The Evolving Role of the Molecular Pathologist
advertisement

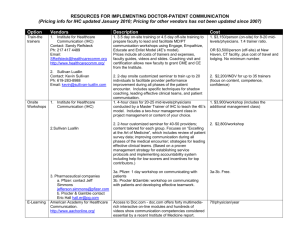
The Evolving Role of the Molecular Pathologist: Opportunities and Challenges Personalized Medicine, Companion Diagnostics CME & P.A.C.E.® Symposium at 2012 ASCO Jeffrey S. Ross, M.D. Department of Pathology and Laboratory Medicine Albany Medical College Albany, NY rossj@mail.amc.edu “A Perfect Storm” in the Healthcare Industry Driving Personalized Oncology New Customer Dynamics Pharmaceutical Industry Dynamics $ Out of pocket Informed Mergers Patent expirations New Communication Mechanisms Wireless networking Broadband Healthcare Industry Dynamics Advances in Medicine Changing Economics Generics cost shift to consumer Pricing Source: Craig Fitzgerald, Various industry sources Genomics Proteomics Imaging technologies Devices and biosensors Molecular Medicine Nanotechnologies Personalized Oncology: Key Issues • Which patients will benefit most? • Improved efficacy? • Reduced toxicity? • Cost/benefit ratio? • What time should the test(s) be performed? • What sample to test? • Tumor for Expression Profiling or Sequencing? • Blood for Germline Sequencing? • CTC? • What technique to use? • • • • Gene sequence (DNA)? Germline? Tumor Cells? Gene dosage (DNA)? Gene expression (mRNA)? Protein expression (IHC) and Proteomics? • Which algorithm or mathematic model should be used to make predictions? • Are the tests regulated by the FDA? EMA? CLIA? • Will the test(s) be reimbursed or will the patient have to pay out of pocket? • Will the added test cost reduce overall expenditures by driving better clinical outcomes? Roles for Anatomic Pathologists in Molecular Pathology and Personalized Medicine • Providing slide-based biomarker services – IHC – FISH – CISH • Preparing biopsies and resections for extraction-based biomarker services – RT-PCR – Genotyping by traditional sequencing techniques – Next Generation Sequencing Comparison of Molecular Pathology Test Platforms (1) IHC FISH CISH mRNA by RTPCR or Microarray DNA Sequencing Traditional DNA Sequencing NGS Starting Material FFPE FFPE FFPE FFPE PPFE Slide Based/Morphology Driven Requires Enrichment Yes Yes No No No No No On occasion On occasion On occasion Impact of Sample Storage/Processing High Low High Low Low Bio-informatics Expertise Requirement Potential for False Discovery Low Low Moderate Moderate High Low Low High Low Low Comparison of Molecular Pathology Test Platforms (2) IHC FISH CISH mRNA by RTPCR or Microarray DNA Sequencing Traditional DNA Sequencing NGS Prediction of Response to Cytotoxic Therapies Not established Not in current routine clinical practice Not In use in some established practices Not in current routine clinical practice In use in some practices Pending Prediction of Therapy Toxicity Not established Not in current routine clinical practice Not In use in some established practices Not in current routine clinical practice In use in some practices Pending Cost Low Higher Moderate for each assay. High for multiple assays on same sample. High High Pathologist Roles in Preparing Clinical Samples for mRNA Profiling and DNA Genotyping/NGS • Selecting the best tissue block when multiple blocks are available – Highest percentage of malignant cells – Selecting viable areas and avoiding necrosis and wound healing/severe inflammation • Recommending or performing sample enrichment when necessary Small Samples and FNAs • A FFPE section with a 4 X 4 mm minimum surface area with minimum of 40 micron thickness measurement is recommended • For FNAs – Sample is pun into a cell pellet and then converted to an FFPE tissue section – Enrichment by macrodissection rarely possible • Local IHC Procedures – Local pathologists should be discouraged from performing excessive numbers of