VESTIBULAR SYSTEM
advertisement

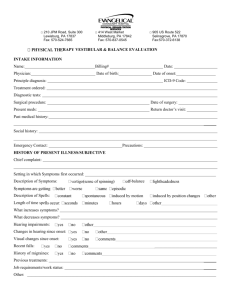
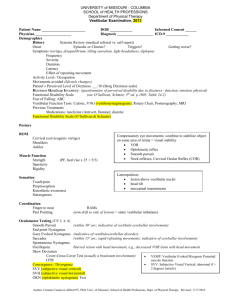
Vestibular Examination ANATOMY & FUNCTION Carmen Casanova Abbott PT, PhD Lecture Objectives ► Discuss vestibular structure as it relates to vestibular function when examining a dizzy patient. ► Discuss signs and symptoms associated with vestibular disorders ► Differentiate between peripheral and central vestibular pathology ► Discuss components of a physical therapy vestibular examination. Vestibular System Function ► Provides information concerning gravity, rotation and acceleration ► Serves as a reference for the somatosensory & visual systems ► Contributes to integration of arousal, conscious awareness of the body via connections with vestibular cortex, thalamus and reticular formation ► Allows for: gaze & postural stability sense of orientation detection of linear & angular acceleration Vestibular Anatomy ► Peripheral sensory apparatus detects & relays information about head angular & linear velocity to central processing system orients the head with respect to gravity ► Central processing system processes information in conjunction with other sensory inputs for position and movement of head in space ► Motor output system generates compensatory eye movements and compensatory body movements during head & postural adjustments Peripheral Apparatus ► Membranous Labyrinth Semicircular canals (SSC) Otolith organs Netter ‘97 Semicircular Canals ► Angular acceleration ► Ampulla contains sensory epithelium SSC Coplanar Pairing ► Spatial arrangement of the 6 SSC cause 3 coplanar pairings R & L lateral, L anterior and R posterior; l posterior & R anterior; R & L horizontal ► Allows for a Push-Pull arrangement of the two sides (e.g., as head turns right, right SSC will increase firing rate & the left SSC will decrease firing rate) ► Advantages sensory redundancy common mode rejection/noise Inhibitory Cutoff ► Depolarization of the ipsilateral hair cells occurs during angular head movements ► Hyperpolarization of contralateral hair cells occurs at the same time ► Hair cells are only able to hyperpolarize to what they were at rest = cut off of inhibitory influences from the movement going in the opposite direction even if the ipsilateral hair cells continue to spike higher firing rates Purves 2001 Otoliths ► Utricle and saccule ► Otolith sensory structures Maculae Otolithic membrane Otoconia ► Movement of gel membrane & otoconia cause a shearing action to occur over the hair cells → sensitivity of otoliths Otolith Function ► Respond to: Linear head motion on acceleration Static tilt Two organs respond to respective accelerations or tilts in their respective planes ►Saccule has vertical orientation of maculae ►Utricle has horizontal orientation of maculae Bear 1996 Purves 2001. Hair Cells ►2 types: kinocilium & stereocilia ► Sensory structures for the peripheral end organs (maculae and ampula) ► Hyperpolarized or depolarized depending upon the direction of deflection of the stereocilia (movement of stereocilia towards the kinocilium causes depolarization of the hair cell) ► Affect the firing rate of the primary vestibular afferents to the brainstem Bear 1996 Striola of the Macula ► Striola serves as a structural landmark ► Contains otoconia arranged in narrow trenches, dividing each otolith ► Orientation of the hair cells change over the course of the macula ► Allows otoliths to have multidirectional sensitivity Purves 2001. Principles of the Vestibular System ► Tonic firing rate ► Vestibular Ocular Reflex ► Push-pull mechanism ► Inhibitory cutoff ► Velocity storage system Ascending Pathways ► Vestibular nerve ► Vestibular nuclei ► Cerebellum ► Oculomotor complex CN 3, 4, and 6 Along with vestibulospinal reflexes coordinate head and eye movements Relay Centers ► Thalamus Connection with vestibular cortex and reticular formation → arousal and conscious awareness of body; discrimination between self movement vs. that of the environment ► Vestibular Cortex Junction of parietal and insular lobe Target for afferents along with the cerebellum ►Both process