Rh factor and are considered Rh-negative. If the baby's Rh positive blood enters a mother who is Rh Negative, then her immune system sees the cells as 'foreign' and will produce antirhesus antibodies to try to destroy them for her own self-protection. Thromboembolic Conditions Thrombophlebitis–the formation of a clot in an inflamed vein. Risk factors include maternal age over 35, cesarean birth, prolonged time in stirrups, obesity, smoking, and history of varicosities or venous thromboses. Prevention: client needs to ambulate early after delivery. Respiratory Distress Respiratory Distress Syndrome (RDS) RDS: preterm infants/surfactant deficiency Hypoxia, respiratory acidosis and metabolic acidosis Surfactant is produced by alveoli - lung maturity L/S ratio (lecithin-to-sphingomyelin ratio) is a test done before birth to determine fetal lung maturity. These phospholipids stabilize alveoli so that they do not collapse on exhalation Prophylactic Care Vitamin K –to prevent hemorrhagic disorders – vit k (clotting process) is synthesized in the intestine requires food for this process. Newborn’s stomach is sterile has no food. aquaMEPHYTON Hepatitis B vaccination –within the first 12 hours Eye prophylaxis –(Erythromycin Ointment) to prevent ophthalmia neonatorum – gonorrhea/chlamydia The Head and Chest The Head: Anterior fontanel diamond shaped 2-3 - 3-4 cms Posterior fontanel triangular 0.5 - 1 cm Fontanels soft, firm and flat head circumference is 33 – 35 cm The head is a few centimeters larger than the chest!!!! The Chest: circumference is 30.5 – 33 cm Vital Signs normal Temperature - range 36.5 to 37 axillary (97.7-98.6) Axillary vs Rectal about 0.2 to 0.5 difference Common variations Crying may elevate temperature Stabilizes in 8 to 10 hours after delivery Heart rate - range 120 to 160 beats per minute Apical pulse for one minute Common variations Heart rate range to 100 when sleeping to 180 when crying Color pink with acrocyanosis Heart rate may be irregular with crying Respiration - range 30 to 60 breaths per minute Blood pressure - not done routinely Ranges between 60-80 mm systolic and 40-45 mm diastolic. Common Normal Variations Acrocyanosis - result of sluggish peripheral circulation. Mongolian Spots: Patch of purple-black or blueblack color distributed over coccygeal and sacral regions of infants of African-American or Asian descent. Milia: Tiny white bumps papules (plugged sebaceous glands) located over nose, cheek, and chin. Erythema toxicum: Most common newborn rash. Variable, irregular macular patches. Lasts a few days. Erythema toxicum, acrocyanosis, milia and mongolian spots Caput succedaneum Swelling of the soft tissue of the scalp caused by pressure of the fetal head on a cervix that is not fully dilated. Swelling is generalized. may cross suture line and decreases rapidly in a few days after birth. Requires no treatment 2 – 3 days disappears Cephalohematoma Collection of blood between the periosteum and skull of newborn. Does not cross suture lines Caused by rupturing of the periosteal bridging veins due to friction and pressure during labor. Lasts 3 – 6 weeks Normal Reflexes Tonic Neck Reflex (FENCING) EXTENDS arm & leg on the side that the face points. Flexes opposite arm & leg 6-8 wks to 6 months Babinski Reflex is (+) This is Normal Birth to after walking 12-18 months age Gestational Age Relationship to Intrauterine Growth Normal range of birth weight for each week of gestation. Birth weight is classified as follows: Large for gestational age (LGA): weight falls above the 90th percentile for gestational age Appropriate for gestational age (AGA): weight falls between the 90th and 10th percentile for gestational age Small for gestational age (SGA): weight falls below the 10th percentile for gestational age Newborn – Term vs Preterm The premature newborn has no flexion of extremeties Full term newborn is fully flexed. Skin in a preterm is very transparent and thin Veins disappear as subcutaneous fat is deposited. Lanugo is most abundant at 28 to 30 weeks gestation a small amount may remain at full term Eyelids are fused until 26 to 28 weeks gestation Ears when folded remains folded at 32 weeks and by 36 weeks there is enough cartilage for the ear to return to its original state when folded. Bathing the Newborn No tub bath until after the cord has fallen off and healing is complete. Newborn’s first baththe nurse needs to wear gloves to prevent infection. What is wrong with this nursing action? Circumcision Circumcision is considered an elective procedure Anesthesia should be provided. Parents must give written consent Full term health infants Aftercare: Check hourly for 12 hours Check for bleeding and voiding Before discharge: Newborn goes home within the first 12 hours after procedure Bleeding should be minimal and infant must void Breastfeeding Colostrum is rich in immunoglobulins to protect newborn GI tract from infection; laxative effect. Breast milk in 2 weeks sufficient nutrients 20 kcal/oz (infant’s nutritional needs) To support Breastfeeding: Mother needs to consume extra 500 calories per day. Feeding length: should be long enough to remove all the foremilk (watery 1st milk from breast high in lactose - skim milk & effective in quenching thirst) Hindmilk: higher in fat content leads to weight gain and more satisfying. Breastfeeding time approximately 30 minutes Infant Formula Formula 7.5 ml to 15 ml at feeding gradually increase to 90 ml to 120 ml at each feeding in 2 weeks. Formula preparation: mixing must be accurate to provide the 20 kcal/oz. (newborn nutritional need) Burping: is needed to expel air swallowed when infant sucks. Should be done about halfway through feeding for bottle feeders and when changing breasts for breast feeders. Hyperbilirubinemia Physiologic Jaundice =Appears 24 hours after birth peaks at 72 hrs. Bilirubin may reach 6 to 10 mg/dl and resolve in 5 to 7 days. Due to Unconjugated bilirubin circulating in the blood stream that is deposited in the skin. Immature liver unable to conjugate bilirubin released by destroyed RBC. Pathologic Jaundice =Not appear until after 24 hrs leads to Kernicterus (deposits of bili in brain). Bilirubin >20mg/dl The most common cause is Rh incompatibility. Neural Tube Defects 3 types: Spina Bifida Occulta: failure of the vertebral arch to close. Has dimple on the back with a tuft of hair. No treatment required. Meningocele: saclike protrusion along the vertebral column filled with cerebrospinal fluid and meninges. Surgery required. Myelomeningocele: saclike protrusion along the vertebral column filled with spinal fluid meninges, nerve roots, and spinal cord = paralysis. Surgical repair required. Sterile saline dressing. hydrocepalus Spina bifida occulta Spina bifida Occulta meningocele myelomeningocele Infants of DM mothers (IDM) Complications Hypoglycemia: maternal glucose declines at birth. Infant has high level of insulin production= decreases infant’s blood glucose within hours after birth. Respiratory Distress: less mature lungs due to insulin Hyperbilirubinemia: hepatic immaturity, increased hematocrit, bruising due to difficult delivery. Birth trauma: large size of infant Congenital birth defects: birth defects – Patent Ductus Arteriosus, Ventricular Septal Defect and more.