Nursing 715 Pharmacological Basis of Therapeutics
advertisement

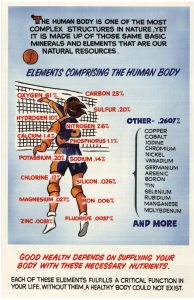
Introduction to Principles of Clinical Pharmacology Definition of Basic Terms Drug Simply – a drug is a chemical or substance that causes changes in the structure or function of living organisms Medicine A medicine is the vehicle for administration of the drug (active ingredient) to the human or animal e.g. tablet, capsule, injection, ointment, inhaler, suppository etc. Does This Apply to Foods/Minerals etc? Obviously, they are not ‘drugs’ in the conventional use of the term However, from a prescribing perspective, many are regarded as ‘medicines’ In addition, all prescribers should have a general understanding of pharmacology and pharmacokinetics as their patients will be on a range of medications Does This Apply to Foods/Minerals etc? In this course ‘Drug’ is used as a generic term, to include vitamins/minerals/supplements etc. when they are used for therapeutic purposes From a pharmacological perspective, ‘drugs’ are not ‘good’ or ‘bad’; they are simply molecules that cause some physiological event to occur Sources of Drugs Plant sources eg morphine, atropine, some vitamins Animal sources eg thyroxine, insulin Mineral sources eg lithium, magnesium Microorganisms eg penicillins, cephalosporins Synthetic eg benzodiazepines, phenothiazines, some vitamins Bioengineered (recombinant DNA technology) eg human insulin, human growth hormone Definition of Basic Terms cont. Generic name Standardised internationally recognised name for a drug e.g. ferrous sulfate, metoprolol, omeprazole, ibuprofen etc. (some exceptions in US e.g. paracetamol = acetominophen) Trade or Brand name Name given by the manufacturer e.g. Ferrogradumet (ferrous sulfate), Viagra® (sildenafil); Ventolin® (salbutamol) Definition of Basic Terms cont. Pharmacology Simply: the science of drug actions and uses Pharmacodynamics Mechanisms of action (“what the drug does to the body”) Pharmacokinetics Literally, movement of the drug within the body (“what the body does to the drug”) Definition of Basic Terms cont. Toxicity Manifestation of the harmful effects of the drug after exposure to high levels (“intoxication” or “poisoning”) Therapeutics Use of drugs for intended clinical benefits – cure of a disease, relief of symptoms etc. Therapeutic Prescribing Prime goal of drug therapy is to achieve the desired beneficial effects with minimal adverse effects Choice of drug will be governed by mechanism of action (pharmacodynamics) Dose of drug, route, formulation etc. will be determined by how the body handles the drug (pharmacokinetics) Pharmacodynamics: Basic Principles Mechanism of action of drugs Specific molecular processes by which drugs work, e.g. inhibition of an enzyme or stimulation of a receptor subtype Mode of action of drugs General description of the type of action: e.g. supplements, antihypertensives, analgesics Site of action of drugs Specific organs, tissues or cells affected by the drug: e.g. sensory neurones; myocardium, bronchii, etc. How Do Drugs Work (Mechanism of Action)? Fundamental premise of pharmacodynamics is ‘drugreceptor interactions’ Within the organs of the body are specific receptors with which specific drugs can interact The analogy often used is ‘lock and key’: only drugs (chemicals) with the ‘correct’ molecular shape can interact with a particular receptor Example: Morphine Naturally-occurring substance found in the Opium Poppy (Papaver somniferum) One of a family of natural substances known as opiates or opioids (includes codeine) Some synthetic derivatives also available e.g. heroin, methadone, pethidine Been used for both therapeutic (medicinal) and recreational purposes throughout history Opium Poppy (Papaver somniferum) Opioid receptors In the 1970s pharmacologists identified a number of ‘endogenous’ (within the body) opioids known as enkephalins and endorphins Found to have a role in pain perception, mood and a number of other physiological functions Also discovered opioid receptors in key areas of the body e.g. brain, spinal cord, gut, eye etc. Receptor Interactions Only substances with a similar chemical structure to morphine can attach to opioid receptors (‘key-lock’ analogy) These substances are called opioid agonists – when they attach to the opioid receptors they trigger certain responses Effects of Opioids (Morphine etc.) Relief of pain (analgesia) – main therapeutic use Mood elevation (euphoria) Sedation Constriction of pupil (miosis) Reduction in gut motility (constipation) Suppress cough (anti-tussive) Tolerance to effects, and dependence in some individuals with repeated doses Respiratory depression leading to death in overdose A Mix of Desirable and Unwanted Effects Because there is a variety of opioid receptors in different parts of the body, it is very difficult to separate desirable and unwanted effects of morphine and other opioid drugs Example – all patients receiving morphine or codeine for ongoing treatment of cancer pain become very constipated But, these drugs can also be used as anti-diarrhoeals! Opioid Antagonists Some chemical substances can attach to the opioid receptors and just ‘occupy’ them without triggering an effect These ‘antagonists’ prevent access of the receptor to endogenous chemicals and drugs Naloxone (Narcan®) is an opioid antagonist. It is used to ‘block’ the effects of morphine etc. and will reverse respiratory depression caused by high doses of morphine Receptor sites Where are receptors (drug targets) found? - Cell membranes – usually associated with ion channels, transducer proteins or enzymes - Cell nucleus - Enzymes (many vitamins are co-factors) - Carrier molecules Agonists and Antagonists Most conventional drugs are ‘agonists’ i.e. stimulate receptors or ‘antagonists’ i.e. block receptors For example, salbutamol (Ventolin®) is a beta-receptor stimulant; stimulation of beta-receptors in the lungs causes bronchodilation Metoprolol (Betaloc®) is a beta-receptor antagonist (‘blocker’); blockade of beta-receptors in the heart will slow rate and be ‘cardiprotective’. Note that by blocking the beta-receptors in the lungs ‘beta-blockers’ can cause bronchoconstriction in asthmatics etc. Mechanism of Action