A Case of Recurrent Anaphylaxis
advertisement

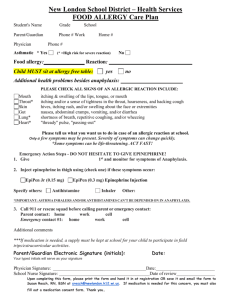
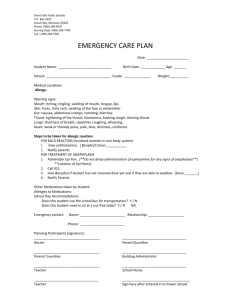
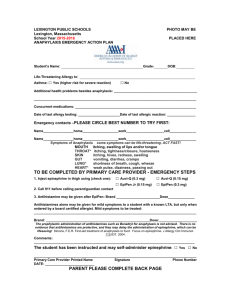
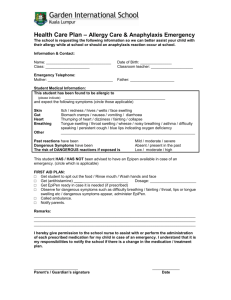
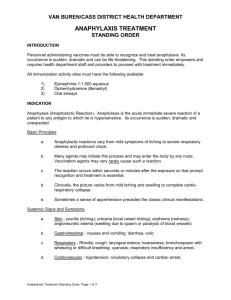
A Case of Recurrent Anaphylaxis Lynne M. Zheutlin, MD Case presentation History of present illness 43 YO WF seen in the ER six times for anaphylaxis Initial episode after gardening and taking a walk Developed swelling of hands and feet, trouble breathing and swallowing Treated with oxygen, IV Benadryl and prednisone History of present illness She presented to the ER 3 more times over the next 4 weeks. Breathing progressively worse with each. All began with swelling of hands and feet, but no urticaria. No consistent pattern of exercise or food ingestion before-hand. Used Epipen at onset of fourth episode; unknown benefit Developed pyschosis secondary to steroid treatment History of present illness She was seen first by another allergist. Diagnosed as vascular leak syndrome and referred to a vascular surgeon Fifth episode associated with loss of consciousness. Admitted to pulmonary service History of present illness CXR abnormal and TB suspected; PPD negative and diagnosis R/O Sent home on daily loratadine Sixth episode described as trouble breathing without swelling. Seen in ER and sent home Presented for a second opinion Past Medical History Pneumonia Bronchitis, sinusitis No hx of asthma or rhinitis or hives Bipolar disorder Hypertension Herniated cervical discs Stevens-Johnson Syndrome (tegretol) Rash from penicillin, Demerol, codeine Family HX negative for anaphylaxis or angioedema ROS positive only for mild cough Physical exam – BP 140/80, P 72, PF 400, mild pedal edema Skin testing for inhalants negative RAST from other allergist negative for foods Laboratory Findings (from other allergist) WBC 9000, Hgb 11.8, Hct 35.7, MCV 105, MCH 34.6, Normal diff Metabolic panel WNL Urinalysis 3+ occult blood, 15-20 RBC/HPF C1 esterase inhibitor 30 mg/dl (2840) C1q 13.5 (7.9-25) Anti-DNA (DS) Ab 25 U/ml (0-99) Hospital Records 6/28/03: Presented with swelling of throat and hands, shortness of breath, hoarseness, dizziness BP 143/84, P 95, R 28, O2 Sat 98% Exam showed swelling of uvula, tongue, hands, hoarse voice Lungs clear; no respiratory distress Meds: lithium, Depakote, Restoril, Cardizem, Vistaril, Nexium, Seroquel Hospital Records Treated with IV Decadron, epinephrine, Benadryl, Pepcid, 2L O2 Received second dose of epinephrine and Benadryl At discharge: BP 141/81, P78, R20, O2 Sat 99% Hospital Records 8/15/03 (fifth episode) Presented to ER with swelling of throat and tongue after a wasp sting. Noted to be lethargic. BP 146/85, P 110, R 19, O2 Sat 99% RX IV Solumedrol, epinephrine, Benadryl. WBC 26,000. Given Rocephin and admitted. Tequin begun. CXR: RUL infiltrate. CT scan: nodular disease RUL. PPD neg. At discharge WBC 10,000. Folate 7.1, Vit B12 505. Told to discontinue Seroquel. Began daily loratadine Follow-Up Reported one episode of shortness of breath and leg swelling in recovery room after back surgery. Treated with epinephrine and Benadryl. No further episodes for 4 months Current meds: Depakote, Restoril, Nexium, Benicar, Lithium, Celebrex, Vit B12. Taking Benadryl daily to prevent recurrence. Switched to Zyrtec. Follow-Up Phone call 7/8/04: Seen at Washington Adventist for 7th allergic reaction. Had eaten ice cream at a lacrosse game. Could not swallow, lost voice, swelling of hands and feet. Used Epipen. Received second dose of epinephrine in ER Idiopathic Anaphylaxis? No consistent history of food ingestion before episodes. RAST for common foods negative. Insect sting associated with only one episode. Should she be tested for hymenoptera? Seroquel considered as cause, but had reactions after discontinuation. No association with exercise Idiopathic Anaphylaxis Anaphylaxis with no definable etiology and not triggered by exogenous allergens 335 cases reported by AllergyImmunology Division, Northwestern University Categorized as idiopathic anaphylaxis- generalized or idiopathic anaphylaxis-angiodema. Further classified as frequent (>6/y) or infrequent Manifestations of Idiopathic Anaphylaxis Urticaria or angioedema Upper airway obstruction 335 100% 210 63% Bronchospasm 132 39% Hypotension or syncope Gastrointestinal Sx 78 23% 75 22% Therapeutic Regimen Idiopathic Anaphylaxis Infrequent episodes (<6/y): Treat acute episodes with epinephrine, prednisone and antihistamine Frequent episodes (>6/y): Initially prednisone 60 mg qAM, hydroxyzine 25 mg TID, albuteral 2mg TID, Epipen to carry After episodes disappear, prednisone converted to every other day and tapered by 5-10 mg monthly Questions Is this Idiopathic anaphylaxisangioedema? Should she receive prophylactic treatment? Could this be undifferentiated Somatoform IA? History mimics IA but lacks correlating objective physical findings, shows no response to therapeutic regimen, and meets criteria for undifferentiated somatoform disorder How does the history of psychosis secondary to corticosteroids impact treatment?