Cerebrovascular endothelial cells are protected from ischemic injury
advertisement

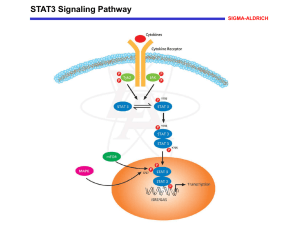
Cerebrovascular endothelial cells are protected from ischemic injury by STAT3 C.M. Davis and N.J. Alkayed Department of Anesthesiology and Perioperative Medicine, Oregon Health and Science University, Portland, OR 97239, USA. Signal Transducer and Activator of Transcription 3 (STAT3) plays a protective role in the brain following ischemia/ reperfusion injury. The function of STAT3 in cerebral endothelial cells in response to ischemic injury has not been investigated. Since neuronalspecific ablation of STAT3 does not alter infarct size, endothelial STAT3 may be responsible for the STAT3-mediated protection in the brain. We therefore hypothesized that STAT3 protects endothelial cells from ischemic injury. We used primary adult mouse cerebrovascular endothelial cells and subjected them to oxygen and glucose deprivation (OGD), an in vitro model of ischemia. Using Western blot analysis, we found that STAT3 protein levels and its phosphorylation on tyrosine residue 705 are regulated by OGD; they are decreased immediately following OGD but increase to exceed pre-OGD levels by 24 hours of reoxygenation. Using a pharmacological inhibitor of STAT3 activation, we show that attenuation of STAT3 signaling induces endothelial cell death. STAT3 is therefore a survival factor for endothelial cells, and plays an important role in determining susceptibility to ischemic damage. We demonstrate that STAT3 is essential for correcting endothelial dysfunction after ischemic injury. Since endothelial dysfunction is a contributing factor, as well as an outcome of pathological states, regulation of endothelial STAT3 may have important consequences in cerebrovascular disease. 1 STAT3 is regulated by ischemic injury in endothelial cells 3 Ischemia and STAT3 inhibition reduce nitric oxide release by endothelial cells A. A. P-STAT3 Y705 is present at baseline and increases after OGD in HUVECs. A. Nitric Oxide levels are decreased following OGD The levels of the final products of nitric oxide, nitrate and nitrite, are reduced in culture medium following 8 hours of OGD compared to baseline controls. Human Umbilical Vein Endothelial Cells immunolabeled for P-STAT3 Y705 (green) at baseline 24 hours following 8- hour OGD B. STAT3 inhibition reduces nitric oxide levels. Application of sub-lethal doses of Stattic and AG490 results in a decrease in nitrate/ nitrite in culture medium compared to vehicle treated cells. This is observed both in baseline (light blue) and cells subjected to OGD (dark blue). B. A. B. B + C. STAT3 and its phosphorylation are decreased/ abolished immediately following OGD, increasing during reperfusion. Western blot analysis (B) of primary mouse brain endothelial cells. 8 hours of OGD abolishes phosphorylation at Y705, and decreases phosphorylation at S727 as well as total STAT3. All levels increase during reperfusion. Quantified in (C ). C. 2 Inhibition of STAT3 induces endothelial cell death A. Pharmacological inhibition of STAT3 activation by (A) 10µM Stattic, or (B) 50µM AG490 induces endotheilal cell death. Inhibitors were applied to cells for 12 hours immediately following 8 hours of OGD (dark blue) or their baseline controls (light blue). Cell death was assessed by Calcein -AM (live) and propidium iodide (PI; dead) labeling. Death is expressed as PI- positive cells as a percentage of total (Calcein- AM + PI- positive) cells. 4 Conclusions 1. STAT3 in brain endothelial cells is regulated by ischemia. STAT3, and its phosphorylation levels are decreased immediately following OGD, but increase during reperfusion. 2. The increase in STAT3 observed during reperfusion protect brain endothelial cells from cell death. Pharmacological inhibition of this increase in STAT3 activation during reperfusion results in cell death. 3. OGD reduces nitric oxide release from endothelial cells, an indicator of endothelial dysfunction. B. 4. STAT3 activation is a positive regulator of correct brain endothelial function. Inhibition of STAT3 activation, both at baseline and following OGD, results in endothelial dysfunction, as measured by nitric oxide release. Minimal death was observed in vehicle (baseline and OGD) conditions. However cell death was observed on STAT3 inhibition; this effect was greater in OGD compared to baseline cells. Acknowledgements: This work was supported by a Pacific Mountain Affiliate Postdoctoral Fellowship from the American Heart Association to C. M. Davis.