Respiratory Failure
advertisement

Diabetic Emergencies
Sa’ad Lahri
Registrar
Dept Of Emergency Medicine
Outline
• Hypoglycaemia
• Diabetic Ketoacidosis (DKA)
• Hyperglycemic Hyperosmolar state
(HHS)
• Lactic Acidosis
Hypoglycaemia
• Case Study
• 55 y old diabetic brought to ER with history of “L
CVA” by EMS crew.
• Management en - route: “calmed and
reassured”
• Glucose in ER = 1,1 mmol/l
• Nurses records: “seen by Dr X and 50mls 50%
dextrose given IV. Patient now talking and
moving all limbs freely”
• Definition: blood glucose level <2.5 mmol/l
Postgrad Med J 2007; 83:79-86
Principles of Disease
• Protection against hypoglycaemia :
• Cessation of insulin release and
mobilisation of counter regulatory
hormones – increase in glucose
production and decrease glucose use.
Rosen’s Emergency Medicine 6th Ed
Causes of hypoglycaemia
Hypoglycaemic admissions among diabetic patients in Soweto, South Africa
• A total of 51 episodes of
biochemically confirmed
hypoglycaemia (blood glucose
< 2.2 mmol/l with coma or precoma, and requiring
intravenous glucose) were
observed in 43 patients.
Inappropiate
Tx,18%
Gliclazide
33%
GIT upset
20%
Gliclazide
Missed meal
Alcohol
GIT upset
• Important to check for sepsis,
renal failure, heart failure,
accidental overdose
Alcohol
22%
Missed
meal 36%
Inappropiate Tx
Diabet Med. 1993 Mar;10(2):181-3
Metformin and hypoglycaemia?
• Metformin – decreases hepatic production
of glucose and increases insulin
sensitivity.
• Symptoms of OD : nausea, vomiting,
abdominal pain and lactic acidosis.
• Lactic acidosis can be fatal
Emergency Medicine Secrets 4th Ed
Hypoglycaemia due to OD
• OD – delayed hypoglycaemia
• Observation period – 12-16hrs
• Sulphonylurea – Octreotide
Emergency Medicine: Just the facts 2nd Ed
Diagnostic Strategies
• Cardinal test: blood glucose (before therapy)
• Finger prick : beware insufficient sample
• Other tests should address aetiology (eg sepsis)
• Factitious hypoglycaemia: low levels of Cpeptide helpful
Rosen’s Emergency Medicine 6th Ed
Clinical Symptoms and signs
• Autonomic: (sweating, anxiety, nausea,
palpitations and hunger) (3.3 – 3.6 mmol/l)
• Neuroglycopenia: confusion, drowsiness, altered
behaviour and focal deficits. (<2.6 mmol/l)
Postgrad Med J 2007; 83:79-86
• ABCD “EFG”
• Doctor “she is extending” (glucose 1mmol/l)
Management
• Alert with mild symptoms – sugar
containing food
• Unable to take po – IV 50 mls 50 %
dextrose.
• 30% gel (hypostop) buccal mucosa
Postgrad Med J 2007; 83:79-86
• Irritant to veins – venous sclerosis rebound hypoglycaemia. Problem children
Rosen’s Emergency Medicine 6th Ed
Dextrose 10% or 50%?
Emerg Med J 2005; 22:512-515
• Dextrose 10% or 50% in the treatment of hypoglycaemia
out of hospital? A randomised controlled trial:
• Main outcome measures: To compare for each
dextrose concentration the time to achieve a Glasgow
Coma Scale (GCS) score of 15, and the dose required to
obtain a blood glucose level of 4.5 mmol/l.
• Results:
• No statistically significant differences in median time to
recovery
• Dextrose 10 % lower post treatment glucose levels
• Thiamine if alcohol abuse
• No IV – 1mg Glucagon IM.
• Onset of action 10 -20 mins and peak
response 30-60 mins.
• Ineffective if glycogen absent – alcohol
induced hypoglycaemia.
Rosen’s Emergency Medicine 6th Ed
“Appropiate Disposition”
• Admit/observe – suicidal ; excessive amounts of
oral hypoglycaemics or long – acting insulin.
Persistent altered mental status.
Emergency Medicine Secrets 4th ED
• Hypoglycaemia uncomplicated by other disease
– discharged if caused found and corrected.
