Approach To The Patient In Shock
advertisement

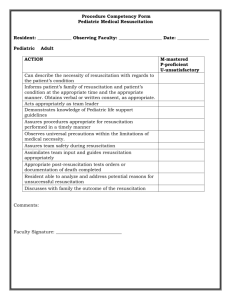
Approach To The Patient In Shock By James Holencik, DO Epidemiology • More than 1 million cases of shock present to US ED’s yearly. • Approx. 30-45% of patient in septic shock, and 60-90% for those with cardiogenic shock die within 1 month of presentation. Pathophysiology • • 1. 2. 3. 4. Shock is defined as: circulatory insufficiency that creates an imbalance between tissue oxygen supply and demand. Four categories of shock: Hypovolemic Cardiogenic Distributive Obstructive Pathophysiology Cont. • Normally, the tissues consume approximately 25% of the oxygen carried on hemoglobin. • Venous blood returning to the right heart is approximately 75% saturated. • When demand is insufficient the first compensatory mechanism is increase in cardiac output (CO). Pathophysiology Cont. • When compensatory mechanisms failure the body starts anaerobic metabolism forming lactic acid. • Shock is usually, but not always, associated with systemic arterial hypotension, ie SBP <90. Pathophysiology Cont. • 1. 2. 3. 4. The onset of shock provokes a myriad of autonomic responses. Arteriolar vasoconstriction. Increase in HR and contractility increases CO. Constriction of venous capacitance, which augments venous return. Release of vasoactive hormones epi, norepi, dopamine, and cortisol to increase arteriolar and venous tone. Pathophysiology Cont. 5. Release of ADH and activation of the renin-angiotensin axis to enhance water and sodium conservation. • The cellular response to a decrease in systemic O2 delivery is ATP depletion leading to ion-pump dysfunction (influx Na+ and efflux K+ leading to membrane instability and cellular dysfunction. Pathophysiology Cont. • • 1. 2. 3. 4. In early phases of shock the physiologic changes produce a clinical syndrome called SIRS (systemic inflammatory response syndrome). SIRS is defined as 2 or more of the following features. Temp. >38 or less than 36. HR >90 beats/min. RR faster than 20. WBC’s >12 or <4 or >10% bands. Physical Examination • No single vital sign or value is diagnostic of shock. • Look at the whole patient. • Refer to all the vital signs as well as physical signs of shock (cynosis, confusion, restlessness, and other signs of poor perfusion). Diagnosis • • • • • • • Ancillary Studies: CBC, BMP with Mg and Phos. PT, PTT, UA, lactic acid, ABG, Preg test. CXR, EKG, Hepatic func., cortisol level. Blood, urine, sputum, and pelvic cultures. CT head and sinuses, lumbar puncture. Invasive tests: filling pressures, CO, and central venous oxygen saturation. Diagnosis • Also monitoring of pulse ox, electrocardiographic, CVP, arterial line, and end-tidal CO2. Treatment • The rationale for early intervention • Application of an algorithmic approach to optimize hemodynamic endpoints with early goal directed therapy reduces ED mortality by 16%. • Also the ABCDE tenets of shock resuscitation must be established. Treatment Cont. • Establishing Airway • Airway is best controlled with endotracheal intubation for airway protection. • Sedatives used in intubation can worsen hypotension, through arterial and venous dilation as well as myocardial suppression. • Volume resuscitation or application of vasoactive agents may be needed before intubation. Treatment Cont. • Controlling Work of Breathing • Control of breathing is required when tachypnea accompanies shock. • Respiratory muscles are significant consumers of O2 during shock increasing lactate formation. • Mechanical ventilation and sedation has been shown to improve survival. Treatment Cont. • Optimizing the Circulation • Hemodynamic stabilization begins with IV access through large bore peripheral lines. • Trendelenburg positioning does not improve cardiopulmonary performance compared with the supine position. • Trendelenburg position may worsen pulmonary gas exchange and predispose to aspiration. Treatment Cont. • Central venous access will aid in assessing volume status (preload) and monitoring central venous oxygen sats (Scvo2). • This is also the preferred route of vassopressor therapy. • Fluid resuscitation begins with isotonic crystalloid, initially 20cc/kg. Treatment Cont. • The colloid vs crystalloid resuscitation controversy remains despite a slight increase in mortality when colloids are used. • Vasopressor agents are used when an inadequate response to volume occurs. • Vasopressors are most effective when vascular spaces are full and least when empty. Treatment Cont. • The use of vasopressors is accompanied with pitfalls: decreasing capillary blood flow in certain tissue beds (bowel), and falsely elevates intracardiac filling pressures (CVP). Treatment Cont. • Assuring Adequate Oxygen Delivery • Arterial saturation should be returned to 9395% and hemoglobin above 10g/dl. • A hyperadrenergic state results from the compensatory response to shock, physiologic stress, pain, and anxiety. • Shivering frequently results so patient need to be kept warm. Treatment Cont. • Achieving End Points of Resuscitation • Traditional end points have been normalization of blood pressure, heart rate, and urinary output. • A goal-directed approach at achieving urine output >.5cc/kg/hr, CVP 8-12, MAP 65-90, and venous oxygen sat >70% during ED resuscitation greatly reduced mortality. Treatment Cont. • Bicarbonate Use in Shock • Experimental data indicates that exogenous bicarb can actually worsen intracellular acidosis, and has not be shown to have a benefit. • Bicab also shifts the oxygen-hemoglobinbound curve to the left impairing tissue unloading. Treatment Cont. • A compromise is to partially correct the acidosis. • Bicarb deficit is determined by (normal HCO3 minus the patients HCO3) X 0.5 X body weight (kg). • One-half of this amount is infused slowly and the remainder over 6-8hr. • Bicarb should be withheld once the pH is 7.25 or greater. Disposition and Transition to the Intensive Care Unit • A system-oriented problem list with an assessment and plan, including all procedures and complications, should be verbally communicated and written prior to transfer. • Currently outcome prediction at ED disposition has not been fully studied. Fluid And Blood Resuscitation Fluid and Blood Resuscitation • Fluid resuscitation is the initial therapy for disorders causing intravasular volume depletion with resulting tissue hypoperfusion and organ dysfunction. • Acute hemorrhage is the predominant cause of acute intravascular volume loss requiring aggressive fluid resuscitation. Fluid and Blood Resuscitation • Until recently, the widely accepted goal of fluid resuscitation was to restore a state fo normovolemia. • However present laboratory and clinical reports have raised controversy about filling the tank in the setting of ongoing hemorrhage. Fluid and Blood Resuscitation • The objective of fluid resuscitation is to restore sufficient intravascular volume and oxygen-carrying capacity to maintain cellular delivery of metabolic substrates sustaining cellular viability. Pathophysiology • The acute loss of intravascular volume triggers a wide range of physiologic regulatory responses. • At the cellular level, hemorrhagic shock is defined as a state of impaired oxidative metabolism and homeostasis due to inadequate O2 delivery and inadequate cellular waste removal. Pathophysiology • Loss of circulating blood volume leads to decreases in arterial blood pressure, venous return, and ventricular stroke volume. • This in turn leads to a physiologic response by the body to increase HR, arterial and venous constriction, increased ventricular contractility, and extravascular to intravascular fluid shift. Pathophysiology • Vagal tone is decreased • Kidneys through the stimulation of reninangiotensin-aldosterone system and ADH retain Na+ and H2O. • Angiotensin II and vasopressin promote vasoconstriction. • Activation of the coagulation system leads to platlet depostion and release of local mediators. Pathophysiology • Severe hemorrhage causes decreased CO, and vital organs will only be perfused (brain and heart). • Once decompensation of the bodies natural responses occur myocardial contractility decreases, local tissue acidosis and hypoxia develops resulting in loss of peripheral vasocontriction. Clinical Features • The hemodynamic profile response to hemorrhage induced hypovolemia commonly includes tachycardia, hypotension, and signs of poor peripheral perfusion. • Arterial and venous constriction lead to a narrow pulse pressure. • Hypoalertness ensues secondary to cerebral hypoperfusion. Clinical Features Cont. • The normal total circulating volume of an adult is approx. 7% of total body weight. • Therefore 5L for a 70kg patient divided into 3L of plasma and 2L of RBC’s. • Class 1 shock is loss of 15% (750ml) of circulating blood. • Usually well tolerated in healthy patients. Clinical Features Cont. • Class 2 shock is loss of 15-30% (7501500ml) of circulating blood. • Results in tachycardia and narrow pulse pressure. • Class 3 shock is loss of 30-40% (15002000ml) circulating blood. • Hypotension, tachycardia, peripheral hypoperfusion, and decline in mental status. Clinical Features Cont. • Class 4 shock is loss of >40% (>2000ml) of circulating blood. • The body has reached its limits to compensate and therefore imminent hemodynamic collapse. • Be cautious with elderly due the possibility to evoke tachycardia secondary to poor heart function or medication. Management • Initial therapy should involve securing an airway, assuring adequate ventilation and oxygenation, controlling external bleeding, and spinal cord protection when necessary. • Obtain 2 large bore IV’s • Fluid resuscitation keep 3 objectives in mind. 1. Restoring intravascular volume sufficiently to reverse systemic hypoperfusion. Management Cont. 2. Maintaining adequate oxygen-carrying capacity so that tissue oxygen delivery meets critical tissue oxygen demand. 