vestibular information with somatosensory and visual input Netter 1997 Tonic Firing Rate ► Vestibular nerve and vestibular nuclei have a normal resting firing rate (70-100 cycles/sec) ► Baseline firing rate present without head movement ► Tonic firing is equal in both sides; if not, a sense of motion is felt e.g., vertigo, tilt, impulsion, spinning ► Excitation and inhibition of the vestibular system can then occur from stimulation of the hair cells ► Spontaneous recovery with light Vestibular-Ocular Reflex (VOR) ► Causes eyes to move in the opposite direction to head movement ► Speed of the eye movement equals that of the head movement ► Allows objects to remain in focus during head movements Compensatory Eye Movements ► VOR ► Optokinetic reflex ► Smooth pursuit reflex, saccades, vergence ► Neck reflexes combine to stabilize object on the same area of the retina=visual stability Purves 2001. Vestibular Processing Gain ► Keeps eye still in space while head is moving ► Ratio of eye movement to head movement (equals 1) Vestibular Processing Velocity Storage Mechanism ► Perseveration of neural firing in the vestibular nerve by the brainstem after stimulation of SSC to increase time constant (10sec.) SSC respond by producing an exponentially decaying change in neural firing to sustained head movement ► Otolith & somatosensory input also drive mechanism VOR Dysfunction ► Direction of gaze will shift with the head movement ► Cause degradation of the visual image ► In severe cases, visual world will move with each head movement Oscillopsia ► Visual illusion of oscillating movement of stationary objects ► Can arise with lesions of peripheral or central vestibular systems ► Indicative of diminished VOR gain motion of images on fovea diminished visual acuity Cerebellum ► Monitors vestibular performance ► Readjusts central vestibular processing of static & dynamic postural activity ► Modulates VOR ► Provides inhibitory drive of VOR (allows for VORc) Descending Pathways ► Provide motor output from the vestibular system to: Extraocular muscles (part of VOR) Spinal cord & skeletal muscles (generate antigravity postural activity to cervical, trunk & lower extremity muscles) ► Response to changing head position with respect to gravity (righting, equilibrium responses) Vestibulospinal Reflex (VSR) ► Generates compensatory body movement to maintain head and postural stability, thereby preventing falls Netter 1997 Vestibular Dysfunction Demographics ► Vestibular disorders manifested by vertigo are a significant health problem, secondary only to low back pain ► NIH study estimates that 40% of the population over the age of 40 will experience a dizziness disorder during their lifetime Fall Demographics ► Falls will be experienced in community dwelling individuals: 28-35 % over age 65 42-49% over age 75 ► Greater than 60% will have bilateral vestibular lesion (BVL) in the <65 or >75 years of age Fall Risk Factors ≥ 4 risk factors, 78% chance of falling in an older adult ► Sedatives ► Dizziness ► Cognitive ►↑ impairment ► Palmomental reflex ► LE disability ► Foot problems ► Balance abnormalities dependence on visual cues ► Fear of falling ► Orthostatic hypotension (Tideiksaar R 1998) Other Fall Risk Factors? Aging Changes ► Progressive changes begin at age 40 Decreased number of hair cells Decreased vestibular nerve fibers ► Lead to dizziness and vertigo ► Harder to deal with competing visual and somatosensory input Fear of Falling (FOF) FOF affects willingness to participate in physical activity & exercise ► FOF occurs in an average of 30% of older adults who have not fallen ► FOF increases to an average of 60% of older adults who have fallen ► FOF is higher among women ► Prevalence of FOF is underestimated ► Greater FOF associated with lower quality of life in mental health, social & leisure pursuits ► (Legters, 2002) Falls Related Self-efficacy ► Falls Efficacy Scales (FES) better for frail indoor activities ► Activities-Specific Balance Confidence Scale (ABC) higher functioning indoor & outdoor activities > discrimination between fearful & nonfearful (Legters, 2002) Vestibular