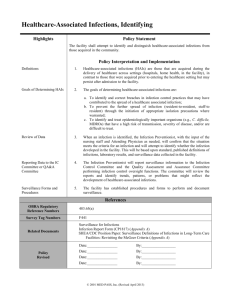
Surveillance of HAI
advertisement

Surveillance Of Health Care associated infections By Dr. Alaa Gad Infection Prevention & Control Specialist Infection at Healthcare Facilities DEFINITION Health care associated or hospital-acquired infection (HAI) (nosocomial infections) can be defined as: Infection acquired during hospitalization; not present or incubating at the time of admission to hospital (i.e. occurs at least 48 hours after admission). 2 Factors contributing to increased incidence of infection transmission at healthcare facilities • • • • Patients are generally less immune. Patients may have infections. Patients undergo invasive procedures. Healthcare providers may transmit infections to clients and to themselves. • Other general factors Overcrowding with limited physical space Staff shortages. Poor infrastructure. 3 Modes of Nosocomial Infection Transmission Endogenous source Exogenous source Normal flora Any Organism C/A Altered resistance Or Introduction of microbes into normally sterile areas e.g. intravenous catheter. Results from Introduction of microbes into or on the patient from an outside source e.g. hands of staff 4 Disease-Transmission Cycle (The Chain of Infection ) 5 How to Prevent Nosocomial Infection Killing the agent • e.g., applying an skin antiseptic agent before surgery Blocking means of transmission from infected to susceptible • e.g., hand washing to remove bacteria or viruses acquired through touching an infected patient Immunize susceptible • e.g. HBV vaccination of HCWs 6 Break The Chain Inhibiting or killing the agent Blocking transmission Immunize susceptible 7 Infectious Agent • The infectious agent is the microorganism that can cause infection or disease. • Pathogens may be classified as conventional, conditional, or opportunistic based on their ability to cause disease in normal Vs immunocompromised hosts. However, almost any microbe, in favorable circumstances e.g. if introduced into a normally sterile area, can cause infection. 8 Conventional (acute) pathogens Cause disease in Examples Conditional pathogens Opportunistic pathogens Healthy individuals •Local trivial infection in healthy. •Persons with reduced resistance to infection. •When implanted directly into tissue or in a normally sterile area. only in patients with profoundly diminished resistance to infection e.g. AIDS, cancer. Bacteria: •Staph. aureus, •Strept. pyo, •Salmonella, •Shigella, •C. diphtheriae, •M. tuberculosis, •B. pertussis , Viruses: •Hepatitis A, B, C, •Rubella virus, •Rotavirus, •HIV •Strept. agalactiae, •Enterococci., •C. tetani, •E. coli, •Klebsiella , •Serratia marcescens, •Acinetobacter baumanii, •Pseudomonas aeruginosa, •Candida •Listeria monocytogenes, •Toxoplasma, •Aspergillus, •Legionella. •Atypical mycobacteria, •Nocardia asteroides, •Pneumocystis carinii, •Cryptococcus neoformans, •Histoplasma, •Cryptosporidium. •Previous columns. 9 Colonization Vs Infection • It is the presence of microorganisms at a body site(s) without presence of symptoms or clinical manifestations of illness or infection. • Colonization may be a form of carriage and is a potential method of transmission. 10 The transition from colonization to infection • Developing an infection after contact with microorganisms depends upon the interaction between the contaminating organisms and the host. • Not all individuals who are colonized will develop infection. In fact, those who have progressed from colonization to infection may represent only the “tip of the iceberg” of persons carrying a particular pathogen. 11 Minimal infective dose of a microorganism • It is the critical number of microorganisms present on or in a tissue that when exceeded, it is very likely that the tissue will become infected. • It varies by the type of microorganism and by point of entry or invasion. • Many causative agents of Hospital-acquired infections have a relatively high minimal infective dose e.g. For Klebsiella, Serratia spp. and other Enterobacteriaceae it is more than 100,000 microorganisms (105 cfu/ml). • Some causative agents, however, require very few particles to infect, such as hepatitis B virus (less than 10 viral particles). 13 Surveillance of Hospital – Acquired infections Surveillance is the ongoing, systematic collection, analysis, interpretation, and dissemination of data regarding a healthrelated event for use in public health action in order to reduce morbidity and mortality and to improve health. 