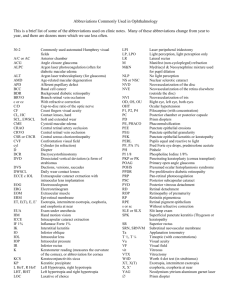
Intraocular Assessment
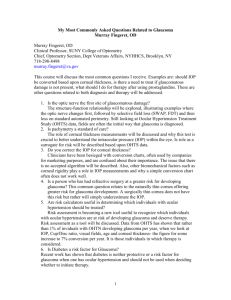
advertisement

Intraocular Assessment Anterior Chamber Anatomy o Most of the anterior chamber is visible with the unaided eye and easily seen with the biomicroscope. The anterior boundary of the fluid-filled chamber is the posterior surface of the cornea and a small lip of the sclera. The posterior boundary is the anterior surface of the iris and the papillary portion of the anterior lens. the peripheral margin demonstrates an angle between the sclera at the edge of the corneal dome and the floor of the chamber. Deepest centrally, the chamber narrows approaching the peripheral margin. A clear fluid, the aqueous humor, fills this chamber, about 0.2ml. o Location Space between the anterior surface of the iris and the cornea/ sclera o Depth 3.54mm. This is larger than the corneal vault, which is about 2.6mm Decreased arc Trends o Due to the lengths of the eyes, myopes have a deeper anterior chamber and hyperopes have a shallower anterior chamber. o The anterior chamber becomes more shallow with age due to the thickening of the lens, pushing the iris forward. o These are important to know with dilation and angle closer glaucoma. Filtration Angle o This angle is at the peripheral margin and is a U-shaped structure foemd by the TM anteriorly and the peripheral iris posteriorly. Aqueous leaves the anterior chamber through the TM. If the filtration angle is too small, movement of the iris into the angle during dilation can physically obstruct drainage and cause an attacek of ACG. o Location Junction of ciliary root of the iris and the sclera, 1.5 posterior to the limbus. Shape- “U” The angle can vary from 20-45 degrees. With dilation, the iris is stuffed into the angle and can block the trabecular meshwork. With angle closure, there is a lot of pain and a lot of pressure on the optic nerve. 40mmHg paralyzes the dilator. It is stuck. Estimation Slit lamp Shadow Test o This is done with a pen light. Aim light temporally at the corneal limbus and look nasally. o Look for bowing of the iris-lens diaphragm. o Do not dilate if there is a shadow more than 50% covering the eye. Gonioscopy- done to inspect narrow angles Trabecular Meshwork o Shape- Triangular Apex faces the cornea. Base against scleral spur and anterior surface of ciliary body. Spongelike o Components (internal to external) Uveal meshwork Most interior. Arises from the ciliary body (uveal tissue) and extends anteriorly and medially to the end of Descemet’s membrane. This is seen on the cornea as a white line called Schwalbe’s ring. End of descemet’s to ciliary body. o A smaller zone (thin slice) o Composed of small fibers and large openings. Perforated sheet (2-3 layers), forming a sieve. This has finer, more rounded strands and larger openings. The strands have a collagen core surrounded by endothelial cells. Pectinate ligaments (aka iris processes) o Connect iris and trabecular meshwork. o Observable with gonioscopy. Corneoscleral Meshwork- smaller holes and thicker fibers. More external. Connected posteriorly to the scleral spur. The corneoscleral meshwork runs anteriorly to merge with the corneal tissue in the region of the end of Descemet’s membrane. More like sheets with holes (trabecular sheets) Strands are more flattened, and the openings are smaller. Size- thickest component of trabecular meshwork. o Thickest at its posterior end near the scleral spur, where it measures 120-150 microns. Juxtaconicular Tissue, aka Endothelial Meshwork Thin (10-20 microns) Location- around Schlemm’s canal, covering it Solid sheet of connective tissue, thicker than the tissue surrounding the rest of the canal, with a distinctive cellular composition which includes endothelial cells. There are no pores. The aqueous enters the endothelial cells through small passages which form vacuoles. A membrane between Schlemm’s canal and corneoscleral meshwork. o Has endothelial cells that transports it across the membrane (pinocytic activity). Canal of Schlemm o A circular venous channel external to the TM. A collective channel. 36mm long which encircles the eye in the area of the limbus, just exterior to the TM. o Technically, Schlemm’s Canal is surrounded by sclera posteriorly and to the external side. Immediately posterior to it, and somewhat overlapping it internally is the scleral spur. In the circular course, it occasionally divides into two or more canals only to rejoin into one canal further on. o o o o o o On cross section, it is oval with the long axis parallel to the sheets of the TM. Structurally, the histology of the canal is cimple. It is surrounded by the juxtacanicular tissue and includes a endothelial basement membrane and an endothelial cell lining. Most of theendothelial cells are small with the exception of the cells on the side of the TM, which are 2-5x larger in diameter. The outstanding characteristic of these latter cells is the presence of giant vacuoles which are thought to be involved with transport of aqueous into the lumen of Schlemm’s canal. Location- external to trabecular meshwork in anterior chamber. Flattened tube parallel to eye surface. Scleral spur is posterior and interior Sclera is external Drains to venous system Purpose- drains 90% of aqueous Cross section Will divide and return as one sometimes Lined with endothelial cells Observation with gonioscopy Use a gonioscope- a lens with mirrors Cornea- the done End of descemet’s- glistening white line Schwalbe’s line Trabecular meshwork- a gray strip Scleral spur- thick white line Ciliary body- brownish strip Iris- floor Iris processes- line going up to trabecular meshwork Accessory Channels- gets aqueous into Schlemm’s Canal Internal channels- coming from the center Internal collector channels of Sondermann o Are either endothelium-lined canaliculi connecting the anterior chamber with Schlemm’s canal or folds of Schlemm’s canal that serve to increase the total surface area of the wall of Schlemm’s canal opposing the TM. External Actual canals Efferent collector channels o Unevenly distributed around the outer circumference of Schlemm’s canal. Most of them anastomose with each other to form the deep scleral plexus, and some course directly to the episcleral venous plexus. The latter are called aqueal veins, because they may be seen with the SLE under the conjunctiva as minute clear vessels containing aqueous. From the deep scleral plexus, the aqueous ultimately makes its way to the episcleral venous plexus to join venous blood. o 20-30 o Drain aqueous into blood vascular system (interscleral venous plexus and deep scleral plexus episcleral veins- seen on eye surface) Aqueal Veins of Asher Larger external channels From canal of Schlemm to episceral veins, by passing plexi. Uveoscleral Flow- remaining 10% of aqueous outflow o How a group of glaucoma medications work o Through iris and ciliary body to choroid then the vortex veins Aqueous Humor o Definition Transparent, colorless liquid in the anterior and posterior chambers of the eye. o Functions Nutrients for anterior chamber structures: lens and posterior cornea. Also provides oxygen. Amino acids, oxygen, glucose to the cornea, lens, iris, and ciliary body. Waste product removal IOP maintenance keeps anterior chamber inflated. Normal about 15-20 mmHg Balance due to production/ drainage Optical- a refracting medium due to index differences Maintains transparency o Production Not truly understood completely From plasma of blood From ANS? Decreases in sleep by 45% Ciliary body Extends from the (anterior) iris to the (posterior) ora serrata Principally unstraiated muscle o Longitudinal, radial, and circular Two divisions o Pars plicata- anterior third consisting of ciliary processes Highly convoluted to increased surface area Where the aqueous is produced o Pars plana- posterior 2/3 Flat Ciliary processes- approximately 70 ridges projecting inward from the pars plicata. o 0.5mm wide, 1mm high, 2mm long. 5-7mm total. o Injections go behind this to decreased bleeding Firmly attached at the scleral spur. o This is the most anterior of the ciliary body. Blood supplies consist of the anterior and long posterior ciliary arteries o They join at the major circle of the iris. Small arterioles from this. o Each ciliary process receives an arteriole and is drained by a venule which connects with the vortex system. o o Nervous supply- long posterior and short ciliary nerves, parasympathetic and sympathetic innervations, sympathetic being more important. Anatomy Stromal core surrounded by a layer of pigmented epithelium (cuboidal) and nonpigmented epithelium (columnar) Two layers of epithelium face apex to apex. o Bruch’s membrane forms the basement membrane for the pigmented layer. It continues into the retina. o Basement membrane for the nonpigmented layer is the internal limiting membrane. o All layers of the retina condense to this near the ora serrata. Many connections between the two layers (PE and NPE) o Desmosomes, gap junctions, tight junctions o Tight junctions- at apex of nonpigmented cells, for a tight barrier. o Tight junctions and blood vessels with small fenestrations result in a blood-aqueous barrier Clinical consequences Only small substances get out of blood vessels. Anything leaving bloodleaves though the NPE, therefore there is little light scatter. Blood aqueous barrier very important Some cannot cross this Depends on lipid solubility and size. Hard for drug companies and TPAs. Composition Initially compared concentration with that of plasma. Tells you transport mechanism with core gradients Substances in the aqueous are used by all the surrounding tissues and the aqueous contains all their waste products (cornea, lens, vitreous and iris) Osmolarity o Slightly hyperosmotic to plasma. Depends on where you sample. It is higher to the ciliary processes. In monkeys, there is no difference. Electrolytes o Na+ (150) and K+(4) concentrations similar to plasma. o CL- (124/107) higher and HCO3- (20/27) lower than plasma levels o Oxygen diffuses into aqueous from blood, so lower concentration in aqueous (53) o Glucose lower (2x) since it diffuses into the tissues o Lactate higher (3x) than plasma because the aqueous is the dumping ground. o Ascorbate- high concentration in aqueous (about 20x that of plasma) rises with increasing concentration in the blood until a ceiling of about 50 mg/100ml is reached in the aqueous Thus, secreted actively by a specific carrier mechanism that can be saturated. This is a freeradical scavenger that removes them, minimizing the effect of UV. Free radicals damage proteins and DNA. o Amino acids (7-3) Most amino acids in higher concentrations in the aqueous than theplasma which indicates active transport. so they are pumped in. they are needed in structures like the lens that have no blood supply. Different amino acids have different concentrations. o Proteins are limited in the aqueous by