• Give meal before discharge – ability to tolerate
oral feeds and replenish glycogen stores.
Rosen’s Emergency Medicine 6th Ed
What about Non – diabetic
Patients?
• Classify as Postprandial or fasting.
• Postprandial: alimentary hyperinsulinism –
gastrectomy, fructose intolerance.
• Fasting: imbalance production and use.
• Underproduction: hormone deficiencies,
liver disease.
• Overuse: hyperinsulinism ; drugs,
insulinoma, tumours.
Rosen’s Emergency Medicine 6th Ed
Case Study 2
• Referral letter from Primary Care:
• 19 y old male presents with hx of nausea,
vomiting and abdominal pain.
• Notice him to be dehydrated with acidotic
breathing
• Glucose … HI!
• Urine 3+ ketones
• Diagnosis … Diabetic ketoacidosis
DKA
•
•
•
•
•
•
•
•
Triad of:
hyperglycaemia, ketosis and acidaemia.
Diagnostic criteria (ADA)
Blood glucose >14
Ph <7.30
Serum Bicarb <18mmol/l
Anion Gap >10
Ketonaemia
Postgrad Med J 2004; 80: 253-61
Precipitants
QJ Med 2004;97:773 -780
• Infections and inadequate insulin doses.
• Most frequent dx infections: pneumonia
and UTI. Check for meningism &PID
• Others include Myocardial infarction, CVA,
pulmonary embolism
Postgrad Med J 2004; 80: 253-61
History and Physical Exam
• DKA usually short time (<24hrs)
• Classic clinical picture: polyuria,
polydipsia, weight loss, vomiting,
abdominal pain, dehydration, weakness,
mental stage change and coma.
Diabetes Care 2006;29: 2739 - 2747
Physical findings:
•
•
•
•
•
•
•
•
Poor skin turgor
Kussmaul respirations
Tachycardia
Hypotension
Shock
Coma
Severe hypothermia poor prognostic sign.
Abdominal pain may be present – 50-75% resolves
correction of hyperglycaemia and acidosis.
• Abdominal pain? – dehydration of muscle tissue,delayed
gastric emptying and ileus Postgrad Med J 2004; 80: 253-61
Diabetes Care 2006;29: 2739 - 2747
Endocrinol Metab Clin N Am 35 (2006) 725–751
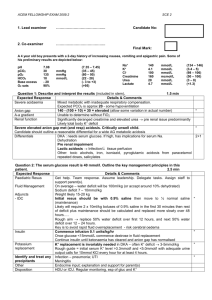
Laboratory Tests and Evaluation
• ABG not necessary – can use venous
blood
• Lab: Na, K , Urea, Creatinine
• Serum ketones
• Culture of blood and urine if clinically
indicated.
• ECG and CXR
• Preg test if female
Postgrad Med J 2004; 80: 253-61
Discussion of tests
• Leucocytosis common finding – stress and
dehydration.
• Leukocytosis above 25000 suggests
ongoing infection. Band neutrophils high
sensitivity and specificity.
• Na : usually low osmotic flux of water.
• If high profound water loss.
• K: may be up due to extracellular shift
Endocrinol Metab Clin N Am 35 (2006) 725–751
Management Aims
Correct
Acidosis
Hyperglycaemia
Electrolytes
Precipitant
Fluids
Insulin
Potassium
Education
EMJ 2003, 20 :210-213
Fluid Therapy
• Controversy is rife!!!
• Which fluid?
• How much?
• At what rate?
Which Fluid?
• Current guidelines ADA – Initial Fluid 0.9%
Saline
• Other’s prefer Hartmann’s.
• 0.9% Saline – hyperchloraemiac
metabolic acidosis
• Hartmann’s – 29mmol/l lactate. In DKA
high lactate to pyruvate ratio.
• Hartmann’s – generate glucose from
lactate
BMJ 2007;334:1284-5
• Hartmann’s – 5mmol/l K. DKA patient may
be hyperkalaemic
• 0.9% saline acidotic Ph 4.5
• Hartmann’s Ph 6,0
• Need a trial !
BMJ 2007;334:1284-5
Fluid replacement
• Aim to expand extracellular volume and
restore renal perfusion.
• Rate of 15-20ml/kg hour or 1-1.5l 1st hour.
• Subsequent choice depends on state of
hydration, serum electrolytes and urine
output.
