Foot Ankle Unit PPT
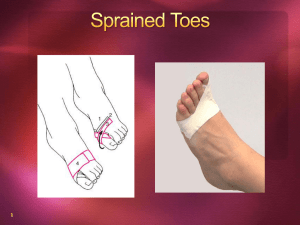
advertisement

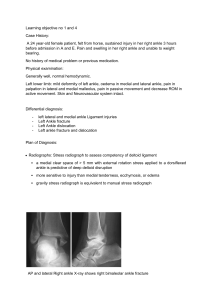
Foot/Ankle Unit SKELETAL ANATOMY Lower Leg Bones • Tibia – Shin Bone – Weight bearing bone in the lower leg – Medial Malleolus: • Distal end of tibia that forms the medial ankle bone • Fibula – Non-weight bearing bone – Lateral Malleolus: • Distal end of fibula that forms the lateral ankle bone Foot Bones • Tarsals (7) – – – – Talus Calcaneus Cuboid Cuneiforms • (medial, middle, lateral) – Navicular • Metatarsals (5) • Phalanges (14) – Proximal – Middle – Distal Joints • Ankle: – Distal Tibiofibular – Talofibular – Talocrural • Foot: – Intertarsal – Tarsalmetatarsal • Toes: – Metatarsalphalangeal – Proximal Interphalangeal – Distal Interphalangeal Ligaments • Lateral – Anterior Talofibular (ATF) – Calcaneofibular (CF) – Posterior Talofibular (PTF) • Medial – Deltoid • High – Anterior Tibiofibular SOFT TISSUE ANATOMY Terminology • Plantarflexion (PF): – Ankle movement in which foot moves toward ground and toes are pointed to the ground • Dorsiflexion (DF): – Ankle movement in which toes/dorsum of foot moves upwards towards knee • Origin: – Where muscle originates and attaches to bone • Insertion: – Where muscle attaches, usually distally, and where movement occurs Movements/Actions • Foot/Ankle: – – – – Inversion (inv) Eversion (ev) Plantarflexion (PF) Dorsiflexion (DF) • Toes: – – – – Flexion (flex) Extension (ext) Abduction (abd) Adduction (add) Muscles • The muscles for the foot and ankle are in muscle groups on the lower leg. • There are four main groups – Anterior – Posterior – Medial – Lateral Posterior Muscles Muscle Origin Insertion Action Gastrocnemius Distal Femur Calcaneus PF and Knee Flexion Soleus Posterior tibia & fibula Calcaneus PF Posterior Muscle Diagram Anterior Muscles Muscle Origin Insertion Function/Action Tibialis Anterior Tibia Medial cuneiform & DF and slight 1st metatarsal inversion Extensor Hallicus Longus Fibula Dorsal surface of big toe Extensor Digitorum Longus Tibia & Fibula DF and inv of ankle, extends 1st digit DF and eversion, extends toes 2-5 Anterior Muscles Diagram Medial Muscles Muscles Origin Insertion Function/Action Tibialis Posterior Posterior Tibia Navicular, cuneiforms, cuboid/metatarsals 2-4 PF and inversion Flexor Digitorum Longus Posterior Tibia Dorsal surface of PF and inv, flexes distal phalanges 2-5 toes 2-5 Flexor Hallicus Longus Fibula Dorsal surface of 1st PF and inversion, distal phalanx flexes big toe Medial & Lateral Diagram Lateral Muscle Diagram Lateral Muscles Muscle Origin Insertion Function/Action Peroneus Longus Fibula Dorsal surface of 1st Eversion & PF metatarsal and medial cuneiform Peroneus Brevis Fibula Proximal 5th metatarsal Eversion & PF SPRAINS Ankle Sprains • Single most common injury in the physically active caused by sudden inversion or eversion moments • There are 3 types of Ankle Sprains: – Inversion • Also called a Lateral ankle sprain • Most common and result in injury to the lateral ligaments – Eversion • Also called a Medial ankle sprain • Least common due to anatomical structures, medial malleolus – Syndesmotic • Also called a High ankle sprain Ankle Sprains The following chart shows the mechanism of injury or MOI for each type of sprain according to the ligament that is injured. Lateral Medial High ATF: PF and Inv Deltoid: DF and Eversion Ant. Tibiofibular: Excessive DF or PF CF: Inv PTF: Severe inversion or dislocation (rare) Ankle Sprain Grades & Types Ankle Sprain: S/S • General S/S for all types of sprains: – Swelling – Pain with WB (weight bearing) – Instability – Ecchymosis (bruising/discoloration) • Stress Test Positives: – Anterior Drawer Test- ATF ligament – Talar Tilt