the blood aqueous barrier (1/90) Low molecular weight proteins can get into the aqueous (albumin in high concentration). This minimizes light scatter. o Immunoglobulins IgG concentration of 3mg/100ml of aqueous IgD, IgA, and IgM not normally found Only found in inflammation Small quantities of complement can be found. o Other compounds found include hyaluronic acid, corticosteroids, lipids, vitamin B12, and lens proteins. Clinical Significance May aid in diagnosis of ocular conditions o Increase in glucose can mean diabetes mellitus? o 140,000 Dahlstrom proteins seen in patients with POAG. Aqueous Dynamics Review o Aqueous Production Aqueous volume 0.25ml in anterior chamber 0.06ml in posterior chamber Aqueous production Production rate- 2.5ml/min. o Total displacement of aqueous in 100 minutes. Ciliary body o Produced in ciliary body by ciliary processes, specifically the ciliary epithelium. o Flows into the posterior chamber to the anterior chamber and vitreole chamber. The bulk of the fluid flows out the angle (trabecular outflow) of the anterior chamber. Aqueous is also exchanged with the retina (uveoscleral outflow), lens, ciliary body, iris and cornea. o There is a resistance to flow at the lens-iris interface, Pupillary Block- lens pushes iris out and blocks the TM o There is also a resistance to flow at the angle of the anterior chamber. Pressure in the eye increases until the force pushing fluid out of the eye (i.e., the eye pressure) results in the same amount of fluid leaving the eye as is produced and enters the eye. Methods of aqueous production o Active secretion Produces the bulk of the aqueous “Active”- requires energy expenditure Na/K ATPase located along lateral cellular interdigitations of NPE. aqueous production decreased when use ouabain, therefore 70% aqueous is produced vua active transport na+ transported out with CL-, HCO3-, and H2O following positive charge in aqueous near NPE wall. Solute concentration at region near the tight junction and decreases as you approach the posterior chamber. Two essential enzymes for active secretion Carbonic anhydrase o CAIs are clinically used to lower IOP Na K dependent ATPase o Quabain- little use for these. Side effects are too great. o Ultrafiltration A substance is forced across a membrane with the help of a hydrostatic driving force This equals the capillary pressure (BP) = 2730mmHg Produces a small amount of aqueous Hydrostatic pressure probably greater in opposite direction (out of eye). Capillary pressure in ciliary processes is 45 mmHg Very high, higher than IOP, which is opposite force. Columnar epithelium impermeable to protein- blood aqueous barrier. Ultrafiltration is IOP dependent Elevated IOP- reduced ultrafiltration Lower IOP- increased ultrafiltration Maintains IOP at about 15 mmHg o Diffusion o o o Movement of a substance down its concentration gradient Ions flow in/out pulling water with it Small amount of aqueous made this way Flow of Aqueous Posterior chamber to outflow pathways Ciliary body posterior chamber through lens-iris diaphragm anterior chamber trabecular outflow path or uveoscleral outflow pathway In anterior chamber In deep anterior chamber aqueous is hotter drifts upward approaches peripheral AC and cools drifts downward in more anterior AC. Particles in AC (pigment, etc) may deposit on inferior or middle corneal epithelium Aqueous outflow TM Major route- 65-80% of outflow TM outflow path o AC uveal TM corneoscleral TM justacanalicular tissue Schlemm’s cancal aqueous veins of Ascher epscleral venous plexus superior and inferior ophthalmic veins cavernous sinus jugular veins Each structure has the capacity to affect tonometry Common cause of elevated IOP o Most high IOP in OAG particularly COAG is caused by an obstruction in the TM outflow mechanism Episcleral venous pressure and IOP o 1 to 1 relationship between pressure change in episcleral veins and IOP change. o Increased episcleral venous pressure caused by Valsalva maneuver, gonioscopy (pressure on episcleral veins), carotid cavernous fistula, Sturge Weber syndrome Increased IOP increased TM outflow Uveoscleral Outflow 20-35% of total flow Uveoscleral pathway o Iris ciliary body suprachoroidal space choroidal (or episcleral) veins Not pressure dependent Ciliary muscle contraction caused increased trabecular outflow and decreased uveoscleral outflow. Function of Aqueous Responsible for producing IOP Maintains structural integrity of globe, maintains retina and choroid in place. Maintains optical elements in place. o Nourishes lens, endothelium of cornea, vitreous, TM Overview of actions of DPAs and glaucoma meds- relation to aqueous flow Anticholinergics (parasympatholytics) and adrenergic agonists (sympathomimetics) Anticholinergics used clinically o Tropicamide (Mydriacyl, Mydrifairm Spectrocyl, etc) Good mydriasis of short duration, weak cycloplegic o Cyclopentolate (Cyclogyl, Spectropentolate, etc) o Scopolamine o Homatropine o Atropine Strong mydriatic and cycloplegic effect Actions o Actos to block parasympathetic system causing Cycloplegia (ciuliary muscle blocked) Papillary dilation (papillary sphincter blocked) Potential effect of anticholinergic agents on IOP of patients with open angles o IOP may be increased in two ways Cyclplogic effect: Ciliary muscle relaxed longitudinal fibers relax no pull on scleral spur pore size through TM is decreased decreased aqueous outflow rate increased IOP Pigment release into anterior chamber Much more likely with phenylephrine o Can produce higher IOP in susceptible individuals with open angle. Common in COAG patients (<10%) o To detect this must check post-dilated IOPs. o Significance Significant IOP elevation in susceptible patients (elderly, vascular disease such as carotid occlusive disease, prior CRVO) can cause CRVO, BRVO which can in turn cause acute vision loss. Increased IOP can cause decreased blood flow to the eye. Indicates very fragile IOP balance the patient’s IOP may spike at other times while not dilated best to get diurnal IOP evaluation and carefully review all prior IOPs in your records. Indicates decreased homeostasis. This is a transient (wears off as cycloplegia wears off) increase in IOP but occassionaly IOP does not return to normal best to monitor the IOPs until they have returned to normal. o Post dilated IOPs should be measured Glaucoma patients Glaucoma patients on pilocarpine Cycloplegia reverses the ciliary spasm that pilo produces to decrease IOP. Narrow Angles Most narrow angles that close due to dilation (rare) close several hours after the dilation. Pigmentary Dispersion Syndrome/ P. Glaucoma A condition where the anterior chamber is so deep and the iris plane is concave so that the iris lays back against the ciliary zonules. The zonules rub the posteriuor pigment off and it is dispersed into the anterior chamber. It can cause glaucoma (pigmentary glaucoma). Phenylephrine can induce iris pigment release into the anterior chamber in normal patients and is much more likely to do so and to cause increased IOP in patients with pigment dispersion syndrome. Pseudoexfoliation Phenylephrine can induce iris pigment release into the anterior chamber. Glaucoma suspects DDx- post-dilated increased IOP Angle closure (narrow angle) Plateau iris Mydriatic cycloplegic effect Pigment in AC Angle closure glaucoma and papillary block o Sphincter relaxed papillary dilation mid-dilated position (maximum contact between posterior iris and anterior lens) relative pupil blocl IOP higher in posterior chamber iris bombe (iris bowed forward) angle closure rapid elevation of IOP. Usually occurs when patient is coming down from dilation. o This mechanism only occurs in patients with narrow (occludable) angles A grade 3 or 4 angle will not close. Cholinergics (parasympathomimetics) Pilocarpine- most commonly used Stimulates the ciliary muscle (ciliary spasm) pulls on scleral spur and trabecular meshwork increased aqueous outflow rate decreased IOP. Sympathomimetics Epinephrine, propine Increase aqueous outflow through TM by stimulating B2 sites in TM. Sympatholytics Beta blockers- timoptic, betoptic (cardioselective), Betagan, Optipranolol, Ocupress Reduce aqueous formation by blocking B2 sites in ciliary body. Carbonic Anhydrase Inhibitors Diamox, Neptazane Inhibit carbonic anhydrase decreased active secretion of aqueous decreased IOP. Anatomy of Filtration Angle and Related Physiology The trabecular meshwork is located in the internal scleral sulcus, extending from Schwalbe’s ring to the scleral spur, ciliary body band and iris root. Components of the Trabecular Meshwork o Uveal Trabeculum Adjacent to (and lines) the anterior chamber Consists of cords of collagen connective tissue covered by a single layer of endothelial cells extending from Schwalbe’s line to the iris root. Large openings between the cords cause little resistance to aqueous outflow normally. It is rare to have obstruction here. The endothelial cells have phagocytic capability. These endothelial cells are lost with age in this area, but they are lost to a greater degree in glaucoma. This is followed by an increased thickness and fusion of trabecular cords and sheets. o Corneo-Scleral Trabeculum Extends from Schwalbe’s ring to the scleral spur and ciliary body It consists of sheets of connective tissue covered by a single layer of endothelial cells, running circumferentially around the anterior chamber angle. Small holes (“trabecular pores”) become smaller in size with increasing distance from the anterior chamber (closer to Schlemm’s canal). This acts as a filtering system. Endothelial phagocytosis acts to “clean” the filter. However, phagocytosis can lead to detachment of endothelial cells, causing permanent loss. The scleral spur inserts on the posterior end of the trabecular meshwork. Increased force of ciliary muscle contraction causes increased traction on the scleral spur and trabecular meshwork, resulting in increased trabecular pore size (greater aqueous outflow). This may also affect the inner wall of Schlemm’s canal. o Intratrabecular Space Mucopolysaccharides (MPS) such as glycosaminoglycans (GAGs) are ground substance the fill the space between the trabecular sheets. MPS is secreted and degraded by the trabecular endothelium. More MPS means decreased aqueous outflow. Factors affecting MPS Steroids (steroid responders) Age Hypothyroidism o Juxtacanalicular Tissue o o This is the area of thetrabecular meshwork immediately adjacent to Schlemm’s canal. Endothelial cells here are different than those in the uveal and corneoscleral trabecular meshwork. It is the site of greatest resistance to aqueous outflow in the trabecular meshwork. Tendons from the longitudinal fibers of the ciliary muscle connect to elastic fiber network here and to the endothelial cells lining Schlemm’s canal. This forms the cribiform plexus which probably affects aqueous outflow. Aging increases resistance to aqueous movement, possibly due