• O.45% NaCl at 4-14ml/kg/hr if hyperNa or
euNa 0.9% if hypoNa
• Glucose <14 mmol/l 5% glucose
containing solutions at 100-125mls/hr.
• Change in osmolality not exceed 3
mmol/kg/hr
CMAJ 2003;168(7) 859 -66
GF Jooste Clinical Guidelines 2007
•
•
•
•
•
•
Richardson, Meintjies and Burch:
1l N/S stat
1l over 1 1hr
1l over 2 hrs
1l over 4hrs
1 litre 6 hrly
Insulin
• Continous IV infusion
• IV bolus 0.1 u/kg
• Not subcut or IM for shocked. May used mild
DKA or no infusion available.
• If K >3.3 0.1 U/kg per hour.
• Gradual decline 3-4 mmol/l/hr.
• If level not drop 3mmol in first hour infusion may
be doubled.
• When Glucose level reaches 12-14 mmol/l
insulin rate may be decreased by 50% as 5%
dextrose is added
Diabetes Care V 29:12 Dec 2006
GF Jooste Protocol
• Infusion 50 units Actrapid in 200mls
Normal saline at 24mls/hr (6mls/hr)
• Visidex <15:
change to rehydration fluid
• Visidex 10-15: 24 mls/hr
• Visidex 4-10: 12mls/hr
• Visidex <4:
stop Actrapid 2 hrs and
50mls 50% dextrose
•
•
•
•
Once the ketoacidosis has been corrected
Glucose <11.0 mmol/l
Serum Bicarb >18 mmol/l
Venous Ph >7.3 and patient able to eat
• Multi dose insulin regimen may be
started
Diabetes Care V 29:12 Dec 2006
Potassium
• Total body potassium depleted.
• May get hyperK because of acidosis.
• Give 20-30mmol K to each litre to maintain K 4 and 5 mmol/l.
• If K < 3.3 mmol/l give K & delay insulin therapy
to avoid arrhythmias
Diabetes Care V 29:12 Dec 2006
Bicarbonate therapy
(could be a presentation on its own)
• Use remains controversial.
• Ph>7.0 insulin blocks lipolysis and
resolves ketoacidosis.
• Disadvantages: Increased risk of
hypokalaemia, decreased tissue oxygen
uptake, cerebral oedema and may even
augment ketone production.
Diabetes Care V 29:12 Dec 2006
Bicarb
• If Ph <7,0 ADA recommends 50mmol
bicarb in 200mls sterile water with 10
mmol of K over 1 hr till ph >7,0.
• No studies PH <6.9. Risk of impaired
myocardial contractility
• 100mmol bicarb in 400mls sterile water
with 20 mmol K at 200mls/hr for 2 hrs until
venous ph >7,0
Endocrinol Metab Clin N Am 35 (2006) 725–751
What about Phosphate and
Magnesium?
• Phosphate: replacement not required for
routine correction. May be harmful –
hypocalcaemia.
• If potential complications of
hypophosphatemia – replacement may be
justified.
• Cydulka and Pennington in Rosen’s 6th Ed
recommend Mg 0.35mEq/kg in fluids, 1st 3
-4 hrs.
Postgrad Med J 2004; 80: 253-61
Treatment related complications
•
•
•
•
Hypoglycaemia – poor monitoring
Hypokalaemia – inadequate replacement
Heart Failure – too much fluid
Cerebral oedema – correct water and
sodium deficits slowly. Suspect if
comatose after reversal of acidosis
CMAJ 2003; 168 (7), Rosen’s Emergency Med 6th ed
• Non cardiogenic pulmonary oedema – due
to increased water in lungs and reduced
lung compliance.
• Hyperchloraemic metabolic acidosis: loss
of ketanions necessary for bicarb
regeneration, use of 0.9% saline.
• Acidosis: no adverse effects and corrects
spontaneously
CMAJ 2003; 168 (7)
CASE STUDY 3
• 64 y old type 2 diabetic presents to EU
with hx from family “doc, I had difficulty
waking my mum this morning. She’s
confused”
• Good doc, you check hgt = 48 mmol/l and
notice her to be dehydrated.
• Diagnosis …
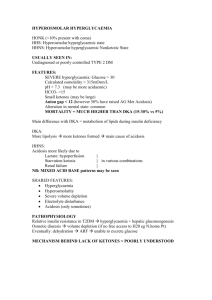
Hyperglycaemic hyperosmolar
state
• HHS replaces “hyperosmolar non-ketotic
coma”
• Alterations in sensoria may be present
without coma.