immunostains that deplete the small amounts of tissue needed for RNA/DNA analysis • Critical importance for NSCLC biopsies • Limit immunostains for the squamous vs non-squamous deision Selected Common Examples of Slide Based Molecular Pathology for Solid Tumors • Breast Cancer – ER and PR by IHC – HER2 by IHC and FISH/CISH • NSCLC – – – – SCC vs Adenocarcinoma ALK IHC Status EGFR IHC in SCC for cetuximab ERCC1 for platinin resistance • CRC – Mis-match Repair (MSI) IHC for hMLH1, hMSH2, hMSH6 Improving ER Testing Open Issues • Can IHC be standardized? • Do we want simple positive or negative results only? • Can mRNA testing select the best hormonal therapy options? • How do we predict tamoxifen resistance in ER IHC+ tumors? • Can we “personalize” hormonal therapy The ASCO-CAP 2010 Guidelines for Hormone Receptor IHC Testing • Did not require IHC staining intensity in slide scoring • Focused on pre-analytic issues • Pre-analytic guidelines differ from HER2 guidelines (72 vs 48 hrs max fixation) • CAP Certification + Proficiency testing required • Did not establish a cut-off staining percentage for ER or PR positive status ER mRNA Testing*: Concordance Between IHC Status and mRNA Levels Relative ER mRNA Expression 25 20 15 10 5 0 + + ++ + ++ ++ + ++ ++ + ++ ++ + ++ ++ + - - - - - - - - - - - - - - - - - - - + - + - IHC > 20% ER + IHC ER - ER Status by IHC on Core Needle Biopsies * Measured by either RT-PCR (eg Oncotype Dx) or by Microarray (eg TargetPrint) HER-2 Testing Is CISH the “Kish of Death” for FISH and IHC? • Is IHC still the international method of choice for screening with 2+ cases triaged to FISH? • Will primary FISH testing ever become the standard? • Will mRNA detection gain in popularity? • Will the recently approved CISH (SISH) assay become the preferred method? • Has the ToGA Trial and Gastic/GEJ trastuzumab approvals changed how HER2 testing is done? • Will trastuzumab-DM1 and pertuzimab require HER2+ testing prior to use? The ASCO-CAP Guidelines for HER2 Testing* Key Issues - 20% of testing in the field incorrect - Required higher thresholds for HER2 positive status - 10% to 30% IHC 3+ required - FISH ratio increased from 2.0 to 2.2 - Serious concerns for patients who are HER2 positive by trastuzumab package insert guidelines but not positive by ASCO-CAP criteria not receiving anti-HER2 therapy - Criteria for HER2 positive differ from the gastric/GEJ approvals - Some laboratories no longer use the ASCO-CAP guidelines and have reverted to the package insert guidelines * Wolff AC, Hammond ME, Schwartz JN, et al. American Society of Clinical Oncology/College of American Pathologists Guideline Recommendations for Human Epidermal Growth Factor Receptor 2 Testing in Breast ancer. J Clin Oncol. 2006 Dec 11; IHC: Positive Control on Same Slide with Sample from Each New Patient It has been estimated that 3-4% of all US HER2 testing is falsely negative. HER2 Gene Copy Number Alteration Validation Increased HER2 gene copies detected by NGS HER2 FISH Positive Breast Invasive Duct Carcinoma Demonstrating High HER2 Copy Number ERBB2 RARA HER2 Protein 3+ Expression by IHC Chromogenic In Situ Hybridization Overall FISH/CISH Concordance = 98% NOT AMPLIFIED: 2 SIGNALS PER NUCLEUS HIGHLY AMPLIFIED DETAIL CISH • Chromogenic ISH • Light microscope ready • All the advantages of the DNA target in paraffin sections, but does not require fluorescent detection • FDA approval 7/2/08 Emerging HER2 Tests mRNA Oncotype Dx™ Genomic Health Redwood City, CA 2005 Not Approved On the market RT-PCR (FFPE) RNA mRNA TargetPrint Agendia Amsterdam, NE 2008 Not Approved On the market Agilent Array (Fresh tissue) RNA HER2 Gene Mutation Testing Foundation Medicine Cambridge, MA 2010 Not Approved Homebrews Hybrid Capture Sequencing (FFPE) DNA Centralized