to increased intracellular material. One component of this age effect may be due to a progressive loss of ciliary muscle tone in presbyopia causing reduced ability to open the trabecular meshwork. Schlemm’s Canal These are lined by endothelium with tight junctions. Aqueous enters the canal by vacuolization process. Giant vacuoles within the endothelial cells of the inner wall of Schlemm’s canal transport aqueous through the endothelial wall. The vacuolization rate is pressure dependent, not energy dependent. The IOP must exceed the pressure in Schlemm’s canal. The higher the IOP, the larger the vacuoles. If pressure in Schlemm’s exceeds the IOP, backflow of aqueous and possibly blood from the episcleral venous plexus into the trabecular meshwork can cause elevated IOP. Aging and POAG reduce the vacuolization. Collection Channels, Episcleral Venous Plexus There are 30-35 collection channels that collect fluid and dump into aqueous veins or intrasceral venous plexus, which then feed into episcleral venous plexus. There is a 1 to 1 ratio of pressure change in episceral venous plexus pressure to IOP. If the episceral venous plexus pressure is increased, the IOP will increase the same amount. Normal episcleral venous pressure is 8-10 mmHg. Sturge Weber syndrome, carotid cavernous fistula, thyroid eye disease, enthusiastic gonioscopy with Haag-Streit-style goniolens all cause elevated episcleral venous plexus pressure and resultant equal elevation of IOP. Normal Aqueous Production and Flow Aqueous Production o Two Mechanisms Ultrafiltration About 20% of aqueous production Perfusion pressure in the ciliary process capillaries is the highest in the body, 45 mmHg. This pressure exceeds the opposing pressures (IOP and osmotic pressure). Serum is “pushed” by the high pressure in the capillaries (hydrostatic pressure) through walls of capillaries in ciliary processes. This is a pressure dependent mechanism. o If IOP goes up, ultrafiltration is reduced. This is a homeostatic mechanism to maintain IOP at a fairly constant level. o If perfusion through small capillaries in ciliary processes goes down, ultrafiltration is reduced. This contributes to the “pseudofacility of outflow” in tonography. If IOP is increased by the Schiotz tonometer, ultrafiltration is decreased and the trabecular outflow is increased. This decreases IOP. Ultrafiltration may be controlled clinically by controlling the capillary blood pressure. Systemic blood pressure can be related. o Uncontrolled systemic hypertension may be associated with increased ciliary process capillary pressure. Increased ultrafiltration then leads to increased IOP. o However, lowering the systemic blood pressure can cause both lowering of the IOP and lowering of the perfusion to the ONH, causing glaucomatous damage despite the low IOP. Active Secretion 75-80% of aqueous production, occurring in the nonpigmented ciliary epithelium. o This requires energy to actively transport ions of the ciliary processes, including sodium, bicarbonate and chloride. o The transport of ions creates an osmotic gradient toward the posterior chamber. The enzymes carbonic anhydrase (CA) and ATP-ase are required for this. Therefore, active secretion can be clinically controlled by controlling the action of enzymes with carbonic anhydrase inhibitors (CAIs). Flow of Aqueous: Posterior Chamber (PC) to Anterior Chamber (AC) o Aqueous is produced in the ciliary processes. It then flows from the PC though the lensiris diaphragm to the AC. There is no aqueous movement through the iris. It must move between the anterior lens and the posterior iris. o Convection currents in the AC warm the deep AC, causing the aqueous to rise. It is cooler in the anterior portion of the AC, and here it moves downward. This can cause deposition of pigment on the corneal endothelium in the mid to lower cornea (Krukenburg’s spindle). Outflow of Aqueous (General Concepts) o Virtually all elevated IOP/glaucoma is due to outflow obstruction. Hypersecretion is very rare. It occurs most often in middle aged females, associated with hypertension and myopia. Intermittent increased IOP due to increased aqueous production while outflow is normal. The trabecular meshwork is the major site of obstruction to aqueous outflow in POAG, specifically the juxtacanalicular tissue in the trabecular meshwork. o Paths of outflow Trabecular outflow This is 75-90% of the total outflow and depends on pressure (IOP). Aqueous flows from the anterior chamber to the trabecular meshwork, then to Schlemm’s canal and collection channels to aqueous veins and episcleral venous plexus. Affected by o IOP Increased IOP causes increased trabecular outflow. o Miotics Cause increased trabecular pore size, increasing trabecular meshwork outflow and decreased IOP. Also causes decreased uveoscleral outflow. o Adrenergic agonists Beta sites in the trabecular meshwork appear to cause increased aqueous outflow when stimulated. o Cycloplegics May cause reduced trabecular pore size in some patients with POAG, especially those who are on miotics to control their IOP. Post DFE Increased IOP Mechanisms Cyclo effect- decreased TM outflow/ relaxes ciliary body. This is the most common. Pigment release into the AC Pupil block, angle closure, plateau iris Uveoscleral Outflow This is 10-25% of aqueous outflow and is non-pressure dependent. o This is not pressure dependent at IOPs >7-10 mmHg. It is through the iris stroma or face of the ciliary body band through the ciliary muscle to suprachoroidal space to the vortex veins to ophthalmic veins. o The ciliary muscle is the hardest. Does not depend on the pressure within the episcleral venous plexus, unlike trabecular meshwork outflow. Outflow depends greatly on the tone of the ciliary muscle. Contraction (ciliary spasm) causes lowered outflow, relaxation (cycloplegia) causes slightly greater outflow. This is decreased with pilocarpine and increased with cycloplegics and certain prostaglandins, although pilocarpine can block the effect of prostaglandins due to ciliary spasm. Both trabecular and uveoscleral outflows are decreased in POAG. Intraocular Pressure Definition o The tissue pressure of the ocular contents. It is the equilibrium between aqueous production and drainage. o About 15mmHg, but does fluctuate (15.5 +/-2.57) o Normal range of pressures 10.5 – 20.5 2 standard deviations, 95% of the population Factors affecting the IOP o Long term Genetics Relatives of individuals with POAG are more likely to have high IOP, especially the mom. Age IOP increases with age Age <40 >40 >70 Sex o % with Glaucoma 0.7 2 4-5 Race IOPs equal in the age range of 20-40, after menpause women have higher IOPs. This could be an argument of endocrine control? African-Americans have a higher incidence of POAG than Caucasians. Asians have more closed angle glaucoma than Caucasians, but less POAG. Short term Diurnal Variation 3-6mmHg change in a 24hr period. Because of the broad variability, you need to see those with glaucoma at the same time Change probably related to aqueous production and not drainage. Lowest at about 2-3am. o Production decreases 45% when sleeping. Highest at about 7-8am. >10mmHg is pathogenic. Sitting Going from sitting to a lying position results in an increase in IOP which is even greater in glaucoma patients. This is due to the increase in the arterial pressure. Normal- 2mmHg increase Glaucoma patients is 3 or more. Total body inversion Causes an increase in IOP by as much as 15mmHg. Blinking Raises IOP briefly, by pushing the globe back. Exercise Decreases IOP short term Blepharospasm Increases IOP Coughing Increases IOP Blood pressure Some people believe there is a link between blood pressure and IOP, but there is no clear evidence. This is probably short, not long-term. General Anesthesia Decreases IOP Decreases blood pressure and muscles are relaxed Alcohol Decreases IOP Pulls fluid out of the eye Cannabis Decreases IOP Tobacco Decreases IOP Tonometry and Glaucoma Rationale for Tonometry o Tonometry is performed primarily to assess risk, help detect, help diagnose and assis in management of glaucoma. Tonometry indications o All patients who can tolerate tonometry o Note: if a patient cannot have tonometry this fact and the reason should be recorded in the patient’s file. Glaucoma defined o Group of diseases where progressive damage occurs to the retinal ganglion cell axons and is clinically evident in the optic nerve and the retinal nerve fiber layer (RNFL). This damage may in part be due to IO which is too high at some time for the health of the ganglion cell axons. Eventually the ONH/ RNFL damage is accompanied by characteristic progressive visual field loss and other visual function loss. Clinical evidence of glaucoma o Damage to optic nerve, RNFL structure (structural damage) Increased cup size vertically or overall RNFL loss o Damage to the function of the eye (functional damage) Visual field loss- most commonly used index of functional damage Pattern electroretinogram (PERG) Pattern VER (PVER) Flash VER Contrast sensitivity Color vision Other IOP and Glaucomatous Damage o The ON damage in glaucoma is the direct result of retinal nerve fiber death (ganglion cell axons) o The exact cause of the RNFL damage and optic nerve damage is not known, but can be the result of an IOP which is too high for normal functioning of the ganglion cell axon in some cases. o Significant individual variation exists in ability of an ON to withstand various levels of IOP. Types of Glaucoma o Importance of glaucoma in any discussion of IOP. o OAG There is no clinically evident obstruction of aqueous outflow; there is no obstruction of the flow of aqueous to the TM. The angles are opwn and there is no pupil block. Glaucoma characterized by ONH or RNFL or VF damage. There may be elevated IOP (>21) at some time. There may never be IOP >21mmHg (low tension glaucoma) o ACG A clinically evident block of aqueous outflow is present at the angle the angle is “closed” the peripheral iris (iris root) covers the TM. Aqueous cannot get to the TM. Definitive diagnosis is by gonioscopy. The high IOP usually >40mmHg can quickly produce glaucomatous change. o Two groups which cause great problems in glaucoma diagnosis Low tension glaucoma/ normal tension glaucoma A form of OAG characterized by glaucomatous damage, but IOP is never >21mmHg. Numerous IOP measurements are necessary to ensure IOP never exceeds 21mmHg. Ocular hypertension A condition where there is no clinically evident structural or functional damage consistent with glaucoma though the IOP is >21mmHg. Common in the US At risk for glaucoma Document over time. Normal vs. Abnormal IOP o “Clinically normal IOP” Clinical examination reveals no functional or structural dysfunction consistent with glaucoma Clinical exam includes stereoscopic ONH evaluation, RNFL evaluation, VF evaluation, etc. A very critical examination is necessary in order to detect subtle glaucomatous