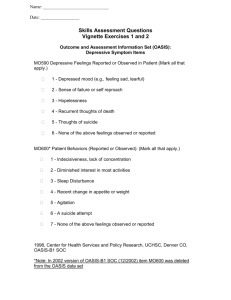
MOOD DISORDERS
advertisement
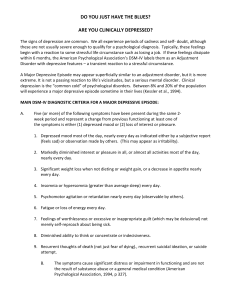
MOOD DISORDERS Epidemiology Sex: MDD F:M = 2:1 BID F=M Age: onset - BID is earlier (30 yo) than MDD (40yo) Marital Status: MDD - no close interpersonal relationships, divorced, separated BID - single/divorced > married SE & Cultural Considerations Etiology 1. Biological Factors: abN in biogenic amine metabolites (5-HIAA, HVA, MHPG) Biogenic Amines - NE, 5HT, DA, GABA 2. Neuroendocrine regulations 1. 1. Hypothalamus 1. 2. 3. Adrenal axis Thyroid axis Growth hormone 3. 4. 5. 6. 7. 8. Sleep Abnormalities - EEG abN Kindling Circadian Rhythm Neuroimmune Regulations Brain Imaging - CT scan, MRI Neuroanatomical Considerations - limbic system, basal ganglia, hypothalamus 2. Genetic Factors - BID > MDD 1. 2. 3. 3. Family Studies Adoption Studies Twin Studies Psychosocial Factors 1. 2. 3. 4. 5. Life events & Environmental stress Premorbid Personality Factors Psychoanalytic & Psychodynamic Factors Learned Helplessness Cognitive Theory Diagnosis Major Depressive Disorder – – – – – – – – – – Depressed mood Loss of interest or pleasure Weight loss or gain Insomnia/hypersomnia Psychomotor agitation or retardation Fatigue or loss of energy Feelings of worthlessness or inappropriate guilt Diminished ability to think or concentrate Recurrent thoughts of death Sxs cause significant distress or impairment Manic Episode – – – – – – – – Elevated, expansive, or irritable mood Inflated self-esteem or grandiosity Decreased need for sleep More talkative Flights if ideas Distractibility Psychomotor agitation Excessive involvement in pleasurable activities Clinical Features Depressive Episodes – Depressed mood: feel blue, sad, hopeless, worthless – Agonizing emotional pain – 2/3 contemplate suicide – 10 - 15% commit suicide – 97% - reduced energy – 80% - sleep disturbance – Decreased appetite – 90% - anxiety Atypical Features – Hysteroid Dysphoria – Increased appetite – Weight gain – Hypersomnia Depression in Children and Adolescents – – – – – – – School phobia Poor academic performance Substance abuse Antisocial behavior Sexual promiscuity Truancy Running away Depression in the Elderly – More common - 25-50% – More somatic complaints Manic Episodes – – – – – Elevated, expansive, irritable mood Infectious Disinhibited Impulsive Preoccupied by religious, political, financial, sexual or persecutory ideas Manic in Adolescents – Misdiagnosed as antisocial PD or schizophrenia – Psychosis, substance abuse, suicide attempts, academic problems, somatic complaints, irritability Co-existing Diagnosis 1. 2. 3. 4. Anxiety Alcohol dependence Other substance-related disorder Medical conditions Mental Status Examination Depressive Episodes General Description - retardation, agitation 2. MAF - depression 3. Speech - decreased rate and volume 4. Perceptual Disturbances 1. 1. 2. 3. 4. With perceptual disturbances Psychotic depression Mood-congruent Mood-incongruent 5. Thought - negative view of the world and themselves 1. 2. Content - loss, suicide, guilt, death Thought blocking 6. Sensorium and Cognition Memory: 50-75% depressive dementia Impaired concentration & forgetfulness 7. Impulse Control 10-15% - complete suicide 2/3 cases - suicide ideation Paradoxical suicide 8. Judgment and Insight excessive insight 9. Reliability poor Manic Episodes General Description - excited, talkative, hyperactive 2. MAF - euphoric, irritable, angry, hostile, labile 3. Speech - disturbed, loud, rapid, pressured 4. Perceptual disturbances - 75% delusional 1. 5. Thought 1. 2. 3. Content: self-confidence, selfaggrandizement Form: looseness of association, flight of ideas, word salad, neologisms Cognitive function: unrestrained, accelerated flow of ideas 6. Sensorium and Cognition orientation and memory intact 7. Impulse Control - 75% assaultive and threatening attempt suicide and homicide 8. Judgment and Insight impaired judgment - hallmark little insighht 9. Reliability notoriously unreliable lying and deceit Differential Diagnosis MDD 1. 2. Medical Disorders - medications, neurological conditions Mental Disorders 1. 2. 3. 