in commercial and academic labs Centralized at company headquarters Same Others Next-Gen Sequencing Di-merization HERmark™ Monogram Biosciences/USLabs/LCA South San Francisco, CA 2008 Not Approved On the market VeraTag™ Capillary electrophoresis (FFPE) Protein dimers Decentralized in clinical and commercial labs ELISA Serum HER2 Advia Centaur™ Siemens Healthcare Diagnostics Deerfield, IL 2002 Approved (PMA) On the market Sandwich Immunoassay (serum) Protein (serum) Decentralized in clinical and commercial labs CTC Based Assays Veridex OncoVista Others 2004 Not Approved On the market DNA RNA Centralized and decentralized FISH RT-PCR (whole blood) Squamous vs Non-Squamous (Adenocarcinoma) in NSCLC • At least 75% of cases can be resolved on H & E • IHC to decide Squamous vs Non-Squamous consumes vital tissue reserves for clinical trial biomarkers • Over-use of IHC markers must be discouraged • Adenocarcinoma – TTF-1 (Best), Napsin, PE-10 • Squamous Carcinoma – P63 (Best), CK5/6, 34βe12 – Desmocolin-3 (Need More Testing) • Cocktails – Nuclear/Cytoplasmic Antibodies – Adenocarcinoma – TTF-1/Napsin – Squamous – P63/CK5/6 EML4-ALK Rearrangement in NSCLC • Crizotinib – Oral ALK4 receptor kinase inhibitor – Phase I Trial on NSCLC patients with EML4-ALK rearrangement • “echinoderm microtubule-associated protein-like 4” – “anaplastic lymphoma kinase” – 10/19 (53%) had a partial response • Seen in 5-13% of adenocarcinomas • More common in non-smokers • All ELM4-ALK Positive NSCLC are Negative for EGFR and KRAS mutations • ELM4-ALK translocation can be detected by FISH or NGS • ALK IHC (Cell Signaling Ab) being developed as a CDx for crizotinib Shaw et al. J Clin Oncol. 27;2009:4247-4253. EGFR IHC Testing in Squamous Cell NSCLC • May be developed as a CDx for selection of NSCLC SCC for treatment with cetuximab • ECCO/ESMO data indicated that “H Score” IHC scoring must be used and tumors must have a score > 200 • EGFR IHC not currently required for HNSCC case selection for cetuximab use ERCC1 Testing in NSCLC • ERCC1 as a predictive marker in cisplatin-based adjuvant chemotherapy in resected NSCLC has been suggested in large, retrospective analyses • Confirmation needed in large prospective studies • Data mainly for cis-platinin, data for carbo-platinin lacking • Hypothesis that low/negative ERCC1 IHC expression is predictive of platinumbased chemotherapy-sensitivity has not yet been fully validated • ERCC1 by RT-PCR efficacy varies due to the quality of material • IHC may vary on inter-observer variability and the target lesion chosen for examination • Blood-based SNPs methods determining ERCC1 polymorphisms holds promise • The role of ERCC1 in NSCLC patient-tailored chemotherapy although far from being firmly established may possibly prove to play an important role in tailored chemotherapy for NSCLC Detecting MSI in CRC with IHC • Routine use in many CRC treatment institutions • Mis-match Repair Defective CRC defined as Loss of expression of 2 or more mis-match repair enzymes (MLH1, MSH2, MSH6, others) • Associated with improved prognosis and potential for reduced treatment intensity stage for stage • IHC results also may indicate HNPCC Selected Common Examples of mRNA Profiling for Solid Tumors • Cancer of Unknown Primary Origin • Non-Hodgkin’s Lymphoma • Breast Cancer – Molecular Portraits – Tumor Grading – Predicting prognosis and guiding management • Pharmacogenomics Technology Platforms For High Throughput Analysis Of mRNA Expression cDNA arrays Oligonucleotide arrays Multiplex RT-PCR Probe length Hundreds to thousands of base long cDNA 20-75 base oligonucleotides 15-30 base PCR primers Probes per array 100 –5,000 >20,000 Few hundred Probes per transcript 1-2 1- >10 1 Examples of sources Clontech, Agilent, Incyte, core laboratories