2. Nursing Diagnosis
advertisement

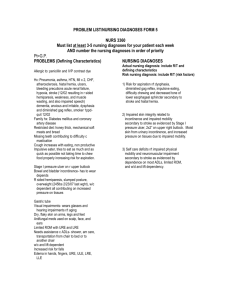
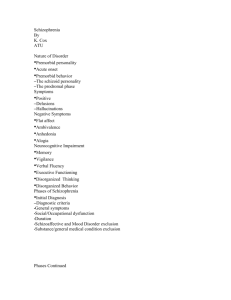
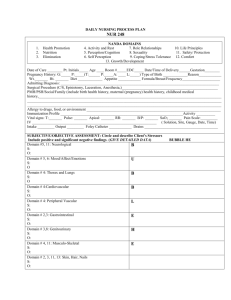
Nursing Diagnosis Nursing diagnoses? What’s up with that? Nursing diagnoses are what you get when you finish your assessment and look at your data. Nursing diagnoses describe patient needs or responses to health conditions and treatments Nursing diagnoses reflect the patient’s level of health or response to disease, emotional state, socio-cultural phenomenon, or developmental stage Medical vs. nursing diagnoses Medical diagnosis- Identifies disease or pathology Nursing diagnosis- Identifies patient’s response to said disease or pathology Medical diagnosis goal- to cure the disease Nursing diagnosis goal- to direct the nursing plan of care to meet the patient’s needs Nursing diagnoses Help facilitate communication between members of the nursing staff Help prioritize the needs of the patient Help to guide charting In practice, you… Do your assessment and think “My patient is in pain!” Take your impressions and put fancy labels on them like “impaired comfort” or “acute pain” Those are nursing diagnoses in a nutshell When I’m at work… The first thing I do is get report on my patients- from the ER or the previous nurse As I am getting report, I am thinking about what I will have to keep in mind when I am caring for my patients… For a postop patient, I might be thinking: Check on pain Check the lungs- potential for pneumonia or atalectasis Check for constipation from narcotic pain meds Check the incision Check if the patient has been out of bed yet Then off to see the patient… When I go to do my assessment on the patient, I keep all those things in mind… I talk to the patient to see: Then I do a physical assessment to check on: How the pain is doing When the last BM was If she has been out of bed yet Lungs- check for diminished breath sounds or fluid Incision- check for redness or drainage Legs- check for clot When I am done, I consider all of my findings and come up with some conclusions… And I come up with… The patient is in a fair amount of pain- I need to give her some pain medication ASAP Her lungs are clear but there is still the potential for pneumonia She has not had a BM in 3 days- pain medications are getting her constipated The incision looks OK- no signs of infection The patient got out of bed last night and sat in the chair, but needs to ambulate To turn these findings into nursing diagnoses… I check the NANDA list to see what fits my findings… My patient is in pain- that could be “impaired comfort” or “acute pain” She doesn’t have pneumonia right now, but she’s still at risk for it- that could be “potential impaired gas exchange” No BM in 3 days- sounds like “constipation” to me! Her incision is OK but it could still become infected- how about “risk for infection” She’s not moving so well- “impaired physical mobility” might work. “Risk for falls” might be good, too, since she’s taking narcotic pain medicines To write or not to write? When I work with patients in the hospital, I formulate nursing diagnoses for my patients in my head automatically as I am getting report and doing my assessments I also refer to the nursing care plan in the patient’s chart to see what other nursing diagnoses have been selected by the staff Nursing students get to write everything out- to show the instructor and help it become second nature in practice after graduation At clinical, you will… 1. Get report on your patients first 2. Go meet with your patients and do a physical assessment 3. Formulate your nursing diagnoses 4. Develop a care plan based on your assessment and nursing diagnoses You got to stick with NANDA! Unfortunately, you are not allowed to make up new and creative nursing diagnoses for your patients No matter how much your patient merits a nursing diagnosis of “persistent stupidity” or “constant whining” you just can’t do it! Some authors like Carpenito have developed nursing diagnoses similar to NANDA’s, they will be acceptable at our university, but NANDA will be preferred. Writing nursing diagnoses The first part is the NANDA