Test- CF and Deltoid ligaments – Kleiger’s Test- Tib/fib ligament Ankle Sprains: Rx • General Acute Care: – RICE with horseshoe – NSAIDs – Crutches? • Usually for a grade 2 and up – Referral Toe Sprains •Sprained Toes – MOI: • Generally caused by kicking non-yielding object • Pushes joint beyond normal ROM or imparting a twisting motion on the toe- disrupting ligaments and joint capsule – S/S: • Pain is immediate and intense but short lived • Immediate swelling and discoloration occurring w/in 1-2 days • Stiffness and residual pain will last several weeks – Rx: • RICE, buddy taping toes to immobilize • Begin weight bearing as tolerable Turf Toe •Great Toe Hyperextension (Turf Toe) – MOI: • Hyperextension injury resulting in sprain of 1st metatarsophalangeal joint • May be the result of single or repetitive trauma – S/S: • Pain and swelling which increases during push off in walking, running, and jumping – Rx: • • • • Increase rigidity of forefoot region in shoe Taping the toe to prevent dorsiflexion Ice and ultrasound Rest and discourage activity until pain free ACUTE INJURIES Muscle Strains • MOI: – Due to violent contraction/twisting of foot – Awkward landing • S/S: – – – – Pain with ROM or RROM Possible pain with WB Swelling or crepitus May feel like being “hit in leg with a stick” • Rx: – RICE – Taping/bracing – Monitor for acute compartment syndrome Achilles Tendon Rupture • Occurs w/ sudden stop and go; forceful plantar flexion w/ knee moving into full extension • Commonly seen in athletes > 30 years old – Can be observed at any age • Generally has history of chronic inflammation Achilles Tendon Achilles Tendon Rupture • S/S: – Pain/inability to plantarflex – Feels like they were “kicked in calf” – Positive Thompson Test – Deformity • Rx: – RICE – Referral is rupture is suspected Contusion • MOI: – Direct blow or crush of the muscle fibers • S/S: – Ecchymosis, bruise may develop – Limited ROM; pain, weakness and partial loss of limb function – Palpation will reveal hard, rigid, inflexible area due to internal hemorrhaging and muscle guarding • Rx: – Stretch to prevent spasm; apply cold compression and ice – Wrap or tape will help to stabilize the area; padding to protect the area – Monitor for Acute Compartment Syndrome Leg Cramps and Spasms • Sudden, violent, involuntary contraction, either clonic (intermittent) or tonic (sustained) in nature • MOI: – Difficult to determine; fatigue, loss of fluids, electrolyte imbalance, inadequate reciprocal muscle coordination • S/S: – Cramping with pain and contraction of calf muscle • Rx: – Try to help patient relax to relieve cramp – Firm grasp of cramping muscle with gentle stretching will relieve acute spasm – Ice will also aid in reducing spasm – If recurrent may be fatigue or water/electrolyte imbalance FRACTURES AND DISLOCATION INJURIES Dislocations • Rare in ankle, but common in phalanges • MOI: • Traction or twisting • S/S: • • • Deformity Possible fractures Inability to move extremity • Rx: • • • Immobilize Cold Referral for reduction or Emergency Action Plan (EAP) Types of Acute Fx • Avulsion Fractures – Common for ATF Ligament to fracture lateral malleolus (looks like 3rd Degree sprain) – Jones Fracture- Peroneus brevis pulls off proximal 5th metatarsal with forced inversion • Growth Plate (Epiphyseal) Fractures – Distal plated in fibula and tibia may fracture with inversion/eversion Acute Fractures • MOI: • • • Direct blows Twisting Associated with avulsions/dislocations • S/S: • • • • • • Localized Pain Deformity? Swelling Ecchymosis Crepitis Pain with WB Acute Fractures • Stress Tests: – Tap Test (Percussion)- tibia, fibula, talus or calcaneus – Calf Squeeze (Compression)- tibia or fibula • Rx: – RICE – X-ray, reduction, casting up to 6 weeks depending on the extent of injury – Be prepared to activate Emergency Action Plan (EAP) if open fracture or signs of shock Types of Stress Fx • March Fracture – Stress Fracture to the metatarsals due to repetitive activity • Most commonly the 2nd metatarsal • Tibial or fibula Stress Fracture – Common overuse condition, particularly in those with structural and biomechanical insufficiencies – Runners tends to develop in lower third of lower leg (dancers middle third) Stress Fractures • Extremely common due to repetitive action • General Management: – S/S: • point tenderness; especially in WB position – Rx: • NWB (non-weight bearing) > week or more • Walking boot or cast possible • Out of activity 3-4 weeks • Gradual resumption of activity OTHER INJURIES Compartment Syndrome • A painful and dangerous condition caused by pressure buildup from internal bleeding or swelling of tissues. – The pressure decreases blood flow, depriving muscles and nerves of needed nourishment. • Acute compartment syndrome – Occurs secondary to direct trauma – Medical emergency • Acute exertional compartment syndrome – Evolves with minimal to moderate activity • Chronic compartment syndrome – Symptoms arise consistently at certain point during activity Compartment Syndrome Acute Compartment Syndrome • MOI: direct blow or tearing of muscle fibers causing swelling • S/S: – Pain becoming worse; eventually numbness – Loss of foot ROM – Leg swelling • Rx: Medical Emergency! Refer Immediately – Apply cold and elevate – Surgical intervention is probably necessary Plantar Fasciitis • MOI: – – – – – – Shoes Overweight Activity on hard surfaces Overuse Poor mechanics Fatigue • S/S: – Morning pain – Swelling – Pain with WB – Crepitus • Rx: – – – – – Good shoes/orthotics Stretching Ice Taping Referral? Arches •Pes Planus Foot (Flatfoot) – MOI: • Associated with excessive pronation, forefoot varus, wearing tight shoes (weakening supportive structures) being overweight, excessive exercise placing undo stress on arch •Pes Cavus (High Arch Foot) – MOI: • Higher arch than normal; associated with excessive supination, accentuated high medial longitudinal arch Morton’s Toe Vs Neuroma •Morton’s Toe – Etiology • Abnormally short 1st metatarsal, making 2nd toe look longer • More weight bearing occurs on 2nd toe as a result and can impact gait • Stress fracture could develop •Morton’s Neuroma – Etiology • Thickening of nerve sheath (common plantar nerve) at point where nerve divides into digital branches • Commonly occurs between 3rd and 4th met heads; medial and lateral plantar nerves come together • Irritated by collapse of transverse arch of foot, putting transverse metatarsal ligaments under stretch, compressing digital nerves and vessels Shin-Splints • Shin-splints is a catch-all term for tendonitis, chronic compartment syndrome or a stress fracture • Medial Tibial Stress Syndrome (MTSS) is the more appropriate term for shin-splint-type pain Shin-Splints • MOI: – Pes planus (flat feet) – Overweight – Poor conditioning – Poor shoes – Activity on hard surfaces – Overuse/Muscle weakness – Poor running technique – Genetics Shin-Splints • S/S: – Pain is usually found on medial side of leg – Pain with activity that gets progressively worse over time • Rx: – – – – – RICE before/after Check shoes, running shoes are only good for 500 miles Stretch, Strengthen, Cross Train NSAIDs Refer for fracture or compartment syndrome EVALUATIONS Evaluation: The Why • The athlete’s well-being WILL depend on the accuracy and thoroughness of your Soap! • Ask probing questions and record accurately • The aim of the examination process is to provide an efficient and effective exchange, and to develop a rapport