Georgia Association of Radiologic Technologists
advertisement

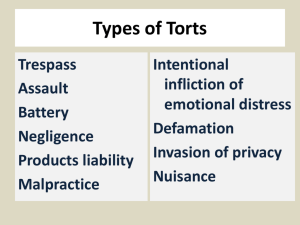
GSRT: An Hour with the Enemy Charles A. Dorminy, J.D., LL.M. Hall, Booth, Smith & Slover, P.C. 220 East 2nd Street Tifton, Georgia 31794 Email: cad@hbss.net Phone: (229) 382-0515 Malpractice Payments by Nursing Category 1998-2001 Roadmap • • • • Overview of lawsuits Law regarding Documentation Pitfalls and Issues Examples Common Themes of Suits • Plaintiff attorneys with expertise in medical negligence cases. • A sympathetic Plaintiff. • The lawsuit names not only the radiologist but other medical specialties. Each physician’s defense is at odds with the other. • Bad outcome which was preventable but for “Your” negligence. • Well-traveled, experienced medical “experts” who make thousands of dollars in testifying based upon opinions made in hindsight. Time Limitations • A lawsuit must be filed generally within two years of date of injury. This is known as the statute of limitations. The statute of limitations, is extended if a minor is involved. • A claim not filed within five years of the date of negligence is barred by the statute of repose. This is absolute. What happens in a lawsuit? • Pleading: – Complaint – Answer within 30 days • Discovery – – – – – Obtain medical records, interviews, meetings Interrogatories Requests for Documents Non-Party Requests for documents Depositions What happens in a lawsuit? • • • • Expert witness reviews Deposition of experts Motion for Summary Judgment Alternative Dispute Resolution – Arbitration, Mediation, Negotiation • Trial Two potential claims 1. Negligence – Malpractice or Simple 2. Battery – Unlawful touching Negligence or Malpractice • Simple Negligence – A mere breach of duty – i.e. Dropping a patient • Professional Negligence or Malpractice – Requires exercise of professional judgment – i.e. Sticking patient in the wrong place To Prove Negligence (either) Duty +Breach (in standard of care) +Proximate causation +Damages __________________ Negligence Overview of Negligence • "A medical provider who undertakes to perform professional services for a patient must use reasonable care to avoid causing injury to the patient. • The knowledge and care required of the physician is the same as that of other reputable physicians practicing in the same or a similar community and under similar circumstances. Overview of Negligence • A medical provider not only must have that degree of learning and skill ordinarily possessed by other reputable providers but also must use the care and skill ordinarily used in like cases. • A failure to have and use such knowledge and skill is negligence." Georgia Pattern Jury Instructions First Element • Duty – Plaintiff (person suing) must prove that there was a “doctor patient” relationship – You all owe your patients a duty to act reasonably. – Most patients do not know the rad techs prior to exam • i.e. they didn’t choose you – Do you have a relationship with patient? • Perform x-ray etc on patient • If you’re in the record (or supposed to be) then you have a duty Second Element: Breach of “Standard of Care” • Standard of Care: – “Reasonable and customary medical practice in like circumstances” • There is no requirement of a perfect result. • Cannot blame the medical provider solely because of a bad result, no matter how bad the result. Second Element: Breach of “Standard of Care” • Defendants are presumed to have complied with the standard of care • Plaintiffs have the burden of proof – By a “preponderance of the evidence” – Must tip scales slightly in their favor, that’s I • Plaintiffs must overcome presumption with “competent expert” testimony Competent Experts • Active practice in defendant’s profession or specialty for at least 3 of the 5 years prior to the date of injury – “You too can be an expert!” • Actual professional knowledge and experience in the area of practice or specialty in which the opinion is to be given. – “But I’ve never done it before” • Up to the discretion of the trial judge • Doctors can testify about nurses – But can Radiologists testify about rad techs? (O.C.G.A. 24-9-67.1 effective 2/16/05) Experts • Competent to offer opinions about rad techs based upon education, training and experience Expert’s Opinions • Must be accepted within the medical community. • Not “junk” science Third Element • Proximate Causation – Plaintiff (person suing) must prove that she suffered injuries as a result of the defendant’s (person being sued) negligent act or omission and injuries would not otherwise have occurred. – Proof to reasonable degree of medical certainty • more likely than not Fourth Element • Damages – If those three elements (duty, breach in the standard of care, and proximate cause) are proven, defendant will be liable for the resulting damages – No harm no foul Malpractice for Rad Techs • Not a lot out there • Usually sue the radiologist and/or Hospital – They may blame it on you – Documentation is your defense Two potential claims 1. Malpractice – Negligence 2. Battery – Unlawful touching Battery • Unlawful touching • Any unauthorized and unprivileged contact by a medical provider with his patient in examination, treatment or surgery would amount to a battery. • In the interest of