of Minerals/Vitamins/Supplements Not classic agonists/antagonists at specific receptors Generally, they are replacing or supplementing body stores, or enhancing effects in certain diseases and disorders Generally, they are co-factors or essential elements in normal metabolic and physiological processes You will already have much more knowledge than us of specific actions and effects Pharmacokinetics “What the body does to the drug” Usually described by the acronym ADME: - Absorption - Distribution - Metabolism - Excretion NB we do not expect dietitians to be experts in pharmacokinetics but to understand some of the basic principles that are commonly used in prescribing Absorption Refers to the processes whereby the drug reaches the bloodstream (systemic circulation) Other than by the intravenous route, or for agents designed to have a direct local effect, drugs must first be absorbed into the circulation before they can be distributed to the site of action Absorption cont. Requires the drug to pass through cells and cell membranes to reach the bloodstream (e.g. in g.i. tract, across the skin, across mucous membranes etc.) Cell membranes are comprised of phospholipids and are essentially lipid (fatty) sheets In general, drugs must be in a lipid-soluble form in order to be absorbed (there are exceptions including minerals and some vitamins) Factors Influencing Oral Absorption We concentrate on oral absorption because it is the main route of drug delivery, but the same basic principles apply to other routes Mechanisms of Drug Absorption (Gastrointestinal Tract) Passive diffusion (major mechanism): lipid-soluble drugs will passively diffuse across membranes on a concentration gradient e.g. fat soluble vitamins A, D, E, K Active transport: for a small number of drugs using carrier molecules in the membrane – can work against a concentration gradient (for example Vitamin B12, iron) Filtration through pores (especially for small water soluble molecules such as glucose, ions such as sodium, magnesium etc.) First Pass Metabolism Extent of metabolism that occurs before drug enters the systemic circulation. Includes metabolism in the gut lumen, gut wall, and lungs; main site, however, is the liver All blood from g.i. tract drains through the portal vein to liver before it reaches systemic circulation (‘firstpass’) First-pass and other pre-systemic metabolism is a very important determinant of oral bioavailibility especially for lipid soluble drugs (see later) Distribution Distribution describes the reversible transfer of drug from the bloodstream to the various other tissues and organs of the body Water-soluble vitamins and minerals will rapidly distribute to the extracellular fluid and be taken up by cells. Lipid-soluble vitamins will follow passive diffusion (as for absorption) Distribution cont. Like absorption, most drugs follow passive diffusion along a concentration gradient Diffusion as reversible: when tissue levels of the drug exceed those in ECF and circulation, then the drug will passively diffuse back to the bloodstream Distribution cont. Extent of distribution also depends on: - the perfusion of the tissue (circulation) – well perfused tissues generally no problems with distribution - the existence of any ‘special’ physiological barriers (e.g. blood-brain barrier) Distribution: Special Barriers ‘Blood-brain barrier’ excludes a number of drugs, esp. more water soluble e.g. dopamine, atenolol, some water soluble-vitamins BBB not a discrete anatomical structure but specialised collection of cells in CNS with ‘tight junctions’ that exclude certain substances Highly Lipid-soluble drugs penetrate BBB readily Distribution: Special Barriers contd. Cerebrospinal fluid (CSF) normally impenetrable to antibiotics (e.g. penicillins) – except when inflamed Some tissues have poor perfusion e.g. bone and nails – for example very difficult to treat infections Metabolism (Biotransformation) Alteration of a drug by the body to one or more chemically different molecules termed metabolites Regulated by enzymes in many tissues e.g. gut, skin, lungs, but predominant organ of metabolism is the liver Metabolism Main purpose of metabolism is to prepare the molecule for excretion (i.e. make it more water-soluble) For minerals and water-soluble vitamins metabolism may not be required, they are excreted unchanged Phase 1 Metabolism Chemical conversion to a metabolite by hydrolysis, reduction, oxidation etc. Most metabolites are inactive pharmacologically, however some drugs may produce active metabolites Some inactive drugs may produce an active metabolite (known as ‘pro-drugs’) Phase 2 Metabolism Phase 2 is addition of another chemical structure by conjugation (joining together) e.g. glucuronic acid, sulphate (example morphine glucuronide) These conjugates are very water-soluble Conjugation increases the water solubility of the drug and prepares it for excretion Metabolism contd. Most drugs undergo both Phase 1 and Phase 2 metabolism to produce a range of metabolites However, some may undergo only Phase 1 or Phase 2 Some drugs may be excreted unchanged (i.e. without biotransformation) – especially if they are already water-soluble e.g. atenolol and of course many vitamins (e.g. Vitamin C) and minerals Excretion (Kidney) Some drugs excreted via lungs, skin etc., but main organ of excretion is the kidney Three phases of drug removal from the blood via the kidney: - filtration at the glomerulus - active secretion into the proximal tubule - passive diffusion (reabsorption) from urine back to blood along the length of the renal tubule Excretion contd. Most drugs and metabolites are filtered at the glomerulus and enter the filtrate in the nephron Some drugs are not filtered but may meet the requirements for active secretion from the arterioles into the nephron at the proximal tubule If filtered drug or metabolite is lipid soluble, it is reabsorbed back into the bloodstream by passive diffusion; if it is water soluble it is excreted in urine PHARMACOLOGY Pharmacokinetics Pharmacodynamics HOW BODY ACTS ON DRUG HOW DRUG ACTS ON BODY Dose of Drug •Absorption •Distribution •Metabolism •Elimination Body concentration over time Drug effect •Receptor Binding •Biological Effect