damage. Needs to detect change with time. o “Statistical normal” IOP in a given case is within the range of most non-glaucomatous IOPs regardless of whether glaucomatous structural or functional damage is present. Note: patients who have LTG have statistically normal IOPs at all times. Statistical studies of IOP are helpful in assessing the risk of the development of glaucomatous damage- very important in decision making process. For an example if the IOP is statistically very high such as 40mmHg the patient should be treated to lower IOP even with normal structural and function since the future risk of glaucomatous damage is great. Tonometry and Glaucoma Detection o Tonometry used alone to detect glaucoma, using 21mmHg as standard Sensitivity 50% Ability to identify glaucoma patient as glaucoma patients Using tonometry only thouse with IOP 21 are considered glaucomatous. Big problem: 50% of glaucoma patients have IOP <21 on any single IOP check. Several studies have shown this. Specificity 70-90% Ability to identify normal patients as normal. Tonometry has fair specificity due to many patients with IOP >21 who do not have glaucoma ocular hypertensives. Percent of population who have ocular hypertension increase with age in older patients tonometry is even less specific. Up to 30% of normal patients have IOP >21mmHg. Tonometry used alone to detect glaucoma screening has poor sensitivity and fair specificity IOP Cutoff >17mmHg >19mmHg >21mmHg >24mmHg >26mmHg Sensitivity 80.1% 64.9% 47.1% 27.2% 20.4% Specificity 51.8% 72.9% 92.4% 96.4% 98.1% Tonometry alone in glaucoma screening Too many “false positives” (IOP >21 but no glaucomatous damageocular hypertensives) over referral (fair specificity) Too many “false negatives” (IOP <21 but glaucoma present- 50% of all COAG (including all LTG have IOP <21mmHg on a single IOP check)- poor sensitivity Patient Education regarding Tonometry o o o Tonometry is performed in a comprehensive exam for one reason- to help detect glaucoma/ to evaluate the risk of glaucoma. Most patients think that with tonometry alone glaucoma can be diagnosed or ruled out. With sensitivity of 50% and specificity of 70-90% certainly this is not true. Therefore patient education must address the misconception and emphasize that several tests (IOP, VF, ONH/RNFL evaluation, case history) are used for glaucoma detection and diagnosis. Thus a comprehensive exam is far better than an IOP check alone. Sample script “With this test we will measure the fluid pressure inside of your eyes. This is a test that is helpful in the detection of glaucoma. Actually we do several tests for glaucoma in our comprehensive exam. All of these tests together must be used to accurately find glaucoma and/or ensure that you do not have glaucoma.” For Goldmann tonometry after ensuring no hypersensitivity to anesthetics “I am going to place a drop on each eye. It is an anesthetic. You can blot your eyes, but please do not rub them for the next half hour.” After instilling the Fluress and having the patient hold the eyes closed for one minute “Please blink a couple of times, then place your chin in the chinrest and your head against the headrest. Keep your head firmly against the headrest at all times.” IOP Interpretation Statistics and Studies o Leydhecker’s Study 10,000 “normal” patients 10-69yo. Schiotz tonometry used. Flaws in methodology/ analysis of data Schiotz tonometry used Not Gaussian distribution (but he used statistical evaluation based upon Gaussian distribution) Made incorrect assumption about pressures around low twenties (a second peak in his data). o Exclused as glaucoma Leydhecker assumed that those with IOPs >21mmHg actually had glaucoma and he threw these patients out assuming that they were not normal. They were not included. He did not make this decision based on presence of damage, only IOP >21. Many normal patients (ocular hypertension) have IOP >21. Findings of Leydhecker’s study Population IOP mean 15.5mmHg Standard deviation 2.5mmHg o 2 standard deviations- 21 mmHg Distribution was not a standard Gaussian (bell-shaped) distribution. There was a skew toward higher IOPs. However, he excluded those with IOPs >21 mmHg. This made the distribution Gaussian. Leydhecker’s interpretation was based upon a standard (Gaussian or bellshaped) IOP distribution because he deleted patients with IOP >21. Based on Gaussuan statistics, 2 standard deviations = 20.5 mmHg, 97.5% of “normal” IOPs would be <21 mmHg Commonly quoted statistics on “normal” IOP o Mean normal IOP 15.5 mmHg. Other studies 15-17 mean, with a standard deviation of 2.5 – 3.5. o Upper limit of normal in Gaussian distribution: 21 mmHg o In a skewed distribution 24 mmHg o Clinical decision: normal vs. abnormal IOP The judgement of normal from abnormal IOP is a clinical decision based on Knowledge of the statistical limits of normality Signs (structural or functional)- suggestive of glaucoma- instrumentation (tonometry) greatly influences the screening. Risk factors for development of glaucoma damage o IOP is the strongest risk factor for predicting future glaucomatous damage. Other important factors in interpretation of IOP in glaucoma evaluation Highest level of IOP (spike height) Long-term trend in IOP Diurnal variation Interocular assymmetry Factors affecting IOP- long-term factors o Age Slightly upward shift in IOP with age in the US, about 1mm every 10 years. Great increase in ocular hypertension with age Most COAG in >40 age group o Race o Sex o Family history o Refractive error Factors causing transient IOP change o Diurnal variation Classic: higher around 7:00am, lower around 7:00pm. 60-75% population lowest in pm. 1985 study (recent paper by Smith at Baylor) two peaks, 7:00am and 12:00pm in both normals and glaucoma patients. It is larger for glaucoma patients. These are generally two times when we are not checking IOPs. We are waking up or at lunch. Note: the peak IOP time varies greatly from patient to patient. To determine the peak IOP it is necessary to obtain several IOPs at various times of the day. Guidelines for interpretation <5 mmHg normal (average in normals is 4 mmHg) 5-10 abnormally high >10 abnormal- highly likely to be glaucoma Cause: diurnal variation in plasma cortisol levels probably Increased variation seen in hospitals with corticosteroid administration. Decreased aqueous outflow to the TM. o o o o o o o o The peak IOP rather than the variation (peak to trough) is somewhat more important in predicting future development of glaucoma. The IOP can vary from minute to minute, hour to hour due to numerous factorsthe diurnal variation is very often not consistent day to day. Serial tonometry- measurement of IOP more than one in a day- CPT 92100 Accommodation Produces decreased IOP in a very short (seconds to minutes) period of time. Do not use an accommodative fixation target during tonometry, i.e., slit lamp fixation target, point on the slit lamp, ear, finger. Posture Sitting to supine- elevated IOP 2-3mmHg in normals. Greater elevation in glaucoma. Related to increased intrathoracic pressure- increased episcleral venous pressure. Inversion- >15mmHg increase in some patients. Exercise Prolonged exercise- decerased IOP by <30% Strain (Valsalve movement)- increased intrathoracic pressure decreased venous return from head higher episcleral venous pressure higher IOP. Each 1mmHg increase in episcleral venous pressure causes 1mmHg increase in IOP. Apprehension, lid squeezing, cocontraction of EOMs Apprehension Can poduce dramatically elevated IOP due to lid squeezing and cocontraction of EOMs. Lid widening Lid widening can produce slight increase in IOP. Holding breath can increase intrathoracic pressure decreases venous flow from head, increasing the IOP. Note: a tight collar may also decreased venous flow from the head, increasing the IOP. Patient should not hold his/her breath during tonometry. External pressure on the globe through the lids Often occurs when holding the lids during tonometry. Can cause small 2-3mmHg increase or large (>10mmHg) increase If enough pressure on the globe can cause a very large, >30mmHg, increase. Do not let the patient hold their lids during tonometry Fluid intake Alcohol- reduced IOP due to osmotic effect Water- may increase IOP Plarmaceutical agents Lower IOP- marijuana, heroin, beta blockers Elevated IOP- steroids (in steroid responders, topical > systemic) Cardiac cycle Cyclic variation of IOP of 1-5mmHg caused by cardiac cycle. In most people 1 or 2mmHg Systole- causes increased intraocular blood volume slight increased IOP CRVP (central vein pressure exceeded by IOP causing vein collapse) Diastole- lower intraocular blood volume slight reduction in IOP central vein pulses outward (central retinal venous pressure exceeds IOP) The cardiac cycle can be visualized with Goldmann tonometry. The mid point (average) of the cardiac cycle can be found with Goldmann tonometry- one reason for the great accuracy of Goldmann tonometry. With Goldmann, the mires go in and out, so take the average. If the mires are getting larger and smaller, this means the cornea is not applanated. NCT only takes a snapshot. o Trauma, inflammation Trauma usually produces an inflammatory response- traumatic iritis. Initially with trauma the IOP will usually decrease due to reduced ciliary body function reduced aqueous formation. Hours after the initial trauma the inflammatory debris (white cell, fibrin, red cells, etc) can block the trabecular meshwork causing an increased IOP. This is usually temporary. Many years later if the longitudinal fibers of the ciliary muscle disinsert from the scleral spur (angle recession), IOP may increase. A retinal tear leads to decreased IOP, because aqueous goes through the break. o Blood pressure Controversial correlation but possible increased IOP with increased blood pressure. Symptoms of high IOP o Chronic elevated IOP Most patients with glaucoma particularly COAG no symptoms at all. This is why tonometry is so important. Symptoms in COAG are rare. There is no pain, no redness, no blurred vision, no awareness of VF loss. Gradual onset. Symptoms occur based on Acuteness of IOP elevation (within 2 hours) o The faster the IOP rise, the more likely that symptoms occur. o Level of IOP (most IOP <35 have no symptoms) the higher the IOP the greater the likelihood of symptoms. o Acute elevated IOP ACG (because of rapid onset of higher IOP and level of IOP, 40-70mmHg) causes numerous symptoms. Angle closure is not the only cause of acute increased IOP. Acute increased can occur in open angle glaucoma, pigmentary glaucoma, and numerous other conditions. Gonioscopy is absolutely necessary to differentiate the cause. With decerased endothelial finction, stroma edema occurs with increased IOP. Symptoms which may occur in ACG Eye pain/ head pain Nausea/ vomiting Blurred/ floggy vision/ haloes Red eye Watery eye Photophobia Homeostatic mechanisms for increased IOP Increased TM