Clinical Decision Making in Physical Therapy
advertisement

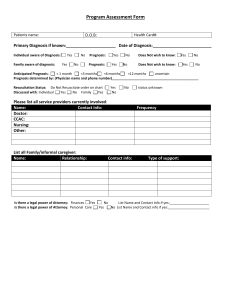
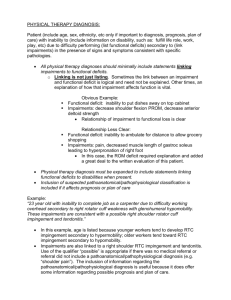
6 1 Clinical Decision Making Process 5 2 Universal Patient Management Guide 4 Connie Blow, MS, PT Kyle Gibson, PT, MA, OCS 3 University of Missouri-Columbia © 2007 Components of Clinical Decision Making 6 Examination 5 2 4 3 Examination Documentation Template • Begins with……… • Patient Demographics • Reason for Referral – Current Pathoanatomical or Pathophysiological conditions • Past Medical History • Systems Review • Tests and Measures Patient Demographics Demographics Patient Name Date of Birth Chronological Age Adjusted Chronological Age Date of Exam Referring Physician Other?? Reason for Referral • Client/Patient Preferred Outcome – Patient’s motivation expected outcome for seeking services. – This information encourages the therapist to keep patient centered examination, intervention and outcome measurement at the forefront of their minds. • Current Pathoanatomical or Pathophysiological Condition – Gives a medical, anatomical or phathophysiological context to the examination Past Medical History • Health History Questionnaire • Review of records Past health status Current health status Previous therapeutic interventions and outcomes Structured Patient/Client Interview – Red/yellow flags – Current Medications – Previous/Current Functional Level Social History – Work Status – Cultural Preferences Systems Review • Identification of issues requiring referrals or consultations • Status of: – – – – – Cardiopulmonary Integumentary Musculoskeletal Neuromuscular Cognitive/Arousal Systems Review Blood Pressure Edema Heart Rate Respiratory Rate Must memorize normal and exercise values for BP, HR, RR Betty Gail Phenomenon “I am fine………just a little dizzy” “I don’t know…..it’s probably the weather….what are we doing first today? “My sugar this morning? …..it was OK yesterday afternoon” “Oh, that bump on my heel? It’s nothing…..I just have to be careful when I first stand up on it” Quick Check • What is the normal blood pressure, heart rate and respiration rate for an 8 month old infant? • Blood Pressure 87-105/53-66 mm Hg • Heart Rate 100-160 bpm • Respiration Rate 30-60 breaths per minute Quick Check • What are four signs of increased ICP in an 8 month old infant? • • • • • • • • Irritability Vomiting (projectile) Sunset Eyes Increased Tone (change in tone) Difficult to arouse Increase Strabismus Changes in feeding Seizures Tests and Measures • Reliability • Validity • Appropriate Population • What are you wanting to measure and why? Quick Check • Where and the categories of tests and measures be found quickly? • Guide to PT Practice Categories of Tests and Measures • Disability – Ability to fulfill life roles in school, work, recreation, social • Functional Status – Mobility, transfers, play skills, self care • Impairments – Pain, ROM, strength, endurance, circulation • Pathophysiological – Often same as medical diagnosis • Disease, trauma, metabolic imbalance Components of Clinical Decision Making 6 5 Examination Evaluation 4 3 6 5 Examination Evaluation 4 PT Diagnosis Quick Check • PT Diagnosis is the same as the Practice Patterns found in the Guide to PT Practice. • False Diagnosis “Guide Language” “Both the process and the end result of evaluating examination data, which the physical therapist organizes into clusters, syndromes or categories to help determine the prognosis (including plan of care) and the most appropriate intervention strategies.” APTA Guide to Physical Therapy Practice Enhanced Mizzou Language • Statement that minimally links impairments to functional deficits. Include pathoanatomical or pathophysiological classification as it affects prognosis or plan of care. – Conclusion of the evaluative process – Helps determine the prognosis – Required to develop plan of care •This sounds like a call for a template! Documentation of PT Diagnosis • “Patient…… • “with an inability to…….(Disability) • “as a result of difficulty in performing…(Linking Disability to FL’s) • “secondary to....... (Linking FL’s to Impairments) • “in the presence of signs and symptoms consistent with specific pathologies Example • Patient is a 23 year old male with an inability to work as a carpenter due to difficulty reaching/working overhead secondary to right rotator cuff weakness with glenohumeral hypomobility. These impairments are consistent with a possible right shoulder rotator cuff impingement and tendonitis. Model • Patient is a 23 year old male with an inability to work as a carpenter due to difficulty reaching/working overhead secondary to right rotator cuff weakness with glenohumeral hypomobility. These impairments are consistent with a possible right shoulder rotator cuff impingement and tendonitis. • • • • • “Patient…… “with an inability to…….(Disability) “as a result of difficulty in performing…(Linking Disability to FL’s) “secondary to....... (Linking FL’s to Impairments) “in the presence of signs and symptoms consistent with specific pathologies IF it affects prognosis or plan of care. Physical Therapy Diagnosis Key Concepts Not the same as PT Practice Pattern More than an ICD Code Linking…NOT Listing – Linkage between functional limitations and impairments always required – Linking functional limitations to disability is required when disability is present – Inclusion of suspected pathoanatomical or pathophysiological classification is included as it affects prognosis or plan. 6 5 Examination Evaluation Prognosis PT Diagnosis Plan of Care Prognosis Determination of the ability to meet Client/Patient Preferred Outcome Total Time Needed to Reach Optimal Level of Functioning Based on Guide to PT Practice and Available Evidence Written as: Who, Will Do What, Under What Conditions, How Well, and By When Long Term Goals/Outcomes: generally address remediation of functional limitations & disability Short Term Goals: generally address remediation of impairments that have been linked to FL Patient Centered 6 Implementation POC Examination Evaluation Prognosis PT Diagnosis Plan of Care Documentation of Interventions • Described such that it reflects “skilled PT” – “Gait training”…..not sufficient – “Gait training utilizing manual and verbal cues for proper weight shift and symmetry of stride length.” Show link to outcome measures Evidence based Specific enough to guide care Document Patient/Family Consent and Understanding Outcomes Re-examination Examination Implementation POC Evaluation Prognosis PT Diagnosis Plan of Care Outcome Measures and Re-examination Efficacy of Treatment Goals and Objectives Reasonable? Appropriate Interventions for Impairments? Patient Motivation? Goals Patient Centered? Constraining Factors? Discharge? Revise Goals and Objectives? Quick Check • At what points in the Client Management Model do we base decisions on the best evidence? • Every One! Outcome Measures Re-examination Examination Patient Preference Implementation Plan of Care Evaluation Research Clinical Expertise Prognosis Plan of Care PT Diagnosis References • O’Sullivan SB, Schmitz TJ, Physical Rehabilitation Assessment and Treatment 4th ed. Philadelphia, PA 2001 • Guide to Physical Therapist Practice. Rev 2nd ed. Alexandria, Va: American Physical Therapy Association;2001 • Using the Guide for Pediatric Practice, Chiarello, LA October 2000 CSM Presentation • Quinn L, Gordon J, Functional Outcomes – Documentation for Rehabilitation. Saunders, Philadelphia PA 2003