3. Limiting ongoing loss of circulating RBC’s. -- Place foley cath to monitor urinary output. Fluid Resuscitation • Currently there is controversy concerning normotensive vs hypotensive resuscitation. • The goal of hypotensive resuscitation is to provide sufficient fluid to maintain vital organ perfusion and avoid cardiovascular collapse while keeping arterial BP relatively low (MAP of 60). Fluid Resuscitation Cont. • Currently there still is controversy concerning crystalloids vs colloids for use in resuscitation. • The cost of colloids greatly out weights that of crystalloids causing most to use the later. Isotonic Crystalloid Solution • Comprised mainly of normal saline and lactated Ringer’s. • Crystalloids are hypo-oncotic because of there lack of protein. • Therefore most of the fluid given will shift into the extravascular space instead of the intravascular or interstitial space. Isotonic Crystalloid Solution Cont. • This is the physiologic basis for the 3:1 ratio for isotonic crystalloid volume replacement. • Therefore for every amount of blood lost 3 times that amount is needed to replace intravascular volume using crystalloids. Isotonic Crystalloid Solution Cont. • Concerns have been raised about each fluid. 1. Infusing large volumes using either causes increased neutrophil activation. 2. LR also increases cytokine release and may increase lactic acidosis in large amounts. 3. NS exacerbates intracellular potassium depletion and causes hypochloremic acidosis. Solution makeup Osmal. Glucose • • • • • 5% D/W 278 10%D/W 556 .45% NS 154 .9% NS 308 LR 274 K+ Ca+ 0 0 0 0 100g/l 0 0 0 0 0 0 77 77 0 0 0 0 154 154 0 0 0 0 130 109 4 1.5 28 50g/l Na+ Cl- 0 Lactate • Na, Cl, K, Ca, and lactate are measured in mmol/liter. Colloid Resuscitation • Colloids have larger molecular weight particles with plasma oncotic pressures similar to normal plasma proteins. • With this it would be thought colloids would be more effective at restoring circulating blood volume compared to crystalloid solutions. Colloid Resuscitation Cont. • However, in a systematic review of the use of albumin in critically ill patients found an increase relative risk of death, as compared to the use of crystalloids. • Given the much greater cost of colloid products, there is no clear basis for the choice of these agents over crystalloids for resuscitation. Blood Transfusion • Remember there are no clear parameters for transfusions. • It is generally accepted that a patient in shock not responding to 2-3 liters of crystalloids will need a blood transfusion. • Per American Society of Anesthesiologists patients with an H/H of 10/30 will very rarely need a transfusion. Blood Transfusion Cont. • However an H/H of 6/18 will almost always need a transfusion. • This however leads to a large area of hemoglobin between 6-10. • Many factors must be taken into account when transfusing between the 6-10 mark. • Remember blood is the ideal resuscitation agent. Hypertonic Resuscitation Fluids • Hypertonic saline has been proposed as a potential crystalloid solution alternative to isotonic due to the limited tissue edema. • Has been showed to rapidly expand intravascular volume and enhance tissue perfusion. • Could be a potential benefit in trauma patients by limiting cerebral edema, lowering intracranial pressure, and improving cerebral perfusion. Hypertonic Resuscitation Fluids Cont. • Also may limit pulmonary interstitial fluid shift. • The volume given during resuscitation must be monitored due to the propensity of causing hypernatremia. Oxygen-Carrying Resuscitation Fluid • Currently not being used in present day resuscitation. • Studies underway for use during resuscitation efforts. • The thought behind the idea is to have products able to carrying O2 when loss of RBC’s occur. • Two classes of agents, hemoglobin-based O2 carriers and fluorocarbon-based O2 carriers. Questions • • A. B. C. D. • T or F the best fluid to use during resuscitation is colloids. Which does not define SIRS: WBC >12000 RR >20 SBP <90 HR >90 T or F Class 2 shock is loss of circulation blood volume of 750-1500. Questions Cont. • A. B. C. D. • • Which is not one of the categories of shock? Obstructive Restrictive Distributive Hypovolemic T or F shock is associated with a SBP of <100 Answers: F, C, T, B, F