one's general right of inviolability of his person, any unlawful touching of that type is a physical injury to the person and is actionable. Consent • No battery if consent is obtained • Consent to medical or surgical treatment may be manifest by acts and conduct, and need not necessarily be shown by writing or by express words • It may be implied from voluntary submission to treatment with full knowledge of what is going on • What about withdrawal of consent? Withdrawal • Withdrawal after examination is in progress 1. The patient must act or use language which can be subject to no other inference and which must be from a clear and rational mind. • Must be such as to leave no room for doubt in the minds of reasonable men that in view of all the circumstances consent was actually withdrawn. 2. It must be medically feasible to stop at that point without the cessation being detrimental to the patient's health from a medical viewpoint. Withdrawal • The burden of proving each of these essential conditions is upon the plaintiff, and with regard to the second condition, it can only be proved by medical evidence as medical questions are involved. • #2 requires expert testimony Mims v. Boland • • • • Patient underwent barium enema Previous colon resection Had colostomy Claims withdrawal during procedure Mims v. Boland • "When [the doctor] . . . started giving me the enema he was going to insert [the bardex catheter tube] . . . into the colostomy and I told him, 'Better let me insert that tube because I am in the habit of taking an enema and I know how to insert these rubber tubes without hurting, because there is such a crook in the colostomy, it has to go part one way and then has to be turned, because it can't go just right straight down.' Mims v. Boland • "He said, 'No, you don't know how to do it,' and he continued with this thing, and I tried to take it out of his hand and he wouldn't let me have it. He said, 'No, you can't do it.‘ • "So with that he shoved that thing right into my colostomy and right on in and just nearly killed me. • "And then when he started pouring that barium into that tube that had been inserted, he poured so much I said, 'I can't take all of the barium because I don't have but a very small part of my large colon,' and of course he didn't know anything about what I had had done and he still kept giving me more. Mims v. Boland • 'That is just all I can take. It's just killing me,' and I just kept getting very, very terrible pains and suffering terrible all the time he was giving it to me. . . "I was in such intense pain and that I didn't think I could stand it and I just kept begging both of them not to give me any more of it. . . "Oh I just suffered terrible, I suffered torture, started into just rigors and just shaking, and they had to hold me on the table. . ." Mims v. Boland • Court said not an effective withdrawal • “…merely shows protestations by the plaintiff of pain and discomfort and disagreement with the defendants in the manner they administered the barium enema.” Battery: Final Thoughts • From my perspective, if even close to withdrawal, stop and have them confirm they want to go forward • If they want to stop, go get the doctor • Costly to defend: – – – – Depositions Expert testimony Motion trial What causes lawsuits? • These plus injury lead to suit: – Poor documentation – Failure to Chart – Incomplete Documentation – Charting before Doing – Charting well after Doing Best Defense: Good Offense • Documentation: – Crucial to the medico-legal process – One of the most critical aspects of defense • The medical record must be complete and as accurate as possible when introduced into evidence Legal View of Documentation • “If it wasn’t documented, it didn’t happen.” – Not true; many ways to prove you did it – But easier when documented Law Joint Commission State Regulations Hospital Policies and Procedures Joint Commission • IM.6.20.1: Medical Records contain, as applicable, information addressing 18 clinical / case information areas: 1. Emergency care, treatment, and services provided to the patient before his or her arrival 2. Documentation and findings of assessments 3. Conclusions or impressions drawn from medical history and physical examination 4. Diagnosis, diagnostic impression, or conditions 5. Reason(s) for administration of care, treatment, and services IM.6.20.1 6. Goals of the treatment and treatment plan 7. Diagnostic and therapeutic orders 8. Diagnostic and therapeutic procedures, tests, and results 9. Progress notes made by authorized individuals 10. Reassessments and plan of care revisions IM.6.20.1 11. Relevant observations 12. Response to care, treatment, and services provided 13. Consultation reports 14. Allergies to food and medicines 15. Medications ordered and prescribed IM.6.20.1 16. Dosages of medications administered a. b. c. d. e. Strength, dose, or rate of administration Administration devices used Access site or route Known drug allergies Adverse drug reactions IM.6.20.1 17. Medications dispensed or prescribed on discharge 18. Relevant dosages / conditions established during course of care, treatment, or services IM.6.20.2 • Medical Records contain the following demographic information: – Patient’s name, sex, address, date