outflow Decreased ultrafiltration Tonometry Manometry o First and most accurate method of measuring IOP. Directly measures IOP by cannulating the anterior chamber. This can not be done on humans. o Not a form of tonometry, not clinically useful. Definition of tonometry o Clinical evaluation of IOP by applying a force to the globe and relating that force to the deformation of the globe. Types of tonometry o All tonometry is based on the application of force to the globe with a deformation can be divided into two types based on the shape of deformation Indentation tonometry This is the older of the two methods to measure IOP in humans. Involves measuring the indentation of the cornea (or sclera) resulting from a given weight. Due to great variation in ocular rigidity (corneal or scleral rigidity) shape of indentation is variable and unpredictable, especially with the sclera. Displaces a large volume of intraocular fluid (aqueous)- then a conversion table is needed since the Pt is not equal to the Po. o Pt = IOP during tonometry o Po = IOP without the force of a tonometer on the globe. o Tonometers can actually raise the IOP. o Shoves aqueous into the TM. Schiotz tonometer is the prototype indentation tonometer. Applanation tonometry Flattens a small portion of the cornea. Shape is consistent, thus IOP can be mathematically determined. Intraocular fluid volume displacement is not as high as in indentation tonometry and ocular rigidity does not have as great an effect on IOP measurements. Therefore it is more accurate. Types of applanation tonometry o Constant area of applanation, variable force Instruments: Goldmann tonometer, McKay Marg, Perkins (handheld Goldmann), Tonopen Measures the force needed to flatten a constant area. o Constant force, variable area of applanation Instruments: Maklakov, Tonomat Measures area applanated by constant force These also tend to have high intraocular volume displacement thus conversion is needed from Pt to Po. Accuracy: Anytime high aqueous displacement occurs, lower accuracy of tonometer results. Less predictable. o Non-contact tonometry, “air puff” tonometer AO NCT, Xpert NCT, Keeler Pulsair, Topcon, Kowa Measures time to applanate cornea in response to a given force (puff of air), constant area. Basic concepts in tonometry o Pt = Po + ΔP Definitions Po = IOP in eye without force of tonometer applied to the globe (the true IOP). Pt = IOP with force of tonometer applied. ΔP = change in IOP caused by tonometer force; higher intraocular volume displaced higher ΔP. Accuracy The most accurate instruments are those where Pt = Po (ΔP = 0) they do not significantly change intraocular flui volume and are minimally affected by corneal rigidity. In indentation tonometry, ΔP is very significant (also true but to a lesser degree in applanation with variable area- Maklakov, Tonomat) o This goes down with time when the aqueous moves to the TM. o log Pt – log Po = EV log Pt1 – log Pt2 = e (Vc2 – Vc1) Pt = tonometric pressure Pt1, Pt2 = tonometric pressures with different plunger loads Po = IOP before tonometry This is what is want to be known. E = coefficient of ocular rigidity Vc1, Vc2 = volume of corneal indentation (displacement) corresponding to Pt1 and Pt2. o Imbert-Fick Law W=PxA The external force (W) against a sphere is equal to the pressure in the sphere (P) times the area (A) flattened by the force. Assumptions made by the Imbert-Fick Law Assumes the sphere (cornea) to be infinitely thin, dry, perfectly flexible, and a perfect sphere. Obviously that these are not true of the cornea. Problems with the applanation of the Imbert-Fick Law to tonometry Lack of flexibility results in a force corneal bending force or corneal rigidity (B). The cornea is not perfectly flexible. Cornea is not dry. Tear film results in an attraction for dry surface approaching the cornea surface tension (S). o Modified Imbert-Fick Law for tonometry W + S = Pt x A + B W = external force against globe S = surface tension of tear film Pt = IOP under force of tonometer A = area applanated o o B = cornea rigidity Pt = (W + S – B) / A Basis of the accuracy of Goldmann tonometry Goldmann found that when A = 7.35mm2, (3.06 mm diameter circular area applanated), S ≈ B and W ≈ Pt. The volume displacement produced by this area of applanantion is only ½ mm3, so Pt = Po. Thus, the effects of ocular rigiditry and surface tension are minimized. (ΔP is only about 3%, thus, Pt ≈ Po). Usually doesn’t work since change in corneal thickness from patient to patient. Note: the effect of ocular rigidity is not eliminated. It is, however, roughly offset by the opposite force of surface tension of tears at normal and near normal ocular rigidity. When the corneal thickness is 520 microns and the cornea is not edematous. Also when area applanated is 3.06mm diameter and each gram of force is 10mmHg (IOP). Factors affecting the accuracy of Goldmann tonometry Central corneal thickness Corneal curvature Corneal rigidity Tonometers- Instruments Indentation tonometers o Schiotz Prototype of indentation tonometers; also the accepted clinical standard in tonometry up to the mid 1960s. A plunger of known weight pushes on the cornea, thus result depends on ocular rigidity. Decreased rigidity means increased IOP. Description of instrument Indentation surface moving freely through a sleeve. Footplate- part that rests on the cornea. “Load” (weight on cornea) o Plunger + weights = “load” on cornea, loads 5.5, 7.5, 10 or 15 grams (these are plunger + weights) Scale reading o A relative scale of corneal indentation o The higher the scale reading the lower the actual IOP. Each 0.05mm of indentation causes an increased scale reading of 1. Scale reading is NOT in mmHg. It is an index of the amount of indentation higher scale readings = lower IOP. Friedenwald Tables In Schiotz tonometry, Pt is very different from Po because of a large volume displacement of aqueous and the effect of ocular rigidity. Conversion to Po is needed 1948 and 1955 Friedenwald tables (Friedenwald nomograms). Friedenwald developed this concept of ocular rigidity. Effect of ocular rigidity o Friedenwald nomograms o o o o o Tables based on Friedenwald nomogram- formula which corrects for ocular rigidity to get Po. However, the Friedenwald nomograms assume normal ocular rigidity. Average Ocular Rigidity 0.0215 This is the slope of the line joining the plots of two nomogram readings. Coefficient of ocular rigidity The factor in the formula (nomogram) for ocular rigidity is K (coefficient of ocular ridigity). Errors in ocular rigidity Most problems result from great individual variation in ocular rigidity (actual K is not what is assumed in Friedenwald’s tables) Ocular rigidity- IOP correlation If patient has high ocular rigidity, Schiotz reads false high. If patient has low ocular rigidity, Schiotz reads false low. Ocular rigidities are much more often lower than Friedenwald’s calculated than higher but there is much variation, causing substantially reduced accuracy of Schiotz on individual patients. Biggest source of error in indentation tonometry is ocular rigidity. Causes of error in indentation tonometry Variances in ocular rigidity Intraocular fluid (aqueous) volume alteration aqueous is “pushed out” through TM in indentation. This causes progressive lowering of IOP on repeated Schiotz readings. Corneal thickness or steeper K higher volume displacement higher ΔP (false high). Low/high ocular rigidity correlations Low ocular rigidity (false lows with Schiotz) Higher IOP Keratoconus Retinal detachment surgery Cataracts surgery o Do not use Schiotz tonometry after cataract surgery, RD surgery, RK- any surgery requiring incision into the sclera or cornea. Miotics (for glaucoma theapy) RK LASIK, PRK Myopia? o o o o o Applanation Tonometers o Goldmann Tonometry High ocular rigidity (false high readings) Hyperopes Thicker than normal corneas. Advantages of Schiotz Light and portable (small) Cheap to buy and maintain Does not require electricity Always get a reading Not particularly technique-dependent Disadvantages of Schiotz May be very inaccurate on individual patients. It is dependent on ocular rigidity and instrument scale markings are not detailed. They are easily misread. Possible spread of ocular disease Must be reclined or head parallel to floor Must use anesthetic Should not be used after intraocular surgery requiring incision into cornea or sclera Assumes an epithelium of 0.05mm. Technique can produce abrasions. Good patient cooperation necessary Rarely delegated to other office personnel Due to large aqueous displacement, Schiotz should not be performed repeatedly Must manually clean the tonometer after each use Recording Sciotz measurements 8/5.5gm 10.2mmHg (1955) T Schiotz 6/5.5gm 14.6mmHg 10:30am Reading should include Scale reading Load (marked on weight) IOP in mmHg from Friedenwald tables Data of table (either 1955 or 1948) Time of day Accuracy Not good correlation to Goldmann on individuals with abnormal corneal rigidity Population average is nearly equal to that obtained by Goldmann. Clinical use Not recommended as the primary tonometer but is useful as a backup tonometer. The most accurate clinical tonometer- all others are compared to Goldmann applanation tonometer. Readings within 1-2mmHg of actual IOP. Requires the use of anesthetic and fluorescein, therefore before DPAs were available to ODs, many ODs could not use Goldmann. Tonometers not requiring DPAs (Mackay-Marg, AO NCT) were used. Applanation area Always applanates an area of cornea surface 7.35mm2 (internal surface) or 3.06mm diameter (external) circular area. This is small. When this area is applanated, S = B, and W = Pt. Also Po = Pt and 1g of applanating force = 10mmHg IOP. This holds true for most patients, but not for all patients. Theory The cornea is covered with a tear layer which exerts a surface tension (force in towards the cornea). A probe applied to the cornea is acted against (a force pushing out from the cornea) by the corneal thickness and elasticity (the bending force). If the area if the probe is of the proper size, then the force from the surface tension will cancel the bending force. This leaves o Pressure = Force / Area The area of the probe has a diameter of 3.06mm. Description of instrument Plastic applanator (probe) applied to corneal surface. View through the probe from behind. Biprism splits image of applanated area which is viewed by the use of fluorescein which pools at the edge of the applanated corneal surface. Scale o Set up so that 1g of force (W) = 10mmHg of IOP. o On measuring drum, a reading of 1 = 1g of applanating force = 10mmHg of IOP, a reading of 2 = 20 mmHg, 3 = 30mmHg, etc. Each small slash on measuring drum = 2mmHg (0.2g of applanating force) Technique review o Clean probe Thoroughly wipe the probe, then dry it. Possible solutions o Cloroz 1:10- do not soak in bleach. It bleaches the external markings off the probe. o 3% hydrogen