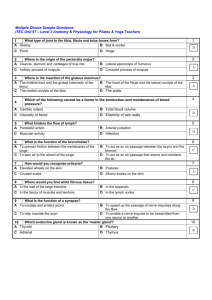
P11_Pediatric_Tibia
advertisement

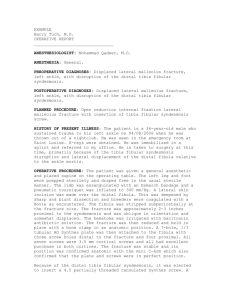
Fractures of the Tibia and Fibula in the Pediatric Patient Steven Frick, MD Created March 2004; Revised August 2006 Growth and Development of the Tibia and Fibula • More growth proximally than distally in both • Fibula moves distally relative to the tibia with growth • Extraphyseal fractures rarely disturb future growth and development (exceptions= proximal tibia, crossunion) Relevant Anatomy • Tibia and fibula bound together by interosseous membrane • Some motion occurs normally (proximal distal translation, inward/outward rotation) at proximal and distal tibiafibular joints • Subcutaneous location of tibia- implications for susceptibility to injury and healing potential Incidence • Low energy fractures common (toddler’s fracture, spiral tibia fractures) • Of open fractures in children, tibia is most frequent location Physical Examination • Integrity of the skin and severity of soft tissue injury • Dorsalis pedis and posterior tibialis pulsers, distal capillary refill • Peroneal and posterior tibial nerve function • Any signs of compartment syndrome Compartment Syndrome • Can occur in skeletally immature patient after closed or open tibia fracture • Tense compartment, pain out of proportion, pain with passive stretch, paresthesias in distribution of nerves that are in compartment • Compartment pressure measurement to confirm • Consider conscious sedation / general anesthesia in child to measure pressures • Fasciotomies emergently if diagnosed Radiographic Evaluation • 2 Orthogonal views usually adequate • Visualize knee and ankle joints • Assess for displacement/displacement/translation, shortening, angulation • Rotation best assessed clinically Classification • Open/Closed • Tibia, Fibula or both • Fracture location- proximal or distal, metaphyseal or diaphyseal • Fracture pattern- transverse, spiral, butterfly, comminuted Decision Making-Principles for Treatment • Restore acceptable length, alignment, translation and rotation • What is acceptable? Little hard date available, depends on age of patient • General guidelines for acceptable position: <10° angulation, <2cm shortening, <50% translation, rotation equal to opposite side • Fractures that heal in positions outside these guidelines may remodel or go on to good clinical result Principles of Treatment • Majority of tibia/fibula fractures in children can be treated closed • Careful attention to casting technique • Radiographic monitoring at regular intervals during early healing- wedge cast, or remanipulate/recast for unacceptable reduction/position Treatment Options • Cast above knee usually, but below knee acceptable for stable fracture patterns or after early healing • Pin fixation and cast- simple and effective, especially in oblique fractures, younger children • External fixation- high energy fractures with associated soft tissue injuries • Flexible nails- proximal medial and lateral insertion • Rigid nail- if near skeletal maturity • Plate fixation- if soft tissues allow Specific Fractures • • • • • • • Toddlers Proximal tibia metaphyseal fracture Isolated fibula fracture Isolated tibia fracture- mid/distal third Open tibia Distal metaphyseal tibia Floating knee Toddler’s Fracture • Very common in young children • Accidental • Stable • Above knee cast with knee flexed 10 degrees for three weeks Proximal Tibia Metaphyseal Fracture • Potential for valgus overgrowth • Usually 3-6 years old when femoral- tibial angle growing towards valgus • Varus mold may prevent • Some believe in completing the fracture • Valgus can be severe but usually remodels over years such that corrective osteotomy unnecessary Valgus after Proximal Tibia Metaphyseal Fracture Asymmetric growth slowdown lines Persistent bow Valgus following Proximal Tibia Fracture Case courtesy of K. Shea. Observe and often improve with time, but may need guided growth surgical intervention Isolated Fibula Fractures • Direct blow mechanism • Immobilize as needed for comfort(fibula 15% of weight bearing) • Carefully assess ankle (r/o Maissenouve injury) Indications for Surgical Treatment • Inability to obtain/maintain acceptable position • Open fractures • Multiple trauma to facilitate mobilization Isolated Tibia Fracture with Intact Fibula • Often at middle/distal third • Muscle forces/biomechanics usually result in drift into varus angulation • Valgus mold in initial cast • Can wedge at 2 weeks but more difficult because of intact fibula Open Tibia Fractures • Soft tissue injuries typically less severe than in adults • Periosteum often intact on concavity • Appropriate debridement, antibiotics • Pins and cast, external fixation, flexible intramedullary rods all useful – choice depends on age, fracture pattern, status of soft tissues, associated injuries • Lower malunion rates and best outcomes seem to be reported after flexible nailing Open Tibia Fracture with Soft Tissue Deficits Appropriate pin placement and construct needed to control varus Open Tibia FracturesI&D, Flexible Nailing Distal Metaphyseal Tibia Fracture • “Gillespie” fracture – apex posterior angulation distal tibia • Dorsiflexion of ankle to neutral may increase apex posterior angulation • Cast in equinus until early healing, then change cast and dorsiflex to neutral Gillespie Fracture – Healed in Excessive DF as was Casted with Ankle at Neutral Pinning and Cast after Failure to Achieve Acceptable Alignment with Closed Methods Floating Knee Injuries • Ipsilateral femur and tibia fractures • Typically high energy mechanism • Operative stabilization of at least one of fractures recommended • Often may treat femur operatively and tibia nonoperatively • If both displaced / unstable recommend fixation of both 12 Year Old, Pedestrian vs. Car Floating Knee Healed Floating Knee Expected Outcomes • Usually heal in 6-12 weeks in juveniles/adolescents • Nonunions rare • Malunion- no accepted definition, later adverse of malunion poorly documented • Remodeling potential- especially for metaphyseal fractures in younger patients Tibia Fracture Malunion/Nonunion Varus – procurvatum malunion following premature removal of ex fix after open tibia fracture Isolated Tibia Fracture Casted with Valgus Mold – Healed with Excellent Alignment If you would like to volunteer as an author for the Resident Slide Project or recommend updates to any of the following slides, please send an e-mail to ota@aaos.org E-mail OTA about Questions/Comments Return to Pediatrics Index