of birth, and authorized representative – Legal status of patients receiving behavioral health care services – Patient’s language and communication needs IM.6.20.3 • Known evidence of advanced directives • Evidence of informed consent • Records of communication with patient regarding care, treatment, and services – Discussion of withdrawal of consent Law Joint Commission State Regulations Hospital Policies and Procedures State Regulations • Why are they important? – Lose your license – Hospital may lose its license • Ga. Comp. R. & Regs. r. 290-9-7-.18 (2007) State Regulation • Entries in the Medical Record – All entries in the patient's medical records shall be • accurate • legible and – Shall contain sufficient information to support the diagnosis State Regulation • Describe: – The treatment provided – The patient's progress – Response to medications and treatments. • Inpatient records shall also contain sufficient information to justify admission and continued hospitalization. State Regulations – All entries shall include: • The date of the entry and • The signature of the person making the entry – Late entries shall be labeled as late entries State Regulations • Verbal / Telephone Orders – The hospital, through its medical staff policies, shall appropriately limit the use of verbal/telephone orders – Shall be used only in situations where immediate written or electronic communication is not feasible and the patient's condition is determined to warrant immediate action for the benefit of the patient – Shall be received by an appropriately license or otherwise qualified individual as determined by the medical staff in accordance with state law. State Regulations • Verbal / Telephone Orders – The individual receiving the verbal/telephone order shall: • Immediately enter the order into the medical record • Sign and date the order, with the time noted, and • Enter the dose to be administered. State Regulations • Verbal / Telephone Orders – The individual receiving the order shall immediately repeat the order – The prescribing physician or other authorized practitioner shall verify that the repeated order is correct – The individual receiving the order shall document, in the patient's medical record, that the order was "repeated and verified.“ State Regulations • Verbal / Telephone Orders – Shall be authenticated by the physician or other authorized practitioner giving the order, or by a physician or other authorized practitioner taking responsibility for the order, in accordance with hospital and medical staff policies Law Joint Commission State Regulations Hospital Policies and Procedures Policies and Procedures • Developed by hospital • Usually will specify what should be included in the record for any given situation – But not all situations • NOT Standard of Care • But can be used to show competence • Should guide your care and treatment • Study your policies and procedures • Will be asked about them in deposition Pitfalls and Issues Pitfalls & Issues • Common Pitfalls: • Opinions are charted • Not facts • Generic language used • For example “Verbalized understanding” for a comatose patient • Entries are obliterated • White out • All charting is done at end of shift Pitfalls & Issues • Physician may be notified but its not in the record • Charting for someone else • Symptoms are charted but not what was done about it, • i.e. pain during enema, etc. • Stop procedure? • Response to treatment • pain reduced? Pitfalls & Issues • Patient’s record is obviously altered • Unacceptable abbreviations are used • Vague descriptions are documented – “a large amount” • Excuses are given – “Meds not given because not available” – So….what did you do about it? Pitfalls & Issues • Language charted suggests a negative attitude – stubborn, looney, etc • Charting is wishy-washy – “Appears to be…” • Charting ahead of time and not actually performing the task Pitfalls & Issues • Staffing problems recorded in record – “We don’t have enough rad techs” • Staff conflicts recorded in the record – “Doctor is wrong” • Erasable ink used in the record • Documentation suggesting that the patient’s safety was at risk – “Almost caused perforation” • Wrong patient was named in the record WHAT NOT TO SAY: • “We are so short staffed, we are all working ourselves to death.” • “This hospital is full of patients with infection.” • “I am so tired.” • “If I were patient, I would look for another doctor.” • “Dr. ______ is terrible at catching breast cancer.” What to Look Out For • Proper patient identification • Patient abuse or neglect (real or perceived) • Failure to properly use equipment (i.e.monitors) • Failure to properly supervise personnel – If there are complaints about personnel, go up your chain ADVERSE OCCURRENCES • Complete Variance Report for anything out of ordinary (falls, equipment malfunction, injuries, etc.) • Call Risk Management for guidance, if necessary • Chart Facts ONLY • Don’t hypothesize or blame • Don’t state “error” made • Don’t indicate Variance Report was Completed • Don’t include Variance Report in Chart Bad Documentation • • • • • Time gaps, Event gaps, Illegibility, Questionable wording, inconsistencies (sudden break in pattern of reporting) Good Documentation • Timely, • Detailed, • Reflects a patient’s reactions and/or understanding of information and situation, • Documents presence of staff and physicians Pitfalls & Issues • Narrative charting: – Provides basis to go back years after the fact and know what they meant when they wrote the notes in the chart – Gives the attorney much more to go on when defending a case What charting says about you • Tells the jury: – About our competence – About our professionalism – About our respect for the patients and their families, – About our relationship with our colleagues on the team – About our degree of compliance with the policies and procedures Jury Issues • Juries rely heavily on charting • Chart is the most reliable source of information to determine what happened • If a provider charts properly, the chances of winning a lawsuit is much better Plaintiff’s attorney • A Plaintiff’s attorney best case scenario is when a provider charts with the mindset of criticizing others or using the chart as a medium for making disparaging or hurtful remarks regarding the institution and its policies. What’s Enough? • How can we distinguish between adequate and inadequate documentation? • How can we be sure that we addressed all aspects of our interventions in our documentation in any given situation? Purposes of documentation • To furnish authoritative information on patient care • To help verify quality of care • To assist in the coordination of care • To ensure continuity of care • To seek reimbursements Purposes of Documentation • reflect the fundamental values of: – Authenticity – Quality – Accountability – Responsibility – Professionalism Purposes of Documentation • To comply with regulations of the government and accrediting organizations • To provide evidence in the court of law • To generate data for research Problems Caused • Incomplete documentation can negate the purpose of documentation • Quality of care cannot be evaluated • Reimbursements may be rejected • The document cannot stand as sound evidence in the court of law • Authenticity will be compromised • Data generation will be inadequate • Continuity of care may be broken, and • Coordination of care may not be ensured. Examples • “ate lunch well” vs. “ate 50% lunch ” • “called results to MD” vs. “called CBC, chem 7 results of 1600 to MD” Six Servants • • • • • • When What Where Who Why how Examples • Entry No. 1 – 6/6/00 0900 IV heplock started in right hand...........CParker, RN • Does it answer all 6 “Servants”? Examples • When we invoke the six honest servants, entry no. 1 will provide answers to when, what, where, and who – but not to the remaining two questions, why and how. Examples • Entry No. 2 – 6/6/00 0900 IV heplock started in right hand using 20 G cathlon, and start kit per telemetry protocol....................CParker, RN Examples • Entry No.2 will provide answers to the six questions as follows: • When ..... 6/6/00 0900 What ..... IV heplock started Where ..... in right hand Who ..... CParker, RN Why ..... per telemetry protocol How ..... using 20 G cathlon, and start kit Examples • Entry No. 3 • 6/6/00 0600 foley catheter inserted .........CParker, RN • Entry No. 4 6/6/00 0630 ate 60% breakfast ..............CParker, RN Examples • The above entries no. 3 and 4 have the answers to when, what, and who • Now consider the following entries no. 5 and 6 to replace the above two entries no. 3 and 4 Examples • Entry No. 5 • 6/7/00 0600 16 Fr foley catheter inserted urethrally by using sterile technique per MD order successfully. The patient tolerated the procedure without acute distress. Clear yellow urine return noted. ........CParker, RN Examples • Entry No. 6 • 6/7/00 0630 Pt. sitting in chair. Pt. scheduled for EEG, Early 2g sodium diet breakfast served. Ate 60% by self feed. Swallowing without difficulty......CParker,RN Examples • In entry no. 5, the answers are: When ......... 6/7/00 0600 What ......... 16 Fr foley catheter inserted Where ........ urethrally How ......... by using sterile technique successfully Why ......... per MD order Who ......... ........CParker, RN Examples • In entry no. 6 the answers to all the six questions are: • When ........ 7/30/99 0630 Where ........ Pt. sitting in the chair What ........... Early 2g sodium diet breakfast served. Ate 60% Why .......... Pt. scheduled for EEG How .......... by self feed. Swallowing without difficulty Who ................CParker, RN Nursing Home case • Patient developed infection in sinuses • 3/31: Doctor examined • 4/1, 7:15 p.m. – “Resident L side of face and cheek very swollen. Resident complains of mouth hurting” – Calls doctor • Rocephin 1 gram IM now, then start PVK PO QID x7 days; consult dentist monday • 4/1, 1:30 a.m. – No distress noted • 4/2, 12 a.m. – Lying in bed Nursing Home case cont. • 4/2, 6 a.m. – Resting quietly “this shift” • 4/3, 8 p.m. – Red area on check • 4/3, 9 p.m. – Called dr. to send to ER • Emergency surgery • Patient dies 4/7 Hospital case • Child comes to ED on monday – Complains of throw up and diarrhea – “Child tolerates 16 ounces of mountain dew” – “20 ounces fluid challenge successful” • Child admitted to hospital Tuesday – – – – Pulse ox is 85% Never charted again Not sure if normal or if any complications Child dies from dehydration