peroxide- best choice for soaking, 10 minutes o Isopropyl alcohol- can wipe probe, but should not soak probe. It loosens the biprism. o 70% Ethanol- same as isopropyl alcohol o o o o o o o o o All require a 10 minute soak to inactivate the AIDS virus. In all cases, insure that the probe is dry before performing tonometry. Clean after each tonometry (and when the room is set up each day) and allow time for air drying. Room lights down or off Adjust slit lamp Cobalt blue (not red free) filter; brighter illumination Place joystick in middle of range of motion and pull slit lamp back to allow maximal forward motion Mag 10x (or 7.5x(- low magnification Click tonometer into place. Most GATs are set up to be viewed by examiner’s left ocular only. Right ocular is often useless. Probe adjustment/ measuring drum adjustment Make sure probe directly forward and clicked into position. Set measuring dial on 10mmHg (1 on the dial) Drops Must use anesthetic; must use flourescein Options Fluress or Fluorox- benoxinate and fluorescein combined Fluorocaine- fluorescein-proparacaine combination Can give a drop of anesthetic then use fluoresceon strip Tetracaine, 1 drop plus fluorescein, proparacaine 1 drop plus fluorescein Instructions to patient Place chin in chin rest and head firmly against headrest at all times. Look straight ahead (do not indicate a close target) at wall, chair, etc. Blink a couple of times please (to spead Fluress) then hold your eyes open and try not to blink. Manually move probe to ½ cm from cornea, viewing side of slit lamp then allow patient to blink Move head to the back of slit lamp with right eye to left ocular view through tonometer while left eye watches patient’s head and eye. Function of examiner’s left eye: Watch head and eye to assure patient does not move. Watch for first corneal touch bluish limbal glow. Right hand joysticl, left hand on tonometer dial Move joystick forward until first corneal touch Left eye sees limbal blue glow (but very faint) Right eye sees very small green circle or semicircles which move erratically- move the joystick forward to get larger mires and to eliminate the erratic movement. o Move forward with joystick until semicircles enlarge to normal size and erratic pulsation ceases (should see a rhythmic pulsation of mores due to the cardiac cycle) o Center the green semicircles so that they are both ½ circle (both are the same size, a ½ circle). Move toward (up or down) the larger semicircle Both are within the circular field. Neither top nor bottom semicircle is cut off by the edge of the field move joystick toward (left or right) the green semicircle that is cut off. They match when 3.06mm of the cornea has been applanated. o Take measurement Adjust the inner edges of circles just touch- try to average the ocular pulse (1-4mmHg generally) so that the endpoint of the reading is the midpoint of the excursion of the semicircles. o Clean probe after use and allow to dry o If patient apprehension is apparent on the first eye (OD), then re-measure it after OS. This is because apprehension can increase the IOP. Will often see IOPs where the first eye (OD) is higher than he second. Other technique issues o Holding lids Do not allow the patient to manually hold his/her lids (too much chance of pressing on the globe which can greatly increase IOP). Do not touch the globe while holding lids. Very substantial IOP increase can occur. If you hold the lids and suspect that you have touched the globe, release the lids while the probe is still on the cornea. If the semicircles separate to indicate a lower pressure, this indicates that you did falsely raise the IOP. o Astigmatism Rarely causes inaccurate readings Adjust probe (rotate around long axis) to match minus cyl axis to red line on probe holder if corneal cyl of >6D Normally the 180 or 0 should align with the 0. Recording GAT o GAT 15/21 2:30pm or GAT 21/32 (dilated) 3:30pm Always indicate right eye over left eye, time of day and indicate if dilated reading. o Note: by convention right eye/ left eye No need to label the eye. No need to write the units (mmHg) o Must include GAT to indicate Goldmann applanation tonometry Right eye/ left eye reading; no need to write the units (mmHg) Time of day Dilated (if so, write “dilated”) Time of the most recent administration of each glaucoma medication Example o GAT 18/22 2:15pm Last T1/2 1gt OD at 8:30pm Accuracy of Goldmann tonometer o Manufacturer + 1mmHg o Actually +2mmHg of true IOP o +3% on cannulated eyes Sources of error in GAT o Mires too fat/thick false high Causes Too much Fluress or fluorescein Tearing Drop of Fluress or fluorescein left on probe Patient lid against the probe o Mires too thin false low Causes Dry eye Waited too long after instillation of Fluress Fluress or fluorescein not adequately spread patient should blink o Mires not equal in size false high Causes Probe too high or too low on cornea adjust slit lamp up or down to ensure that both green semi circles are ½ circles and equal in size. o Patient apprehension false high o Patient fixating at near false low Do not use any part of the slit lamp as the fixation point (also, not your ear) Direct the patient’s fixation to a distant target. Situations where Goldmann is not accurate o GAT is not optimally accurate for scarred or edematous cornea use McKay-Marg, Tonopen, or pneumotonometer Examples: refractive surfery (LASIK, PRK, RK), corneal transplant, corneal trauma These have a softer cornea, and provide false lows. o No tonometer is very accurate for thick (false high IOP) or thin (false low IOPs) corneas LASIK and PRK are very common causes of false low IOPs McKay-Marg, Tonopen or pneumotonometer are best for these situations o Decreased rigidity gives a decreased pressure reading. Decreased thickness means decreased rigidity Advantages of Goldmann tonometry o Standard of accuracy in clinical practice. o Relatively inexpensive, $800-1200, compared to more recently developed instruments, i.e., McKay-Marg, NCT, Tonopen, pneumotonometer o Little aqueous displacement- can be repeated without substantial effect of subsequent IOP measurements o Easy to perform o Easy to check calibration; rarely out of calibration o Very reliable, rare mechanical problems o Perkin’s tonometer (handheld Goldmann) is very portable and can be used for sitting or supine patient. Disadvantages of Goldmann tonometry o Touches cornea (unlike NCTs)- potential for spread of disease EKC has been found to be spread by Goldmann Can result in an abrasion Must sterilize instrument after each use. o Anesthetic needed, as well as a dye. o Unreliable, inaccurate readings on postsurgical scarred or edematous corneas o Not self-recording, i.e., no printout o Not portable. o Cant have a technician do it. You must do it. McKay-Marg Development Developed by OD and engineer during the 1960s. designed for use without anesthetic for ODs. However, consistently reads false high without anesthetic. Accuracy/ design Theoretically very accurate; best for abnormal corneal rigidity edema, scarring, irregular cornea bacuse force of corneal rigidity (B) and surface tenstion (S) are minimized due to instrument design. Very small measuring probe which is 1 ½ mm in diameter. But applanates a larger area, a 3mm diameter. o Corneal bending force (corneal rigidity) has its greatest effect at the edge of the applanated cornea which on the McKay-Marg is outside of the measuring probe. This virtually negates corneal rigidity, B. Waveform analysis/reading the MacKay-Marg. The very small area of the measuring probe (1/2 mm in diameter) minimizes surface tension of tears. Waveform of IOP is generated and printed as a second by second measure of IOP during corneal applanation. To obtain a good waveform, very good applanation technique is necessary- very technique dependent. o Force of corneal rigidity is against the sleeve which does not measure pressure (corneal bending force is almost eliminated). Accuracy o Tends to read slightly higher than Goldmann- even higher if no anesthetic o Very technique dependent; however most keep probe oriented perpendicular to corneal apex, requires practice. Can be used as the primary tonometer in the office if you practice the technique. o False high with patient apprehension. Remember there is no anesthesia Advantages Most accurate for scarred, irregular, edematous, thin/thick corneas o Due to minimal corneal rigidity and surface tension Use of rubber disposable tip required Can use in supine or sitting position Tonopen is very small and portable. Disadvantages Very technique dependent Should use anesthetic for best accuracy Price $2,000-4,000, relatively expensive compared to Goldmann. Tonopen Tonopen is basically a “computerized MacKay-Marg” Basic design is extremely similar to MacKay-Marg Reading the tonopen o Generates a waveform as the MacKay-Marg does o The waveform is not displayed or printed o Waveform is digitalized and analyzed by internal, on board computer o Computer rejects waveforms that are not the optimal (very technique dependent as was the original MacKay-Marg though much faster) and accepts only “optimal” waveforms. o When four waveforms have been accepted and stored, the instrument displays the mean IOP of the four readings on a digital display and displays the range, i.e. 5%, 10%, 15%, or 20% of variance between readings Advantages of the tonopen over MacKay-Marg o Very compact and portable; useful for nursing homes, hospitals, home visits, etc. o Quicker, no need to inspect a printed waveform. Disadvantages of the tonopen o Good accuracy with good technique o Cost $2,000-3,000 o Requires disposable tonotips for each patient o Calibration easier Accuracy o Tends to read false lows on higher IOPs o Pneumotonometers (Alcon) are based upon McKay-Marg principles and are also very accurate for abnormal corneal rigidity such as corneal edema, scarring, post-surgical, irregular corneal surface and thin/thick corneas. NCT (Air Puff Tonometer) In 1972, Bernard Grolman, OD, American Optical developed first non-contact, airpuff tonometer. Achieves corneal flattening by an air jet of calibrated, increasing force. Corneal flattening is detected by a photo cell. From the known force of the air jet and the dimensions of the air jet, the pressure is calculated. The higher the IOP, the longer it takes to flatten the cornea (i.e., if IOP = 17mmHg, flattening takes 10.5msec; if IOP = 36mmHg, flattening takes 24 msec). Newer machines use decreased force, so time is increased. In early 1970s, very few DPA laws had been passed. Designed to eliminate need for anesthetics, does not physically contact globe. Because of this and ease of operation, it is very commonly used in optometric practice. Three advantages of no ocular contact No need for anesthetic, no associated risks of anesthetic use such as toxicity and hypersensitivity No risk of abrasion No risk of disease spread on tonometer Applanation type of tonometer Measures