• Mild to moderate ketosis is commonly
present.
• Kitabchi et al …
Postgrad Med J 2004;80:253–261
Postgrad Med J 2004;80:253–261
Predisposing and precipitating
factors
• Infection (eg, pneumonia, urinary tract infection,
and sepsis) is the most common precipitating
illness, occurring in up to 60% of cases
• others - provoke release of counter regulatory
hormones and precipitate HHS include silent
myocardial infarction, cerebrovascular accident,
pulmonary embolism, and mesenteric
thrombosis
Emerg Med Clin N Am 23 (2005) 629–648
Clinical Presentation
• Type 2 diabetics with more insidious onset.
• Polyuria, polydipsia and weight loss over several
week’s duration.
• May have focal neurological signs
• Coma is associated with severe hypertonicity,
with serum osmolarity at 350 mOsm/L or greater,
and usually more significant hypernatremia than
hyperglycemia
• Dehydration
Postgrad Med J 2004;80:253–261
hypoglycaemia
hyponatraemia
sepsis
Diff Diagnosis
Uraemia
Drug od
Emerg Med Clin N Am 23 (2005) 629–648
• Calculate effective osmolarity, which
reflects actual tonicity, the osmotic
pressure of a solution.
• The normal serum osmolarity 275 to 295
mOsm/L. Levels above 320 mOsm/L alteration in cognitive function
Emerg Med Clin N Am 23 (2005) 629–648
Lab investigations
• serum glucose, serum urea ,creatinine,
electrolytes, serum ketones, osmolality,
urinalysis
• complete blood count with differential.
• arterial blood glasses if respiratory
compromise or acidosis is suspected.
• Bacterial cultures of urine and blood
almost always are indicated.
Emerg Med Clin N Am 23 (2005) 629–648
Sodium
• glucose osmotically shifts water into the
extracellular space, sodium is diluted, and
the measured value is decreased falsely.
• Corrected Na mmol/l = plasma Na +
(1.6x{plasma glucose-5.6})/5.6
• Na high – water loss and dehydration
Emerg Med Clin N Am 23 (2005) 629–648
Other studies
• ECG - to look for signs of ischemia and
infarction, and acute changes related to
electrolyte deficiencies.
• CXR – check for pneumonia
Emerg Med Clin N Am 23 (2005) 629–648
Goals of therapy
Haemodynamic
Stability
Electrolyte
homeostasis
Correction
Of hyperglycaemia
&hyperosmolarity
Find precipitant
Avoid complications
Emerg Med Clin N Am 23 (2005) 629–648
Fluids
• Replace one half of the fluid deficit in the first 12 hours
and the remainder in the next 12 to 24 hours
• Initial replacement should be with isotonic crystalloid (eg,
0.9% sodium chloride).
• The ADA guidelines - corrected serum sodium.
• If it is normal or elevated, 0.45% sodium chloride is
infused at 4 to 14 mL/kg per hour depending on
hydration state
• If low, 0.9% sodium chloride is continued at the same
rate
• Beware underlying disease states!
Emerg Med Clin N Am 23 (2005) 629–648
• Potassium – similar to DKA outlined earlier
• Low K greatest risk of complications
including cardiac dysrhythmias, cardiac
arrest, and respiratory muscle weakness.
Emerg Med Clin N Am 23 (2005) 629–648
Insulin
• Secondary role.
• Fluids always precede insulin administration.
• Insulin drives glucose, potassium, and water into
cells, and administration of insulin alone could
lead to circulatory collapse, shock, and even
thromboembolism if fluid has not been replaced
first.
• Dose similar to DKA outlined earlier
Emerg Med Clin N Am 23 (2005) 629–648
Complications
• Reasons for mortality – theories…
• Elders – cardiac and renal disease.
• Thromboembolic events, cerebral edema,
adult respiratory distress syndrome, and
rhabdomyolysis may occur.
• Low dose subcut heparin - thrombosis
see notes – click end show
Rosen’s Emergency Med 6th Ed
Case Study 4
• 75 yold diabetic, hypertensive on oral
hypoglycaemics presents to EU 2 day history of
vomiting, abdominal pain.
• O/E: confused, restless found to be in Cardiac
failure clinically.