Affymetrix, Amersham, Mergen, Agilent, core laboratories Qiagen, Applied Biosystems, Roche Molecular Systems, Genomic Health Detection system Chemiluminescence Chemiluminescence Chemiluminescence Radioisotope Gel electrophoresis Challenges that Face Genomic Microarrays • Over-fitting The Data • Discovery Research without a hypothesis • Initial excitement followed by failure to reproduce the results • Test results may vary with the extent of the disease • Lack of Currently Approved Rules of Evidence • No standardized approach to data validation • Multivariate Analysis finds independent significance but association with disease outcome was actually due to chance • “Too many genes, not enough patients” Microarray Classification of Non-Hodgkin’s Lymphoma Staudt. Cancer Cell Vol. 2, No. 5, 11/02: 363 - 366 Site of Origin for Metastatic Adenocarcinoma Dennis et al Cancer Res 2002;62:5999-6005 Expression Profiles of 61 Genes by SAGE Established Tumor Markers by RTPCR in Common Adenocarcinomas Molecular Portrait of Breast Cancers Basal–like HER-2 “Normal Luminal B Luminal A Sørlie et al. Proc Natl Acad Sci U S A. 2001 Sep 11;98(19):10869-10874. Molecular Grading of Breast Cancer • Gene expression profiling data indicates that there are 2 molecular grades of breast cancer • Histologic Grade 2 cases redistribute into Molecular Grades 1 and 2 • Molecular grading has outperformed histologic grading in multivariate analysis of traditional prognostic factors including ER/PR and HER2 status • The Genomic Grade IndexTM has been commercialized by Ipsogen, Inc. Patterns of expression of grade-related genes and their association with histologic grade (HG) and relapse-free survival. GGI score of each tumor is plotted below the corresponding column. Relapse-free survival times in years are indicated below the GGI scores. Sotiriou C, et al.. Gene expression profiling in breast cancer: understanding the molecular basis of histologic grade to improve prognosis. J Natl Cancer Inst. 2006 Feb 15;98(4):262-72. Multigene Classifiers and Predictors of Breast Cancer Clinical Outcome* Classification Test Sorlie-Perou Classifier Grading ARUP Bioclassifier Prognosis Sotiriou Molecular Grading Mammostrat® Prognosis and Response to Therapy eXagenBC Rotterdam Signature Oncotype Dx® Two-Gene Ratio MammaPrint® Roche AmpliChip® P450 Manufacturer Not In Development Ipsogen, Inc Commercialized Applied Genomics Exagen Diagnostics Veridex Genomic Health AviaraDx/Quest Agendia BV Cytochrome P450 CYP2D6 Roche Diagnostics/Merck Medco/Lab Corp Method Microarray RT-PCR Microarray IHC FISH Microarray RT-PCR RT-PCR Microarray Microarray Platform Stanford University Agilent array Light Cycler Affymetrix U-133 Immunoperoxidas 3 probe multiAffymetrix U-133 Taqman e color FISH assay Manual scoring (Applied Biosystems Taqman Rosetta Roche Inpharmatics/Agile AmpliChip® nt Custom Array (Affymetrix Platform) Custom cDNA Sample Conditions Fresh/Frozen (Roche Diagnostic Systems) (Applied Biosystems) FFPE Fresh/Frozen FFPE FFPE Fresh/Frozen FFPE FFPE Fresh/Frozen Fresh/Frozen Preserved mRNA Unknown Resections Resections Core Biopsies Resections Core Biopsies Resections Resections Core Biopsies Resections Resections Resections Number of Genes 427 55 97 5 3 76 21 6 70 1 Indication ER Positive All cases on invasive ER Positive breast cancer LN Negative ER Positive ER Positive ER Positive ER Negative ER Negative LN Negative LN Positive Staring Material Requirement Resections All cases on invasive breast cancer ER Negative LN Negative ER ER Positive and ER Positive positive or Negative negative LN Positive and LN Negative Negative LN Negative LN Negative Stand Alone Prognostic Role Established Partially Yes Yes No No Yes Yes No Yes No Guide to Specific No Therapy No No Yes Tamoxifen No