Nutrition for Oral and Dental Health
advertisement

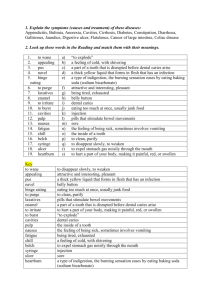
Nutrition for Oral and Dental Health Oral Health Diet and nutrition play a key role in —Tooth development —Gingival and oral tissue integrity —Bone strength —Prevention and management of diseases of the oral cavity Effects of Nutrient Deficiencies on Tooth Development Dental and Oral Health Teeth are made from protein matrix that is mineralized with collagen (requiring vitamin C), calcium, and phosphorus (requiring vitamins D and A) Anatomy of a Tooth Dental Caries Infectious disease of teeth in which organic acid metabolites lead to gradual demineralization of enamel; proteolytic destruction of tooth structure Any tooth surface can be affected. The Decay Process Plaque formation: sticky mix of microorganisms, protein, polysaccharides Bacteria metabolizing fermentable carbohydrate produce acid Acid production: oral pH<5.5 allows tooth demineralization Saliva function: rinses away food; neutralizes acid; promotes remineralization Caries patterns:pattern depends on cause Early Childhood Caries Also called “baby bottle tooth decay” Nursing bottle caries—putting baby to bed with a bottle of sweetened liquid (juice, Kool-Aid, etc.) Front teeth rapidly develop caries Common among Native Americans Wean children before age 2 from bottle Early Childhood Caries (From Swartz MH. Textbook of Physical Diagnosis, History, and Examination, 3rd ed. Philadelphia: W.B. Saunders, 1998.) Dental Caries—cont’d Streptococcus mutans—most common bacteria involved Fermentable Carbohydrate Time Drop in salivary pH to below 5.5 Dental Caries—cont’d Cariogenicity of foods Frequency of consumption of fermentable Carbohydrate Food form—slowly dissolving Food combinations Nutrient composition of food/beverages Timing (end of meal) Medical Sequelae of Dental Caries Bacteria from tooth decay can enter bloodstream and inoculate heart valves, cause bacterial endocarditis Oral-pharyngeal secretions inoculated with bacteria can cause aspiration pneumonia Fluoride Primary anticaries agent Water fluoridation Fluoridated toothpastes Oral rinses Dentrifices Beverages made with fluoridated water Recommendations for Fluoride Supplementation (Data from American Dietetic Association: Position of ADA: The impact of fluoride on dental health. J. Am Diet Assoc. 94:1428, 1994.) * Milligrams of supplemental fluoride recommended according to fluoride concentration in drinking water. Cariogenic vs. Cariostatic Cariogenic: containing fermentable carbohydrates that can cause a decrease in salivary pH to <5.5 and demineralization when in contact with microorganisms in the mouth; promoting caries development Cariostatic: not metabolized by microorganisms in plaque to cause a drop in salivary pH to <5.5 Cariogenic Foods Promote formation of caries Fermentable carbohydrates, those that can be broken down by salivary amylase Result in lower mouth pH Include crackers, chips, pretzels, cereals, breads, fruits, sugars, sweets, desserts Cariostatic Foods Foods that do not contribute to decay Do not cause a drop in salivary pH Includes protein foods, eggs, fish, meat and poultry; most vegetables, fats, sugarless gums Anticariogenic Foods Prevent plaque from recognizing an acidogenic food when it is eaten first May increase salivation or have antimicrobial activity Includes xylitol (sweetener in sugarless gum) and cheeses Other Factors that Affect Diet Carogenicity Consistency: Liquids are cleared quickly while sticky foods remain on the teeth Meal frequency: frequent meals and snacks increase duration of exposure Food composition Food form: liquid, solid, slowly dissolving Sequence of eating: cheese or milk at the end of the meal decrease the cariogenicity of the meal Caries Prevention Guidelines Periodontal Disease Inflammation of the gingiva with destruction of the tooth attachment apparatus Gingivitis—early form Nutritional care involves increasing vitamin C, folate, and zinc Tooth Loss and Dentures Tooth loss—denture placement Food selections change Saliva production decreases Reduced chewing ability Lower calorie and nutrient intake occurs for many Simple nutrition counseling; Food Guide Pyramid, etc. Oral Manifestations of Disease Stomatitis: inflammation of oral mucosa Candidiasis and herpes simplex: fungal and viral infections which can affect mouth and esophagus causing pain and dysphagia Photo: http://webpages.marshall.edu/~gain/bactnote/Image9.gif Oral Manifestations of Disease Xerostomia: Dry mouth Periodontal disease Kaposi’s sarcoma—lesions in mouth and esophagus; associated with AIDS Kaposi’s Sarcoma in AIDS MNT for Mouth Pain/ Oral Infections Avoid acidic and spicy foods Offer soft, cold, nutrient dense foods such as canned fruit, ice cream, yogurt, cottage cheese Try oral supplements Use PEG or NG feeding if oral supplementation is unsuccessful For xerostomia, try artificial