nursing diagnosis statement If your patient doesn’t meet the criteria for the diagnosis yet, you put “Risk for…” in front of the diagnosis Risk for nausea Risk for deficient fluid volume After the diagnosis, you put why you chose the diagnosis for the patient with a “related to” (R/T) statement… Risk for nausea R/T side effects from chemotherapy medications Risk for deficient fluid volume R/T poor fluid intake and high temperature Sleep deprivation R/T busy ICU environment For my earlier postop patient: Acute pain R/T tissue damage from surgical incision Potential impaired gas exchange R/T shallow breathing postoperatively Constipation R/T slowed bowel motility from narcotic pain medications and bed rest Risk for infection R/T new surgical incision Impaired physical mobility R/T postoperative weakness Risk for falls R/T dizziness from narcotic pain medications “Related to” statements Should be within the scope of nursing practice, not medical practice (like a medical diagnosis or treatment) Related to statements should include information such as: Symptoms or situations that can be addressed with nursing care Patient responses to diseases or conditions Treatments that can be performed by a nurse Developmental or maturational stages Writing “related to” statements Don’t put medical diagnoses or diagnostic tests like pneumonia, hip fracture, or angioplasty in the “related to” statement. Do put factors that you can take care of with nursing interventions… BAD Impaired gas exchange R/T increased blood CO2 levels BETTER!! Impaired gas exchange R/T shallow breathing postop Diarrhea R/T C. difficile infection Diarrhea R/T food intolerance Acute pain R/T hip fracture Acute pain R/T swelling and tissue damage More examples… Bad Good Why?? Risk for aspiration Risk for aspiration R/T stroke R/T impaired swallowing Nurses can work with patients to improve swallowing ability Acute pain R/T hip Acute pain R/T fracture tissue damage and swelling in right hip Nurses can give medications to help relieve pain from tissue damage, and provide ice to reduce swelling Risk for falls R/T Multiple Sclerosis Nurses can help patients with transfers to compensate for poor balance and weakness Risk for falls R/T poor balance and leg weakness After the R/T statement… After you say why you chose the diagnosis for the patient with the “related to” statement, include an “as evidenced by” statement that includes specific signs and symptoms of the particular patient This step is not needed when there is only “Risk for …” diagnoses, as the patient is only at risk for the condition and has not actually developed it yet You can use “AEB” for “as evidenced by” so that you don’t need to write it out Some examples from my postop patient… Acute pain R/T tissue damage from surgical incision, AEB patient reports of pain rating of 8 on 1-10 scale, visible grimacing with movement Constipation R/T slowed bowel motility from narcotic pain medications and bed rest, AEB no BM for 3 days Impaired physical mobility R/T postoperative weakness, AEB patient unable to move from bed to chair without assistance AEB statements Don’t include prejudicial statements such as: Risk for impaired skin integrity R/T poor hygiene habits, AEB foul stench from perineal area Instead, you could use: Risk for impaired skin integrity R/T inability to reach perineal area to clean, AEB patient verbalized need for nursing assistance with perineal care Diagnostic testing… Don’t use diagnostic tests specifically in nursing diagnoses like: Anxiety R/T cardiac catheterization, AEB patient statements of uneasiness and nervously pacing floor Instead, focus on patient responses to the tests: Anxiety R/T awaiting of cardiac catheterization results, AEB patient statements of uneasiness and nervously pacing floor Phrasing diagnoses Don’t use blaming phrases or ones that could imply negligence or malpractice, like: Excess fluid volume R/T IV infused too quickly Acute pain R/T improper placement of epidural catheter Don’t overload diagnoses… Constipation and abdominal pain should be 2 different nursing diagnoses Noncompliance and knowledge deficit should be 2 different diagnoses