time needed to flatten central cornea of constant area with puff of air of known force. IOP reading vs. the cardiac cycle Measures IOP in 1-3 msecs (1/500 of cardiac cycle) cannot average the IOP change with cardiac cycle unless multiple readings are acquired. Each reading is independent of the IOP change during the cardiac cyclecannot see the IOP cycle in GAT, cannot continuously measure as in pneumotonometers. Because of this it is not unusual to see readings vary by as much as 4mmHg. Advantages Very good accuracy for pressures in the normal range, if multiple readings are used No anesthetic needed Quick and easy to perform Can be delegated to a technician, and almost always is No ocular contact. Can be used on diseased eyes. Little aqueous displacement- repeat readings are generally accurate (though apprehension often increases with more readings) Disadvantages Expensive- $5,000 – 10,000 Requires separate table. Not portable. Patient apprehension (cant see puff coming). o Also, patient apprehension often increases after the first reading, unlike GAT. o Should obtain >3 readings per eye. The more readings, the greater the accuracy. Not accurate at high pressures. Measures lower. Random to cardiac cycle. o Should take a few readings and average Accuracy Very good screener tends to read slightly high but good correlation to Goldmann At high IOPs >30, reads false low Better to use GAT on glaucoma suspects, ocular hypertensives, glaucoma patients Other “air puff” tonometers Keeler Pulsair (handheld) Topcon Kowa Nidek Reichert Canon Rodenstock Pneumotonometer Two models were available: Alcon pneumotonometer (made by Digilab) and Digilab pneumotonometer. No longer made. Developed in 1970s Design Gas piston which forces gas or air down a flexible tube to the probe tip. Probe tip o Small in diameter, flat chamber with flexible membrane o As the membrane contacts cornea it conforms to the convex corneal surface driving the gas out of the chamber. o Gas is forced into the chamber, pressure needed to do this is measured IOP. Reading o Instrument can generate a continuous reading or continuously measure and digitally display the average. o Must leave the probe on the cornea for 5-10 seconds- good cooperation required. Advantages o Most accurate (along with MacKay-Marg tonometers) for abnormal corneal rigidity, irregular corneas- mostly used by ophthalmologists to measure IOP post-op. o Can use on sitting or supine patients o Fairly compact and portable. Disadvantages o Cost o Not generally as accurate as Goldmann o Technique dependent, though less than MacKay-Marg o Good patient cooperation necessary; good fixation for 5 seconds o Moderate displacement of aqueous- not recommended for operated measurements. o Constant force, measures areas applanated Prototype is Maklakov Tonomat is commonly used in USA All are high fluid volume displacement, thus large ΔP and Pt is not close to Po. Need conversion tables. Advantages Small, portable Very cheap Disadvantages Not good accuracy, not recommended o This is the second least accurate after Schiotz Technique dependent Clinical Aspects of Tonometry o When to take tonometric readings If the patient cannot/will not cooperate, record this. All yearly exams on all patients who can cooprate, including children. Always prior to DFE To ensure that IOPs are controlled prior to dilation To evaluate the degree of IOP change with dilation Glaucoma suspects As many readings at various times of the day as possible to detect diurnal spikes. o Instrument selection- aspects Greatest accuracy- Goldmann and handheld Goldmann (Kowa or Perkins) Most accurate at all IOP levels One of these should be the primary tonometer in the office. Use of DPAs is usually not a negative factor Patient preference- generally Goldmann Anticipation and apprehension is a negative factor against AO NCT and other airpuff tonometers. Ease of use- doctors generally prefer Goldmann, AO NCT can be used easily by all, even those unskilled. Scarred, edematous, thin/thick cornea- MacKay-Marg, MacKay-Marg variation (i.e., tonopen) or pneumotonometer After refractive surgery- MacKay-Marg (Tonopen) or pneumotonometer Soft (hydrogel) lenses- 1987 study suggests that Goldmann yields acceptable accuracy, however question of mechanical damage to lens remains Can remove lens, do GAT, irrigate well and replace lens (2 hour wait recommended) Can use NCT over the SCL Air puff tonometers (AO, Keeler, Topcon) seem best choice if SCLs cannot be removed, no backup spectacles. Small size, portable Handheld Goldmann- best accuracy o o o Tonopen Schiotz Recording tonometry findings Must be included in record of all patients who can and will allow tonometry Must be accurate and legible Must include (at least) Tonometer used Readings Time of day Dilated? If glaucoma patient, the time, dosage of glaucoma meds, name of meds, eyes of last administration of every glaucoma medication. The recording WNL is absolutely unacceptable since this cannot be determined by tonometry alone. If patient cannot cooperate, i.e., blepharospasm, document this in the record and why the patient cannot or will not. Do not simply leave the tonometry section blank. Patient refusal of tonometry Ensure that patient understands why it is recommended for all patients and document this in the record. Be sure to explain that the IOP may be elevated without other evidence of glaucoma- this must be detected ASAP and can only be detected by tonometry. Document thoroughly, including all patient education. Some doctors require the patient to sign a waiver form. Tonometer probe disinfection Contact tonometers such as Goldmann, Perkins, Schiotz are potential sources of cross contamination/ transmission of ocular disease and risk of transmission. Any anterior segment disease Any disorder where causative agent is in the tears of corneal epithelium EKC Hepatitis B HIV Effective modes of inactivation of HIV 10 minute soak of probe with 1:10 solution of sodium hypochlorite or 3% hydrogen peroxide or 70% ethanol or 70% isopropanol Thorough rinse with water Air dry Utilize gloves when in contact with body fluids including tears in high risk patients Advanced Tonometric Procedures Introduction o In some patients, routine tonometry is not adequate for either confirming a diagnosis or for continued management. o The two procedures which are not considered routine but may be necessary for good patient management are diurnal curves (aka serial tonometry) and the prone dark room provocative test (PDRP). There are other procedures and provocative tests. Diurnal Curves/ Serial Tonometry o A diurnal curve measures the fluctuation in a patient’s IOP over a given period of time. This generally refers to daytime hours, but sometimes may be over a 24 hour period. To perform a diurnal curve, the IOP is measured every 30 minutes, every 60 minutes, or every 2 hours throughout the day. The frequency of IOP measurements is controversial thus accounting for the variation in time. o Two significant patterns of diurnal curves exist for both nonglaucomatous patients and patients with galcuoma. In most patients, the high peak exists between 4am and 9am. However, there is a second group of patients reaching their peak between 9am and 5pm. Normal fluctuation in IOP is approximately 5mmHg. Variations in IOP in glaucoma patients is approximately 13mmHg. o Indications for Serial Tonometry LTG- before diagnosing a patient as having LTG, it is best to schedule a diurnal curve so as to establish the highest peak of IOP curve. Glaucoma patients who are apparently controlled (meaning by IOP alone which is not appropriate) yet continue to reveal progreswsive optic nerve cupping and VF loss should also be scheduled for a diurnal curve. Once again, the highest peak of the diurnal curve is established so as to further clarify whether or not current medical therapy is adequate or if additional medications/surgery is indicated. ACG o Patients predisposed to either acute angle closure or subacute angle closure are usually recognized prior to the precipitation of such as attack. This may be because of family history, moderate to high hyperopia, advanced nuclear sclerosis, or clinical examination. o Can one predict who will develop ACG, whether it occurs spontaneously or as a result of dilation? There are several provocative tests which may be utilized to predict which patients are at greatest risk for developing angle closure. The most physiologic and safest of these tests is the PDRP. o Indications for performing the PDRP Patients with gonioscopically narrow angles who are at risk for spontaneously closing an angle or for closing an angle as a result of papillary dilation should be scheduled for a PDRP. o PDRP Technique Measure the IOP. Patient then either lies prone or leans over a slit lamp facedown for 60-90 minutes in the dark with the eyes either open or closed. They must not fall asleep as this will invalidate the results. After the time has elapsed, the IOP is again measured. The patient should not be exposed to any unnecessary light when measuring the IOP as this will immediately open the angle. An increase in IOP of 8mmHg or more in one or both eyes is considered a positive finding. Patients with positive findings should be referred for surgical evaluation of a prophylactic peripheral iridectomy (PI). Patients with negative findings should be warned of the signs and symptoms of angle closure and informed to report to your office immediately if such symptoms are noticed. In addition, they should have periodically have the PDRP repeated. Several negative findings may be noted before a positive test found. Lab- IOP and Provocative Testing Objectives To identify factors which affect measured IOP To compare methods used for provocative testing in glaucoma suspects. To differentiate between provocative tests on the basis of reliability Required Equipment AO NCT Water and 1L flasks Penlight Dark room facility Tropicamide Provocative Testing Introduction o The diagnosis of glaucoma is often obscured by the variable clinical presentations which accompany ocular hypertension. The clinician is expected to differentiate between POAG, secondary OAG, and ACG. Distinguishing these types of glaucoma is dependent on hereditary factors, medical history, or history of trauma discussed during the case history. Clinically, the most important factors are the drainage angle, VF changes, optic disc appearance, and IOP. o Borderline cases of glaucoma can require provocative testing. Such tests are designed to increase IOP in glaucomatous eyes. Some techniques are most reliable for cases of early diagnosis. The tests vary in their application for differentiating open and closed angle glaucoma. o An 8mmHg or greater increase means a positive finding Procedure o Water Drink Test The subject fasts for six hours prior to the laboratory experiment. This provocative test for the diagnosis of POAG requires the examiner to