salivas, citrus beverages, sugar free candies or gums Medications That May Cause Xerostomia Dental Health Affects Nutrition Tooth loss may affect ability to chew (relationship between loss of teeth and reduced intake of fruits and vegetables Dentures are often ill-fitting (especially common after weight loss); problem foods include fresh fruits and vegetables, chewy and crusty breads and chewy meat like steak Interventions Obtain a dental consult: if dentures are missing, find them. If they are loose, replace or reline them Modify diet consistency: mechanical soft, ground, pureed Use least restrictive diet possible; individualize; mix consistencies if appropriate MNT for Wired or Broken Jaw Provide pureed, strained, or blenderized foods as appropriate Encourage nutrient-dense foods such as blenderized casseroles Recommend small, frequent meals with oral supplements such as milkshakes, Instant Breakfast, medical nutritionals Use liquid vitamin supplement if necessary Recommend patient weigh self to monitor weight status Dysphagia = difficulty swallowing Mechanical causes – Trauma to esophagus with scar tissue – Inelasticity due to repeated inflammation – Tumor of esophagus – Aneurism of aorta Dysphagia = difficulty swallowing Neuromuscular causes CVA, brain tumors Head injury Parkinson’s disease, MS, ALS Achalasia (cardiospasm) Spinal cord injury Dysphagia Oral phase problems Pocketing food Drinking from cup or straw Drooling Pharyngeal phase Gagging Choking Nasal regurgitation Esophageal phase Obstruction Symptoms of Dysphagia Drooling, choking, coughing during or after meals Inability to suck from a straw Holding pockets of food in cheeks (pt may be unaware) Absent gag reflex Chronic upper respiratory infections Gargly voice quality or moist cough after eating Diagnosis of Dysphagia Nerve assessment X-rays Fluoroscopic swallow study: barium swallow/cookie swallow Measurement of esophageal sphincter pressure and peristalsis Aspiration Inhalation of food, liquid into lungs Can cause aspiration pneumonia Appears to be dose-dependent A major cause of aspiration pneumonia is thought to be aspiration of oropharyngeal secretions, particularly if contaminated by bacteria MNT for Dysphagia (National Dysphagia Diet) Intervention depends on severity of deficit Mealtime supervision, cueing Thickened liquids: thin » nectarlike » honeylike » spoon thick Altered consistency: – Level 1: pureed – Level 2: mechanically altered – Level 3: advanced Thickened Liquids MNT for Dysphagia In severe cases, patient may be made NPO and enteral feedings initiated National Dysphagia Diet NDD diets are more restrictive than dental consistency diets; may wish to use more liberal diet for edentulous patients Developed by consensus committee; no evidence as yet that it is effective in preventing aspiration Provides much-needed standardization NDD: Level 1 -- Pureed Foods are totally pureed; no coarse textures or lumps of any kind Breads must be pureed or pregelled, slurried through entire product thickness Cereals should be homogeneous or “puddinglike;” such as cream of wheat, cream of rice, farina; avoid oatmeal Fruits pureed without pulp, seeds, skins; juice should be thickened to desired consistency Soups should be pureed, strained, and thickened to desired consistency Mashed potatoes and pureed pasta are main starches NDD Level 2 – Mechanically Altered Foods are soft-textured and moist so they easily form a bolus Breads must be slurried, pre-gelled through entire thickness, but well-moistened pancakes are allowed Cooked cereals may have some textures and some try, well-moistened cereals allowed Soft canned or cooked fruits, no seeds or skins Ground or minced tender meats with no larger than ¼ inch pieces, well-cooked casseroles, cottage cheese; avoid peanut butter, sandwiches, pizza Most soups Soft, well-cooked vegetables with less than ½ inch pieces; no corn, peas, fibrous varieties NDD Level 3 -- Advanced Nearly normal textures, but exclude crunchy, sticky, hard foods Foods should be bite-sized and moist Moist, tender meats and casseroles with small pieces Most vegetables except corn Potatoes, rice, stuffing allowed All beverages if they meet ordered consistency Moist breads allowed; no tough, crusty bread Most desserts allowed, no nuts, seeds, pineapple, coconut, dried fruit Strategies for Improving Acceptance Thickened liquids: commercial products can improve quality and consistency of thickened liquids Seasoning: persons with dysphagia often have dulled sense of taste. Serve seasoned foods such as spaghetti, chili, apple pie Piping and molding: pureed foods can be thickened and molded for more attractive appearance Piped and Molded Pureed Foods Dysphagia Diet Issues Patients on altered consistencies tend to eat less and often lose weight Patients on thickened liquids are at risk for dehydration Re-evaluate patients and advance diet as quickly as possible