lecture 8 -Stroke Volume (2012)
advertisement

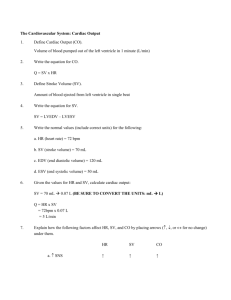
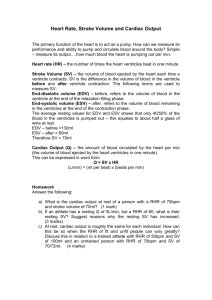
STROKE VOLUME Prof. Sultan Ayoub Meo MBBS, M.Phil, Ph.D (Pak), PG Dip Med Ed, M Med Ed (Scotland) FRCP (London), FRCP (Dublin), FRCP (Glasgow), FRCP (Edinburgh) Professor and Consultant, Department of Physiology, College of Medicine, King Saud University, Riyadh, Saudi Arabia LECTURE OUTLI NES / OBJECTIVES STUDENTS ABLE TO UNDERSTAND: • Understand the concept of preload and after-load • Determine factors effecting the end-diastolic Volume • Explain how cardiac contractility affect stroke volume • Describe the pressure volume loop STROKE VOLUME The amount of blood pumped out of each ventricle per beat is called stroke volume (SV). 70 ml. The output of the heart per unit time (minute) is called cardiac output. Cardiac Out put= Stroke Volume x Hear Rate [70 mL x 72 beats / min= 5040 ml. Approx] Cardiac Index: There is a correlation between resting cardiac output and body surface area. The output per minute per square meter of body surface is called cardiac index. Averages 3.2 L. STROKE VOLUME SV = EDV - ESV Stroke volume is also defined as the difference between the ventricular End Diastolic Volume [EDV] and the End Systolic Volume [ ESV]. EDV is the filled volume of ventricle prior to contraction ESV is the residual volume of blood remaining in the ventricle after ejection. The EDV is about 120 ml of blood and the ESV about 50 ml of blood. The difference in these two volumes 70 ml represents the SV. Factor that alters either the EDV or the ESV will change SV. Example: Increase in EDV increases SV, whereas an increase in ESV decreases SV. STROKE VOLUME When the heart contracts strongly, the end-systolic volume can be decreased to as little as 10 to 20 milliliters. Conversely, when large amounts of blood flow into the ventricles during diastole, the ventricular end diastolic volumes can become as great as 150 to 180 milliliters in healthy heart. By both increasing the end-diastolic volume and decreasing the end-systolic volume, the stroke volume output can be increased STROKE VOLUME Preload affect the SV through the increase in venous return to the heart, increases the filled volume (EDV) of the ventricle, which stretches the muscle fibers thereby increasing their preload. This leads to an increase in the force of ventricular contraction Afterload is related to the pressure that the ventricle generate to eject blood into the aorta. Changes in afterload affect the ability of the ventricle to eject blood and thereby alter ESV and SV. increase in afterload, increase aortic pressure, decreases SV, and causes ESV to increase. STROKE VOLUME STROKE VOLUME STROKE VOLUME / CARDIAC OUT PUT Factor No change Sleep Moderate changes in environmental temperature Increase Anxiety and excitement (50–100%) Eating (30%) Exercise (up to 700%) High environmental temperature Pregnancy Epinephrine Decrease Sitting or standing from lying position (20–30%) Rapid arrhythmias, Heart disease PRESSURE VOLUME LOOP 10 There are only three ways that the body regulates stroke volume from minute-tominute: • Filling pressure (preload) • Aortic pressure (afterload) • Contractility 11 PRESSURE VOLUME LOOP The ejection loop 12 PRESSURE VOLUME LOOP Changing filling pressure changes stroke volume only by changing LVEDV This could be an example of transfusion Lowering LVEDP has the opposite effect (hemorrhage) 13 Lowering the aortic pressure causes the ventricle to empty more completely. The stroke volume increases by an amount equal to the fall in LVESV. LVEDV is not affected. Raising aortic pressure has the opposite effect 14 PRESSURE VOLUME LOOP Increasing contractility decreases LVESV and thus increases stroke volume. LVEDV is not affected. Heart failure has the opposite effect 15 PRESSURE VOLUME LOOP Decreasing the diastolic compliance decreases LVEDV and stroke volume but has no effect on LVESV 16 The real ejection loop has a rounded top since the blood pressure increases during ejection (auxotonic beat) 17 Decreased compliance occurs only in disease and is not a physiological regulator 18 Hypertrophy Normal Dilation 19 Hypertrophy Normal Dilation Hypertrophy results from increased afterload over several months. Dilation results from persistently elevated preload over several days. 20 Hypertrophy Normal Dilation Hypertrophy results from increased afterload over several months. Dilation results from persistently elevated preload over several days. Fiber slippage at the desmosomes will occur before the fibers will extend beyond Lo 21 Hypertrophy Normal Dilation Hypertrophy results from increased work load over several months. Increased mass Dilation results from persistently elevated preload over several days. Same mass The large chamber diameter and thin wall puts the dilated heart at a mechanical disadvantage. 22 Notice that stroke volume change in a reciprocal manner. Stroke Work = P x Vol As P goes up V naturally goes down so their product remains constant. Stroke work should be independent of any change in blood pressure. 23 If aortic pressure is held constant stroke volume increases with contractility. Stroke volume goes down as aortic pressure goes up. Since stroke volume changes reciprocally with aortic pressure their product (stroke work) is relatively independent of aortic pressure 24 How can we measure contractility in the patient? Ejection fraction = (LVEDV-LVESV) / LVEDV The fraction of the ventricular contents at end diastole that is ejected. 25 How can we measure contractility in the patient? Ejection fraction = (LVEDV-LVESV) / LVEDV A normal ejection fraction should be above 0.50. Ejection fractions of 0.30-0.50 are of concern. Values below 0.30 carry a poor prognosis. 26 How can we measure contractility in the patient? Ejection fraction = (LVEDV-LVESV) / LVEDV Can be easily measured by •X-ray • Nuclear techniques • Echo 50-60 normal 35-49 concern <35 serious 27 Often contractility is lost in just a region of the heart as occurs in a myocardial infarction. Regional dysfunction can be seen with ultrasound or with a X-ray of the ventricle. Normal Regional akinesis 28