between the clinician and patient • The information gathered is used to provide the athlete with the best care and to provide a record of what has been done, for medical and legal purposes. HOPS • History: – A series of questions asked to determine nature and location of injury • Observation: – A visual examination of the injury • Palpation: – A hands-on approach where examiner feels for deformity or other abnormal findings • Stress tests: – A series of tests to check range of motion and degree of function of tissues at a joint SOAP Note Format • Subjective: – Detailed information about the history of injury and athlete; chief complaints, sign, and symptoms • Objective: – Information that is a record of test measurements; the data gained from inspection • Assessment: – Identification of the problem; identify the injury and the severity of it • Plan of Action: – What are you going to do; the immediate treatment, rehab, or referral Active Listening Skills The following skills should be used during a evaluation to help you gather information and gain the athletes trust: 1. 2. 3. 4. 5. 6. 7. Face the speaker; lean slightly forward Maintain eye contact Minimize external/internal distractions Respond appropriately Focus solely on what the speaker is saying Keep an open mind Avoid giving advice until you have completely evaluated injury 8. Don’t interrupt 9. Stay engaged in the interview Subjective: Oral/Verbal Info • General Questioning Prompts: – – – – – – – – Was there a previous injury? How did it happen? When did it happen? What did you feel? How do you feel? What is the type of pain? Where does it hurt? Did it make a sound? * Ask for a witness if the person is incapable of answering Objective: Visual Inspection • Look for the following: – Swelling – Deformity: • protrusions – Ecchymosis: • Discoloration – Symmetry – Gait: • Walk – – – – – Scars Facial expressions Bleeding Depressions ROM Objective: Hands-On Format • • • • Perform Palpation Check anatomical structures to determine points of pain Check for abnormalities Preform special test or stress tests to assess severity – Stress Tests: • • • • • • Anterior Drawer Test – ATF Ligament Talar Tilt Test – CF Ligament Kleiger’s Test Thompson Test – Achilles Tendon Rupture Tap (Percussion) Test – Fracture test Calf Squeeze (Compression) Test – Fracture Test – Manual Muscle testing (RROM) • Dorsiflexors/Plantarflexors • Toe flexors/extensors • Inverters/Everters RETURN TO PLAY Terminology • Therapeutic: – Healing action Phase I: Pain Management • The time immediately following the injury or surgery, in which movement is limited to ease pain • Areas of Importance: –Pain control –Decrease inflammation –RICE Phase II: ROM • Time when therapeutic action initiated includes; joint range-of-motion, mobility and flexibility exercises • Areas of Importance: –PROM: •passive rom •AAROM: •active assisted rom •AROM: •active rom •Flexibility Phase III: Balance • PROPRIOCEPTION (Balance) – The body relearning the ability to sense the position of its limbs during movement; includes balance • Areas of Importance: – Balance exercises – Coordination exercises Phase IV: Strength • To increase muscular strength • Areas of Importance: – Emphasize the injured area, but maintain whole body strength Phase V: Endurance • For both the cardiovascular and muscle systems to perform work over a period of time • Areas of Importance: – High amount of repetitions with low weight – Full-body cardiovascular endurance Phase VI: Sport Specific • Where the athlete mimics specific sport-like or functional activity. This leads to full resumption of activity. • Areas of Importance: •Gradual resumption of activity •Limited or restrictive moving towards full resumption