Possible (Tamoxifen) Yes Tamoxifen Yes Tamoxifen No Yes Tamoxifen CypChip Commercial Status In development In Development In Development In development FDA Status Unknown Submitted for Not submitted 510(k) Clearance On the market On the market Centralized Testing Approved (510k) Approved Cost Unknown Unknown - On the market In Development In Development Centralized Testing Exepmt Submitted for Not submitted 510k clearance (Home brew (4/07) assay) Billed as 5 88342 Billed as a Unknown Global CPT codes multiplex FISH (approximately test. ($700-1,000 $600) expected reimbursement) Adjuvant CMF On the market Centralized Testing Exempt >$4,000 Not submitted >$1,500 >$4,000 Approximately $350 *Ross, JS, Hatzis C, Symmans WF, Pusztai L, Hortobagyi GN. Commericalized multi-gene predictors of clinical outcome in breast cancer. Oncologist. 2008;13:477-493. Comparison of Oncotype DxTM and MammaprintTM Oncotype Dx MammaPrint Provider/Cost Genomic Health, Inc. $3,647 Agendia, BRV $4,166 Starting Material FFPE Fresh mRNA and FFPE Number of Genes 21 70 Rank of Importance of Pathways Assessed 1 Proliferation 1 Proliferation 2 ER 3 HER2 2 ER 3 HER2 Current Indication Node-Negative ER-Positive Node Negative ER-Positive/Negative Eligible Patient Age Older patients Young and Old Patients Prognostic vs Predictive Prognostic and Predictive Prognostic and Predictive Outcome Prediction Continuous Dichotomous ASCO Biomarkers Guidelines Status Recommended for use Under Investigation Cost Effectiveness Validation Cost-effective in one published study Not reported FDA Status Not submitted Cleared at 510k level Tissue Requirements for DNA Sequencing • DNA yield from FNAs may not always be satisfactory – Needle core biopsies preferred whenever possible – DNA is typically extracted from FFPE cellblocks from fluids and FNAs • Genotyping DNA in routine practice – EGFR for gefitinib/erlotinib in NSCLC – KRAS for cetuximab in CRC – BRAF for metastatic melanoma • NGS can be performed on FFPE samples – Currently requires 50 ng of DNA (approximately 10,000 cells) – Likely will require less (? 20 ng) as technology improves – Enrichment rarely needed for samples with <20% tumoral DNA present on clinical sample Traditional DNA Sequencing Methods Ross J, Cronin M. Am J Clin Pathol, 2010. Next Generation Sequencing • The Human Genome sequence using original Sanger sequencing techniques was completed in 12 years at a cost of $ 3 Billion • The rate-limiting step in Sanger sequencing is the need to separate randomly terminated DNA polymers by gel electrophoresis • NGS bypasses this by physically arraying DNA molecules on solid surfaces and determining the DNA sequence in situ enabled by the development of reversible (chemically or enzymatically) DNA chain terminators • The DNA sequence is determined by measuring which bases are added into an elongating DNA chain, physically anchored to a glass slide or array of beads • In the next few years, the cost of NGS will continue to decrease rapidly and a clinically relevant gene sequence for a tumor may approach $1,000 cost range with turn-around time of only several days Comparison of Traditional (Sanger) Sequencing and NGS Ross J, Cronin M. Am J Clin Pathol, 2010. Next Generation DNA Sequencing Platforms Ross J, Cronin M. Am J Clin Pathol, 2010. EGFR Mutation Testing in NSCLC • • • • • Primary used to predict response to anti-EGFR tyrosine kinase small molecule drugs (erlotinib/gefitinib) No standardized test with multiple methods of gene sequencing in clinical use Currently, standard of care for EGFR-mutated lung cancer patients should be first-line TKI, using either gefitinib or erlotinib EGFR mutation correlates with gene amplification Does not predict the response to anti-EGFR antibodies (cetuximab, panitumumab) EGFR