14 •Data disseminated by a public health surveillance system can be used for: • Guide immediate action for cases of public health importance; • Measure the burden of a disease (or other health-related event), • Monitor trends in the burden of a disease (or other healthrelated event), including the detection of epidemics (outbreaks) and pandemics; • Guide the planning, implementation, and evaluation of programs to prevent and control disease, injury, or adverse exposure; • Prioritize the allocation of health resources; • Provide a basis for epidemiological research. • Surveillance of Hospital-acquired infections is a key function of the Infection Prevention & Control team. 15 Steps of surveillance • Assess the population served by the facility so that interventions can be directed at those complications of greatest importance given available resources. • Select the outcome (surgical site infection) or process (prophylactic antibiotics )for surveillance. • Define all data elements and assure criteria definitions are valid, accurate, and reproducible. • Collect the surveillance data. • Calculate and analyze surveillance rates. • Report and distribute surveillance information. 16 Aim of Surveillance •serve as an early warning system for impending public health emergencies. •Document the impact of an intervention, or track progress towards specified goals. •Monitor and clarify the epidemiology of health problems, to allow priorities to be set. surveillance Major Types of health –care associated infection UTI SYS SSI SST BSI CAUTI VAP REPR PNEU CLABSI LRI BJ Device associated Infections GI CNS EENT CVS Urinary Tract Infection Surgical Site Infection Blood Stream Infection Pneumonia Bone and Joint Infection Central Nervous system Cardiovascular System infections Eye , Ear , Nose and Throat Gastrointestinal System Infection Lower Respiratory Tract infection Reproductive Tract Infection Skin and Soft Tissue infection Systemic Infection NHSN / CDC facts • • • • • 14 Million operative procedures done annually SSI is the second most common HAI SSI Proportion is 17% SSI overall rate is almost 2% SSI associated with more than 8000 deaths annually 33 What is operative procedure • Procedure performed to a patient (inpatient /Outpatient) takes place during an operation(single trip to OR)where a surgeon makes at least one incision through the skin or mucus membrane , including laparoscopic approach and close the incision before the patient leaves the OR 34 SSI surveillance • Feedback of appropriate data to surgeons has been shown to be an important component of strategies to reduce SSI risk (CATS Implementation after mesurment). • Successful surveillance program needs Epidemiologically sound infection definitions and effective surveillance methods 35 36 Surgical Site Infection Organ space DIP SIP SSI DIS SIS Superficial incision surgical site infection •Infection occurs within 30 days after the operative procedure •Involves only skin and subcutaneous tissue of the incision •Purulent drainage •Organism isolated (aseptically obtained culture of fluid or tissue from the superficial incision ) • Pain , Tenderness , Localized swelling , Redness or Heat •Physician diagnosis (evidence : documenting ,Antibiotic , TLC changes ! ) Deep incision surgical site infection •Infection occurs within 30 days after the operative procedure if no implant is left in place (1 year) •Involves deep soft tissues fascial and muscle layers of the incision •Purulent drainage •Organism isolated (aseptically obtained culture of fluid or tissue from the deep incision) • fever , localized pain, tenderness •Abscess or other evidence of infection involving the deep incision is found by direct examination ,reoperation , histopathology or radiologic examination •Physician diagnosis (evidence : documenting ,Antibiotic ,TLC changes ! ) Organ / Space surgical site infection •Involves any part of the body excluding the skin incision , Fascia , muscle layers. Osteomyleitis Breast Abscess or mastitis Myocarditis or periarditis Disc Space Ear ,Mastoid Endometritis Endocarditis Eye other than conjunctivitis GI tract Intraabdominal Intracranial ,brain abscess or dura Respiratory tract (Not PPP) Mediastinitis Meningitis or ventricullitis Oral cavity Male or female reproductive tract Urinary tract infection Spinal abscess without meningitis Sinusitis Upper respiratory tract Arteial or venous infection Vaginal cuff Joint or bursa Organ / Space surgical site infection Appendectomy with subsequent subdiaphragmatic abscess will be reported as organ /space SSI at the intraabdominal specific site Organ / Space surgical site infection •Infection occurs within 30 days after the operative procedure if no implant is left in place (1 year) •Involves any part of the body excluding the skin incision ,fascia or muscle layers that is opened or manipulated during the operative procedure. •Purulent drainage from the drain •Organism isolated (aseptically obtained culture of fluid or tissue from the organ /space) •Abscess or other evidence of infection involving organ /space is found by direct examination ,reoperation , histopathology or radiologic examination •Physician diagnosis (evidence : documenting ,Antibiotic ,TLC changes ! ) Data Analysis Numerator All SSI patients recorded during the selected time period . Denominator All patients having procedure during the same time period . SSI rate per 100 % Data Stratification Total SSI rate % reflecting total infected procedures regardless the likelihood of getting infection Individual differs from each other of their susceptibility of getting infection We have to do Stratification for all / Selected operative procedure Data will be presented by Standardized Infection Ratio RISK INDEXD We calculate patient risk index category using the four elements 1. 