• Hgt: 6,0
• Gas: ph 6.96 PC02 5.4 P02 9,0 HCo3 14
BE: -12. lactate 7,0 mmol/l
Diagnosis: ……………….
Postgrad Med J 2004; 80:253-261
Discussion:
Diabetes and Lactic Acidosis
Definition:
• Severe lactic acidosis is defined as a high
anion gap metabolic acidosis with a blood
lactate concentration 5.0 mmol/l (normal
0.4–1.2 mmol/l).
• The pathological elevation of lactate and
hydrogen ions may result from
overproduction or delayed clearance of
lactate, or a combination of both.
Postgrad Med J 2004; 80:253-261
Type A lactic acidosis
(anaerobic/hypoxic)
• Type A lactic acidosis (anaerobic/hypoxic)
occurs in states of profound tissue hypoxia such
as myocardial infarction, cardiogenic shock, or
profound sepsis.
• Anaerobic metabolism produces excess lactate
that swamps the body’s capability to clear it and
clearance of lactate may also be decreased.
• This situation is not peculiar to diabetes but
people with diabetes (particularly type 2
diabetes) are at increased risk of hypoxic
cardiovascular complications.
Postgrad Med J 2004; 80:253-261
Type B lactic acidosis (aerobic)
• Type B lactic acidosis (aerobic) is rarer and is
associated with a number of systemic diseases
(including diabetes), drugs, toxins, and inborn errors of
metabolism.
• The biguanides metformin and phenformin, used in the
treatment of type 2 diabetes, have both been associated
with the development of type B lactic acidosis.
• Phenformin was withdrawn from the market because of
this complication; the incidence of lactic acidosis is much
lower with metformin, with an estimated incidence of
0.03 episodes per 1000 patient years.
Postgrad Med J 2004; 80:253-261
Metformin
• May be either type A lactic acidosis, where the acidosis
is the result of concurrent complicating illness without the
accumulation of metformin; type B arising from marked
metformin accumulation without concurrent hypoxic
factors; or mixed.
• 90% of absorbed metformin is excreted unchanged by
the kidneys ; so - renal function that determines
metformin clearance.
Postgrad Med J 2004; 80:253-261
Metformin
• The principal contraindication - is renal
impairment: the American Diabetes
Association recommends avoiding
metformin use if serum creatinine
concentration exceeds 125 mmol/l.
• Because of the accumulation of lactate in
hypoxia, metformin is also contraindicated in
conditions such as uncontrolled heart failure that
predispose to lactic acidosis.
Postgrad Med J 2004; 80:253-261
Clinical Presentation
• Hyperpnoea (Kussmaul respiration), nausea,
vomiting,diarrhoea, epigastric pain, anorexia,
lethargy, thirst, and decreased level of
consciousness.
• Hypotension, hypothermia, cardiac
dysrhythmias, and respiratory failure may also
occur in severe metformin-associated lactic
acidosis.
• Blood glucose levels: low, normal, or high in
diabetic subjects.
Postgrad Med J 2004; 80:253-261
Management
• Treatment of lactic acidosis includes appropriate
supportive care (usually on an intensive care unit),
treatment of any concomitant condition and elimination
of any offending drug by renal excretion or dialysis.
• Bicarbonate therapy is still one of the principal
management modalities for lactic acidosis despite
conflicting reports as to its efficacy and even reports of
potential adverse consequences.
• Metformin is a dialysable drug and the use of
bicarbonate in combination with haemodialysis has been
successful.
Postgrad Med J 2004; 80:253-261
summary
• Prognosis in lactic acidosis of all causes is poor with only
between 12%–17% of patients surviving to discharge in
one well conducted study. N Engl J Med 1992;327:1564–9.
• In summary, general management of the underlying
condition, appropriate supportive care, bicarbonate
therapy and haemodialysis are the key approaches to
the management of severe lactic acidosis.
• Further trials needed before we can be clear as to what
represents optimum care.
Postgrad Med J 2004; 80:253-261
Conclusion
“Many Cases of DKA and HHS can be
prevented by better access to medical
care, proper education and effective
communication with the health care
provider during the intercurrent illness”
Acknowledgements:
Prof Wallis
Prof Pons
Prof Mattu
Prof Cydulka
Kitabchi et al
Diabetes Care V 29 : 12
December 2006
Hyperglycemic crises in adult patients with
diabetes