measure the increase in IOP following imbibitions of one liter of water per 154lb body weight within 5 minutes. Increased blood pressure and venous pressure means there is a resistence to outflow. Decreased osmolarity and if eye stays the same, water enters the eye and increases the IOP. Data IOP Subj 1 (Mike) Subj 2 (Emily K) 0 min 13 14.5 15 min 13 18 30 min 12.5 23.5 45 min 15.5 23.5 60 min 12.5 17 o Dark Room Prone Provocative Test This test physiologically parallels activities which the patient normally experiences: darkness and the prone position. Pupil dilates (mydriasis) increases resistance to outflow (in both the TM and lens/iris). Maximum dilation is normally 6-7mm. When the eye is at the same level of the heart, the Part and Pven are increased, increasing the outflow resistance. Lens falls forward. This increases the resistance at that interface. Procedure Subject lies in prone position Subject raises head on hands or a pillow (prone position) in a totally dark room. Sleeping is not permitted and the eyes are kept open After 60 min, take IOP Data IOP, 0 min 11.5 13 Subj 1 (Lori) Subj 2 (John) o IOP, 60 min 14 15 Mydriasis Test A mydriatic agent is used and caution is necessary to avoid precipitating an ACG attack. However, tension may rise and outflow facility decrease in some cases of OAG. An assessment of the drainage angle with a gonioscope is necessary to obtain a differential diagnosis. Increase IOP because there is increased resistance at the TM and interface. Decreased IOP with OAG because an increased pupil pulls the TM to decrease resistance. Procedure Screen for narrow angles with a penlight or slit lamp. Instill 1 drop of 1% tropicamide. Record pressure at 15min intervals with the same instrument Data Subj 1 (Shirley) Subj 2 (Jennelle) 0 min 10 9 15 min 10.5 12.5 30 min 10 10.5 45 min 10.5 10.5 60 min 11.5 9.5 Variables Affecting Human IOP Introduction o Optometrists are responsible for the measurement and interpretation of the IOP of many patients. There are many variables which can affect the IOP value obtained. Here we will investigate some of the external and internal influences (aside from those discussed as provocative tests) on IOP. o Seating position Kriegelstein and Langham used a pneumatonograph to study the influence oof body position on the IOP. The pressure increment when changing from the seated to the supine position averaged 2.9mmHg in normal eyes and 3.9mmHg in glaucomatous eyes. Determine IOP change with position change from seated to supine. Use the seated IOP as baseline for the subject. o Corticosteroid Response 5% of the population have an increased IOP, but with glaucoma, there is an increase in 90%. Corticosteroid treatment of ocular disease has increased in popularity during recent years because of its anti-inflammatory effect on the eyelids, conjunctiva, cornea and anterior segment of the globe. Administration of corticosteroids, whether longterm therapy as in treatment for RA and skin and collagen diseases, or for local use as in the treatment of conjunctivitis, keratitis, or iritis can bring relief from discomfort caused by anti-inflammatory process. However, there are several severe complications if used indiscreetly over a long period of time. Usage of corticosteroids is contraindicated in HSV involvement due to a potentiation of the virus activity and a subsequent increase in the destructive effect of collagenase on the cornea. Other complications include a possible increased susceptibility to fungal infection, and spread of bacterial infection. PSC formation has been reported by Oglesby as a result of long term high dosage systemic corticosteroid therapy. The risk increased proportionately to the duration and amount of therapy. Topical ocular corticosteroids have been associated with an increase in IOP, a specific ocular complication of local therapy that occurs in genetically predisposed individuals. About 5% of the general population sustains a marked elevation of IOP while in contrast over 90% of patients with POAG develop an increase in IOP. Likewise, offspring of POAG patients show an increased incidence of high IOP in response to corticosteroids. Becker and Hahn have suggested that steroid responsiveness is inherited in a dominant manner. As a result of this, the abnormal corticosteroid response may provide helpful information in steroid provocative procedures, but it cannot be used as a definitive diagnostic test. Steroids are also contraindicated as a routine procedure due to the aforementioned secondary ocular involvements. There are several theories as to the etiology of the IOP elevation but it is commonly suggested that the mucopolysaccharide content of the TM might be altered with increased resistance to aqueous outflow. The elevated pressure in steroid glaucoma usually subsides when use of the steroid is discontinued. The form of glaucoma usually seen can be characterized by a painless increase in IOP, optic atrophy and VF loss. Cupping of the optic nervhead is frequently absent and the field defects are atypical of glaucoma. Clinical evidence implies that topical administration of corticosteroids should be used judiciously and only for short periods of time with strict supervision. o Other factors may influence IOP as well. Forced lid closre, forced coughing, bending over (valsalva maneuver), exercise, pressuring the non-tested eye, pupil miosis are activities which may alter measurements of IOP Procedure o Prone Position o o o o o o Data o Average 2.9 Forced Lid Closure Should increase because increased pressure on the eyes. Increased pressure means increased IOP. Forced Coughing 30 seconds preceeding the test Increases abdominal pressure, increasing venous pressure. It is hard to find a change since the IOP is measured after the cough. Valsalva Maneuver Muscular contractions of chest, abdomen and diaphragm in forced expiration against the closed glottis. Same as forced coughing. Increases internal pressure Exercise 15 push-ups or run in place for one minute Short term increases, long term decreases. Decreased because after exercise. Pupil Miosis Shine penlight into one eye for one minute Decreases because clearing measure. A treatment for glaucoma No change with POAG. Digital Pressure Digital pressure on OD, measure OS If increase in one eye, compensation decreases in both eyes. Subject 1- Kimberly M/ Subject 2- Julie K. Exercise Simple Seated Position Prone Position Forced Lid Closure Forced Coughing Valsalva Maneuver Exercise Pupil Miosis Digital pressure Subject 1/2 1 1 1 1 2 2 2 IOP, in mmHg 13 / 12.5 13.5 13.5 14 13.5 11 11 10.5 Discussion Questions 1. Cite factors which may create false positives or false negatives with the Water Drink Test. o Drinking either too much or not enough water o The position in which one is sitting during measurement, as well as level of relaxation o Effectiveness of aqueous drainage o Compensatory reaction 2. Do you feel that the Water Drink test is of value in thediagnosis of open angle glaucoma? Why or why not? o Yes, because it is of value. o Increased fluids leads to increased blood pressure, then increased arterial and venous pressure, then increased resistance to outflow, therefore increased IOP. 3. What are the advantages of the Dark Room Prone Provocative Test? o Pupils dilate, therefore increases resistance to outflow. o Since the eye is at the level of the heart, venous pressure increases, therefore increased outflow resistance. o With the head down, the lens falls forward, so there is an increased resistance at the lens/iris interface. 4. Discuss the anatomical/ physiological explanations thought to account for IOP changes with the Dark Room Prone Provocative Test. o See Question 3 5. What is the relationship between IOP and systemic blood pressure? o Short term: increased systemic blood pressure leads to an increased outflow resistance and increased IOP. o Long term: no proven relationship. o Tonopen or Pneumotonometer are best for post-op, scarred, edematous and thin/thick corneas. GAT not accurate. Pneumotonometry is very good for edematous, scarred, post-op corneas and appears to be best for children <10 y/o. Goldmann reads false low in children <10 years old. Factors affecting the accuracy of the IOP reading Tonometer used Corneal curvature GAT is calibrated for 44.00D o Steeper than 44.00 gives a false high IOP reading. Corneal rigidity/elasticity, thickness, scarring- false high Corneal thickness GAT is calibrated for an average central corneal thickness (CCT) of 0.52mm, but o Ultrasonic pachymeters show an average CCT of 0.544mm (+/0.034mm) o Optical pachymeters show an average CCT of 0.530mm (+/0.029mm) o Schiotz is even more influenced by rigidity. Thinner corneas lead to a false low IOP on GAT Thicker corneas lead to a false high IOP on GAT o Cadaver eye studies of thicker/thinner cornea demonstrate as much as 7 mmHg overestimation on thick corneas to 5 mmHg under on thin corneas. Correction factor o Various factors have been proposed, as little as 0.19 mmHg for every 10 micron change in thickness to as much as 0.71 mmHg for every 5 microns change. o Clinical Keys o Ocular hypertensives have false high GAT readings due to thicker than average corneas. Consider pachymetry. o LTG suspects may have falsely lower GAT readings. Consider pachymetry o Post-LASIK patients will have lower IOP readings than pre-op on GAT. This is a false low reading. The amount if controversial. Probably an average 2-3mmHg but it is quite variable. Valsalva Maneuver Straining, holding breath, lifting raises IOP Body inversion can substantially increase IOP Aerobic Exercise This can result in up to a 20% decrease in IOP. It is not sustained if the patient discontinues regular exercise. Additive to medications May enhance perfusion to ONH as well. Factors affecting IOP during measurement Accommodation/ near focus o Greatest in young, less in older o Can decrease IOP rapidly o Patient should fixate at a distance during tonometry Apprehension o Increased IOP o May be a significant factor in air puff tonometers o Increased IOP can also be due to holding breath and cocontraction of EOMs. Tight tie/collar leads to an increased IOP Holding lids/pressure on globe can cause a substantial raise in IOP. Corneal edema gives a false low IOP reading Corneal scarring also produces a false high IOP reading o Use MacKay-Marg, e.g., Tonopen or pneumotonometer if there is a scarred or edematous cornea. Recording Tonometry Always record the time of the IOP measurement to help detect diurnal spikes. Example: GAT 12/16 at 12:35pm If glaucoma therapy is started, it is very important to compare treated to untreated IOPs at similar times of the day due to the substantial diurnal IOP changes that can occur in patients, even treated patients. If on glaucoma meds, record the last time of administration of each glaucoma med. Example: GAT 12/18 12:50pm. Last Alphagan 1gt OD at 8:45am. Last T ½ 1gt OU at 8:30am.