2. 3. 4. ASA score Wound class Operation duration Laparoscopy ASA Rated by Anesthesiologist prior to operation ASA Physical Status 1 - A normal healthy patient ASA Physical Status 2 - A patient with mild systemic disease ASA Physical Status 3 - A patient with severe systemic disease ASA Physical Status 4 - A patient with severe systemic disease that is a constant threat to life ASA Physical Status 5 - A moribund patient who is not expected to survive with / without the operation Wound class An assessment of likelihood and degree of contamination of surgical wound at the time of the operation Clean An uninfected operative wound in which no inflammation is encountered and the respiratory ,alimentary ,genital or uninfected urinary tract are not entered Clean –Contaminated Operative wound in which the respiratory ,Alimentary ,genital or urinary tract are entered under controlled conditions and without unusual contamination (no evidence of infection) Contaminated Open ,fresh ,accidental wound in addition operations with major break in the sterile technique Dirty / Infected Traumatic wound with retained devitalized tissue and those involving existing clinical infection or perforated viscera NHSN/CDC data Cut point (75th percentile ) Hospital Joining the data collection Standardized Infection Ratio Standardized Infection Ratio, SIR, is a summary measure used to compare the HAI experience among one or more groups off patients to that of a standard population’ Accounts for differences in risk of HAI among the group 53 Calculation of SIR • • • • SIR = Observed (O) HAIs Expected (E) HAIs Ratio of Observed to Expected infection Risk-adjusted summary measure Used to compare overall HAI rates of any two patient cohorts, groups, or hospitals 54 55 Aim of the project 1. Measuring the Current situation in the participating hospital 2. Enhancing the quality of patient care by encouraging hospitals to use data obtained from surveillance to compare their rates of SSI over time and against a benchmark rate, and to use this information to review and guide clinical practice. 3. Establishing a National /regional Benchmark. Surveillance methodology Active surveillance by trained personnel use a variety of methods to identify cases of infection. Participating Hospitals Targeted Procedure Methods of surveillance to identify surgical site infections Follow-up of patients during the inpatient stay: Review medical and nursing records, temperature and treatment charts to identify signs and symptoms that may indicate an SSI. Methods of surveillance to identify surgical site infections Follow-up of patients during the inpatient stay: Review microbiology reports to find any positive surgical site cultures from patients in the study population and check with the ward why the cultures were taken and if there are clinical signs of infection. Methods of surveillance to identify surgical site infections Detecting SSI in patients readmitted to hospital / OR • establish systems to alert if a patient included in the surveillance is readmitted. If a patient is admitted with an SSI resulting from an operation performed in another hospital the IPCD should liaise with surveillance staff at the hospital in which the procedure took place so that they can report the infection . SSI Surveillance Readmission OR/Hospital for the target procedure in the surveillance time period Flagging System 64 Methods of surveillance to identify surgical site infections SSI detected by healthcare professional during systematic post discharge follow up All patients included in the surveillance attend OPD after their operation and this provides an opportunity to review their wound for SSI. Clinicians should clearly indicate symptoms on a standard report form Methods of surveillance to identify surgical site infections • SSI reported by patient PostDischarge Phone contact from the HCWs ,Educating patient about warning signs of infection to contact the hospital SSI surveillance High Risk High Volume Data Sources Classification according to risk Index Post discharge Continuo monitoring Benchmarking Readmission OPD Home Contact Feedback Improvement Plan analysis Surveillance period Analysis & Interventions Calculation of SSI rate within each risk index category and compare with the NHSN Benchmark 1 year 1 month THANK YOU FOR ALL YOU DO TO PROTECT PATIENTS FROM HARM! 69