Activating Mutation – NSCLC • • • • Mutation: EGFR_c.2573T>G_p.L858R Freq=32%, depth=53 79 year old white female FNA of lung mass: NSCLC FNA sample cytocentrifuged and converted to an FFPE tissue block. Very small numbers of viable tumor cells. Extensively necrotic. KRAS Mutation Testing in CRC Issues • KRAS mutated in 27-53% of CRC • Mutated KRAS identifies 50% of cetuximab/panitumumab resistant CRC • RT-PCR method more sensitive than direct sequencing • ASCO Opinion - All patients with metastatic colorectal carcinoma who are candidates for anti-EGFR antibody therapy should have their tumor tested for KRAS mutations in a CLIA-accredited laboratory - If KRAS mutation in codon 12 or 13 is detected, then patients with metastatic colorectal carcinoma should not receive anti-EGFR antibody therapy as part of their treatment Pivotal KRAS Data from Randomized Clinical Trials Ross J. Arch Pathol Lab Med, 2011 Established Techniques for KRAS Genotyping Ross J. Arch Pathol Lab Med, 2011 Biomarkers Linked to Cetuximab/Panitumumab Resistance in CRC Ross J. Biomarkers in Med., 2011 KRAS Mutation – CRC • • • • • Mutation: KRAS_c.35G>T_p.G12V Freq=30%, depth=283 52 year old white male KRASG12V mutation by “hot-spot” genotyping at Commercial Laboratory pT3 pN2 pMx CRC Classic CRC with origin from mucosal surface at lower right Novel ALK Fusion in CRC Detected by NGS A 5,194,955-bp tandem duplication generates an in-frame C2orf44-ALK gene fusion The RNA sequence of the C2orf44-ALK gene fusion shows aberrant splicing pT4pN1pM1 Mucinous Adenocarcinoma associated with a serrated sessile polyp RNA sequencing shows an 89.8-fold increase in expression of ALK beginning at exon 20 relative to exons 1–19. Lipson et al. Nature Med, Feb, 2012 Vemurafenib in BRAF Mutated Melanoma • Vemurafenib inhibits V600E mutated BRAF tyrosine kinase • BRAF mutation occurs in 50-60% of melanomas • Vemurafenib specifically blocks the activity of the mutated but not wild-type BRAF mutation and causes apoptosis • Phase I escalating dose study of 16 BRAF V600E mutated metastatic melanoma patients presented at ASCO 2009 • Of the 16 treated melanoma patients, 9 had partial responses , 6 had stable disease and one had progressive disease as their best responses. • None of 5 non-mutated melanoma patients also treated with vemurafenib had any responses. • ASCO ‘10: 1/29 BRAF-mutated CRC cases showed a partial response to vemurafenib BRAF V600K Mutation – Metastatic MM • • • • • Mutation: BRAF_c.1798_1799GT>AA_p.V600K Freq=10%, depth=416 77 year old white male Thick melanoma of back Multiple posterior cervical lymph nodes positive for metastatic melanoma Metastatic Melanoma to a cervical lymph node Molecular Pathology for Clinical Management for Major Solid Tumors Breast Cancer NSCLC CRC Prostate Cancer Metastatic Melanoma IHC ER and PR HER2 Ki-67 IHC4 and Mammastrat Squamous vs Adenoca Alk inhibitors pending (crizotinib) ERCC1 controversial EGFR for erbitux in SCC pending EGFR for erbitux and panitumumab MSI and HNPCC PIN4 (racemase) for diagnosis None FISH/CISH HER2 Alk inhibitors (crizotinib) None TMPRSS:ERG fusions Melanoma diagnosis mRNA Profiling Oncotype MammaPrint None Oncotype Colon ColoPrint None None Traditional Genotyping None EGFR inhibitors (erlotinib) KRAS for erbitux/panitumum ab None BRAF for vemurafenib NGS HER2 Hormonal Rx Targeted Rx for TNBC pending EGFR TKI EML4:ALK Other targets (RET-kif5B) Other targets TMPRSS:ERG fusions Other targets BRAF for vemurafenib Other targets Targeted Therapies for Cancer Molecular profiling is driving many new targeted cancer therapeutics • ~500 compounds hitting ~140 targets in development • Growing number of newly identified potential targets Subset of analyzed targets listed; data from BioCentury Online Intelligence Database