4. Mood DO due to General Medical Condition Substance-Induced Mood DO Other Mental DO - SRD, psychotic DO, eating DO, adjustment DO, anxiety DO, somatoform DO Uncomplicated Bereavement BID Medical DO 2. Mental DO - BIID, cyclothymia, Mood DO due to General Medical Condition, Substance-Induced Manic episode, Borderline PD, Narcissistic, Histrionic, Antisocial PDs, Schizophrenia 1. Course and Prognosis Chronic, tend to have relapses MDD Course – – – – – Onset: 50% before age 40 years Duration: untreated 6-13 months treated 3 months Development of manic episodes: 5-10% with initial diagnosis MDD have manic episode 6-10 years after Mean age of switch = 32 years old – Prognosis: chronic, tend to relapse Indicators: GOOD - mild episodes, (-) psychosis, short hospital stay, (+) social support, (-) comorbidity, advanced age of onset POOR - co-existing dysthymic DO, abuse of alcohol and other substances, anxiety DO sxs, hx of more than one episode of depression BID Course – Most often starts with depression – Recurring disorder – Manic episode has rapid onset – Prognosis: poorer prognosis than MDD 40-50% have 2nd manic episode within 2 years 50-60% are controlled with lithium Indicators: GOOD - short duration, advanced stage of onset, few suicidal attempts, few coexisting psych or medical problems POOR - poor occupational status, alcohol dependence, (+) psychosis, depressive features, males Treatment GOALS Safety of the patient 2. Complete diagnostic evaluation 3. Treatment plan 1. Treatment must reduce the number and severity of the stressors in patients’ lives Hospitalization 1. • Indications: prognostic procedures risk of suicide and homicide grossly regressed Psychotherapy 2. • Short-term psychotherapy: cognitive, interpersonal, bahavior 3. Pharmacotherapy – – – MDD: 3-4 weeks principal indication: major depressive episode Patient education Alternatives to Drug Therapy: ECT and phototherapy ECT: unresponsive to pharmacotherapy cannot tolerate pharmacotherapy severe situations that rapid improvement is needed PHOTOTHERAPY: with seasonal pattern; mild Guidelines: Dosage of antidepressant should be raised to the maximum recommended level and maintained at that level for at least 4 weeks. Duration and Prophylaxis: Antidepressant treatment should be maintained for at least 6 months. – BID: lithium, carbamazepine, valproate Lithium: standard treatment SE: renal, nervous, metabolic, GI, derma, thyroid Anticonvulsants: carbamazepine, valproate Other agents: clonazepam, clonidine, clozapine, verapamil Dysthymic Disorder EPIDEMIOLOGY – Common; 3-5% of all persons – Females (less than 65yo) > men – Frequently coexists with other mental Dos ETIOLOGY 1. Biological Factors 1. 2. 2. Sleep studies Neuroendocrine axis Psychosocial Factors 1. 2. 3. Faulty personal and ego development Defense mechanism: reaction formation Low self-esteem, anhedonia, introversion DIAGNOSIS – Depressed mood most of the time for at least 2 years – (-) manic or hypomanic episodes CLINICAL FEATURES – Chronic – Severity of depressive symptoms is generally less – Sarcastic, nihilistic, brooding, demanding, complaining – (-) psychotic symptoms – Associated symptoms: Changes in appetite and sleep patterns Decreased sexual drive Low self-esteem Loss of energy Psychomotor retardation Pessimism, hopelessness, helplessness Social impairment CO-EXISTING DIAGNOSIS Double Depression - poorer prognosis 2. Alcohol and other substance abuse alcohol, stimulants, MJ 1. DIFFERENTIAL DIAGNOSIS Minor Depressive DO 2. Recurrent Brief Depressive DO 1. COURSE AND PROGNOSIS – 50%: insidious onset before age 25 years – 25%: progressed to MDD – 15%: BIID – <5%: BID TREATMENT – Pharmacotherapy + cognitive/behavior tx Cyclothymic Disorder Mild Bipolar II Disorder Hypomania and mild depression EPIDEMIOLOGY – – – – – 3-10% of all psychiatric patients 1% lifetime prevalence Frequently co-exists with Borderline PD F:M = 3:2 Onset between 15-25 years old (50-75%) ETIOLOGY 1. Biological Factors – 2. Genetic: 30% (+) history of BID Psychosocial Factors – – Trauma and fixation during oral stage Freud: ego attempts to overcome a harsh and punitive superego DIAGNOSIS – CLINICAL FEATURES – – – – Symptoms at least 2 years Less severe symptoms of BID Hypomanic symptoms Mixed symptoms with marked irritability Shorter cycles Substance Abuse: to self-medicate or to achieve further stimulation DIFFERENTIAL DIAGNOSIS Medical and Substance-Related causes of depression and mania 2. Borderline, antisocial, histrionic, narcissistic PDs 3. ADHD 1. COURSE AND PROGNOSIS – – Insidious onset; teens or early 20’s 1/3 go to major mood DO, most often BIID TREATMENT Biological tx: antimanic - LiCO3 2. Psychosocial tx: directed towards patients’ insight and coping mechanisms for their mood swings 1.