Pathophysiology ► Disorders of tone & or gain (vertigo / movement- induced vertigo) ► Vestibular nerve / nuclei give abnormal sensory information ► Tone automatically recovers in a few days; does not need visual input ► Compensation for reduced gain depends on visual images; takes month to years to complete; high speeds & accelerations may never be complete ► Nystagmus usually transient sign of vestibular lesion; movement-induced symptoms can be chronic Dizzy Patient Presentation: unexplained or new onset of symptoms ► Medical referral is indicated constant vertigo lateralpulsion facial asymmetry speech & or swallowing difficulties oculomotor dysfunction vertical nystagmus severe headaches recurrent falls unilateral hearing loss, tinnitus, fullness, ear pain Vertigo ► An asymmetrical firing of the two vestibular systems ► Gives an illusion of spinning, movement ► Indicative of any one or combination of causes (acute UVH, BPPV, brainstem lesion, vascular hypotension…) Differentiation Between Peripheral & Central Causes of Vertigo Peripheral Nausea Imbalance Hearing Loss Oscillopsia Neurologic Symptoms Compensation severe mild common mild rare rapid Central moderate severe rare severe common slow (Furman JM, Whitney SL. 2000) Peripheral Vestibular Disorders ► Vestibular Neuronitis ► Labyrinthitis ► Meniere’s ► Acoustic Neuroma ► Fistula ► Benign Paroxysmal Positional Vertigo (BPPV) Central Vestibular Disorders ► Vascular Wallenberg’s Syndrome Head Injury Cerebellar Infarct ► Postconcussive Syndrome ► Demyelinating Disease ► Congenital Degenerative Cerebellar Disease ► Signs & symptoms abnormal ocular pursuit gradual decline irregular saccades gaze end point nystagmus ataxia Objective of Clinical Exam ► Establish location & severity of lesion (central or ► Typical examination - history (hearing status) - cranial nerves - vestibular peripheral) spontaneous nystagmus (imbalance in tone) postural instability (abnormal tone & gain; proprioceptive loss) VOR gain (maintained fixation, dynamic visual acuity) head shaking (compensated UVL; not necessarily PVL) calorics pressure sensitivity (fistula) positional nystagmus (Hallpike-Dix test) hyperventilation (anxiety; acoustic neuroma) Nystagmus ► Rapid alternating movement of eyes in response to continued rotation of the body ► Primary diagnostic indicator in identifying vestibular lesions ► Physiologic nystagmus vestibular, visual, extreme lateral gaze ► Pathologic nystagmus spontaneous, positional, gaze evoked ► Labeled by the direction of the fast component ► Central vs. peripheral cause differentiated by duration Vestibular Function Tests ► Caloric test ► Rotary Chair test ► Posturography Results of Vestibular Function Tests ► Presence of complete vs. incomplete loss ► Presence of peripheral vs. central dysfunction ► Direct patient management ► Help in outcome prediction Dizziness Handicap Inventory ► Three subscales function emotion physical aspects ► Scoring Yes 4 pts. Sometimes 2 pts. No 0 pts. ► Excellent test-retest reliability Hallpike-Dix Maneuver ► Gold standard used to check for the presence of benign paroxysmal positional vertigo (BPPV) ► Nystagmus induced by this test is an objective measurement from which we can determine SSC dysfunction and assess a response to treatment Benign Paroxysmal Positional Vertigo (BPPV) ► Signs & symptoms sudden, severe attacks of vertigo precipitated by certain head positions & movements ►e.g., rolling over, neck extension, bending forward lightheadedness; nausea anxiety avoids movement direction & duration of nystagmus differentiates between BPPV & a central vestibular lesion (CVL) Benign Paroxysmal Positional Vertigo (BPPV) ►5 criteria crucial in diagnosis (Hallpike-Dix Test): torsional/linear-rotary nystagmus; reproduced by provocative positioning with affected ear down nystagmus of 1-5 sec. latency nystagmus of brief duration (5-30 sec.) reversal of nystagmus direction on returning to upright position response diminishes with repetition of maneuver (fatigability) (Massoud ’96) BPPV Cupulolithiasis ► Debris, probably fragments of otoconia from the utricle, adhere to the cupula ► Treatment Brandt-Daroff habituation exercises Semont, liberatory maneuver BPPV Canalithiasis ► Debris floating freely in the endolymph in the long arm of the posterior SSC ► Treatment Canalith repositioning maneuver (Epley) 84-90% remission rate Sleep upright one night only (more severe cases) Problems Experienced with Vestibular Loss ► Balance & gait deficits ► Head movement-induced dizziness ► Head movement-induced visual blurring (oscillopsia) ► LE dressing difficulty ► Driving deficits ► Disability related to work, social & leisure activities Systems Approach to Examination ► Examination of balance & mobility using a variety of tests & measurements to document functional abilities, determine underlying sensory, motor, & cognitive impairments contributing to functional disabilities Balance ► Can be viewed as a motor skill that emerges from the interaction of multiple systems ► These systems are organized to meet functional task goals & are constrained by the type of environment ► Balance, like any skill, can improve with practice Balance Components ► Steadiness ► Symmetry ► Dynamic stability Balance Training: Postural Biofeedback ► Postural symmetry & dynamic stability have been consistently improved by training using force platform systems Clinical Test of Sensory Interaction In Balance (CTSIB) ► Assesses pattern of sensory dependence for balance from timed stance tests during distortion of sensory environment Berg Balance Scale ► Performance -orientated balance assessment ► Interpretation: > 45/56 score highly specific (96%) for nonfallers subjects who fell most frequently were those closer to cut off ► Correlates with other balance tests Functional Gait Assessment (FGA) ► Assesses postural stability during walking ► Modified version of the Dynamic Gait Index ► Added 3 new tasks to increase challenge and sensitivity of the test to minor changes in gait ► Stronger vestibular components (head turns, narrow BOS, ambulating backwards and with eyes closed) General Therapeutic Intervention Objectives ► Changing impairments ► Improving functional performance ► Improving capacity to adapt performance to changing task & environmental demands Mechanism of Recovery: Compensation ► Results from changes in CNS rebalancing of tonic activity within vestibular nuclei (spontaneous recovery) recovery of VOR (vestibular adaptation) habituation (progressive decline in response to same stimulus) alternative strategies/substitution; in complete loss of vestibular function ► Enhanced by active movements & processing of visual, vestibular, & somatosensory stimuli Result of Early Intervention ► Gain returns quicker ► Increased function ► Decreased gait ataxia ► Decreased perception of disequilibrium (Herdman 2000) Vestibular Exercise Program Objectives ► Complement CNS natural compensation diminish dizziness & vertigo enhance gaze stabilization enhance postural stability in static & dynamic situations ► Increase overall functional activities ► Patient education nature of pathology episodic nature, prognosis control of exacerbations Vestibular Program Components ► Gaze stabilization exercises to retrain VOR function ► Balance retraining to retrain VSR function ► Conditioning exercises to increase fitness level ► Habituation or canal repositioning maneuvers as indicated e.g., Unilateral Vestibular Lesion: Exercise Guidelines ► Adaptation is best stimulated by producing an error signal; work at limit of abilities ► Incorporation of head movements & visual input ► Provide context specific stimulation to promote adaptation ► Adaptation is positively affected by voluntary muscle control ► (Herdman 2000) Vestibular Function Recovery Rates ► UVL: 6-8 weeks ► BPPV: remission in 1/few treatments ► BVL: 6 months - 2 years ► CNS Lesion: 6 months - 2 years Physical Therapy Intervention: Prescription ► Individualized program: vestibular rehabilitation Outpatient, 1-2 times / week (4-6 weeks) HEP, 5 minutes, 3x / day Walking program (health & fitness prescription) ► Compliance to daily program essential to success ► Exercise graduated for possible increase of symptoms during the first week