Chronic Kidney Disease & Diabetes for the practice nurse
advertisement

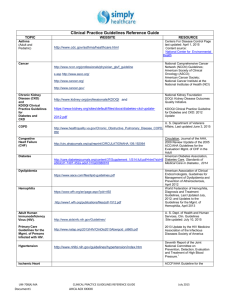
Chronic Kidney Disease & Diabetes for Primary Care Nurses Primary Care Nurse Workshop This workshop was conceived and developed by the Kidney Check Australia Taskforce sub-committee for education in nursing in general practice, with particular thanks to the KCAT team. Version 04.14 KCAT Supporters The KCAT program is proudly supported by unrestricted educational grants from: KCAT Program Partners KCAT Major Sponsor Learning Outcomes At the end of this workshop participants will: Know the eight major risk factors for Chronic Kidney Disease (CKD) Know how to measure kidney function and interpret the results Understand the adjustments to treatment targets and management of CKD in patients with diabetes Understand the signs of diabetic kidney disease and what role the practice nurse plays in its management Develop confidence to include CKD testing and management into the diabetes cycle of care 3 What is CKD? Chronic kidney disease is defined as: Glomerular Filtration Rate (GFR) < 60 mL/min/1.73m2 for ≥3 months with or without evidence of kidney damage. OR Evidence of kidney damage (with or without decreased GFR) for ≥3 months: • • • • albuminuria haematuria after exclusion of urological causes pathological abnormalities anatomical abnormalities. Kidney Disease in Australia Australians aged ≥ 18 years Dialysis or transplant 19,000 Less than 10% of these people are aware they have CKD 53,000 Stage 4-5 CKD 580,000 1,124,000 5+ MILLION AT RISK Stage 3 CKD Stage 1 – 2 CKD Hypertension / Diabetes Australian Health Survey 2013; ABS population estimates June 2012 CKD staging is according to the CKD-EPI equation The Australian CKD staging schema X Combine eGFR stage, albuminuria stage and underlying diagnosis to specify CKD stage (e.g., stage 3b CKD with microalbuminuria secondary to diabetic kidney disease) Colour-coded Clinical Action Plans Diabetic Kidney Disease (DKD) • When damage to the kidneys is caused by diabetes it is called Diabetic Kidney Disease (DKD) or diabetic nephropathy. • DKD can worsen other diabetic complications such as nerve and eye damage • DKD increases the risk of cardiovascular disease • It usually has no symptoms until it is well advanced Diabetic Kidney Disease (DKD) • DKD is the most frequent cause of kidney failure worldwide • DKD is associated with increased morbidity and mortality at all stages of CKD • Early detection and comprehensive management of DKD is associated with improved outcomes • CKD best care overlaps fully with cardiovascular risk reduction and best diabetes care CKD and diabetes Every second patient you see with Type 2 diabetes will have CKD (47%)* A patient with diabetes has CKD if they have: Persistent microalbuminuria or proteinuria An eGFR < 60mL/min/1.73m2 and/or Haematuria after exclusion of urological causes or structural abnormalities *NEFRON Study 2007 The increasing burden of CKD and diabetes Australia - 1981 to 2009 Number of new patients with ESKD due to diabetes starting on dialysis 900 800 700 600 500 400 300 200 100 0 Type2 Type 1 Diabetes is the cause of kidney failure that is largely driving the increase in dialysis patients in Australia 45 Diabetes Gn BP 40 Misc Uncertain PCK 35 Reflux Analg Nx Rate pmp 30 25 20 15 10 5 0 1998 2000 2002 2004 2006 2008 ANZDATA Registry Less than 1 in every 20 patients with diabetes and CKD will live long enough to require dialysis or transplantation* Finding an eGFR < 60 really means: High risk of heart attack or stroke Less likely to survive a heart attack More likely to be hospitalised in next 12 months Likely to have heart failure Wounds will heal more slowly Ankle swelling and fluid retention are more difficult to control BP targets more difficult to achieve Higher likelihood of fractures with a fall Adverse drug reactions more common While blood sugar levels easier to control – more likely to have a hypo *NEFRON Study 2007 Case Study Larry Case study - Larry Background • Larry is a 62 year old male of Caucasian background • He works full-time as a clerk in the Public Service • Larry presents at your general practice with an acute cough with yellow sputum • He has previously been seen at your practice when he accompanied his wife for an annual flu vaccination Case study - Larry Larry’s History • Larry has Type 2 diabetes that was diagnosed elsewhere a year ago after he presented with thirst • Smoking - 40 pack years (1 pack per day for 40 years) • Alcohol - consumes 7-10 drinks per week • Follows a “diabetic diet” • Is on no regular medications but takes occasional NSAIDS for back pain when needed. Today’s Visit Test Result Blood Pressure 160/90 mmHg Weight 102 kg BMI 31 kg/m2 Waist Circumference 110 cm Chest Findings Consistent with bronchitis - no clinical signs of COPD Case study - Larry Today’s Visit Larry’s GP found some of Larry’s results and history concerning. The GP has asked you to review Larry’s case further, looking at his potential risk for kidney disease. Q1: Is Larry at increased risk of kidney disease? If so, why? Risk factors for kidney disease Risk factors for CKD Diabetes High blood pressure Smoking Age over 60 years Obesity Aboriginal or Torres Strait Islander origin Family history of kidney failure Established cardiovascular disease Larry has 5 of the 8 risk factors for CKD 1 in 3 Australian adults is at increased risk of CKD due to the above risk factors! Diabetic kidney disease Q1a: What does Larry’s diabetes mean for his CKD risk? • 20-40% of patients with Type 2 diabetes develop nephropathy, which classically* occurs in 2 stages: Early nephropathy - microalbuminuria and normal-high GFR Overt nephropathy - macroalbuminuria and progressive decline in GFR * Recent data shows that 33% individuals with diabetes with eGFR <60ml/min/1.73m2 do not have albuminuria, and for these subjects, prognosis is similar to those with albuminuria1,2 1. Tapp RJ, Shaw J, Chadban SJ et al. Am J Kidney Dis 2004; 44:792-8 2. Agarwal et al, NDT 2011 Classical stages of diabetic kidney disease* *Those with Type 2 diabetes may have overt nephropathy at presentation GFR normal Albuminuria normal 0 5 10 Duration of Diabetes (years) 15 CKD risk factors - Smoking Q1b: How does smoking increase Larry’s risk of CKD? • Among individuals with diabetes, those who smoke are more likely to get albuminuria and among those with diabetic kidney disease, smoking accelerates progression to failure [1,2] • Even among the normal Australian population, smoking has been associated with kidney damage [3] [1] Gambaro et al. Diabetes Nutr Metab 2001;14:337. [2] Orth & Hallan. Clin J Am Soc Nephrol 2007. [3] Briganti et al. Am J Kidney Dis 2002;40:704. CKD risk factors - Hypertension Q1c: Larry has hypertension. What does this mean for his CKD risk? • Hypertension is extremely common among those with type 2 diabetes, particularly those with DKD • Among those with diabetes (and without), those with hypertension are 5-8 times as likely to have albuminuria • Achieving BP control is one of the most effective ways to delay the progression of kidney disease CKD risk factors - Obesity Q1d: Larry is obese. What impact does his weight have on his risk of CKD? • Overweight (BMI 25.1-30) and obese (BMI >30) people are 40% and 80% more likely to develop CKD compared to normal weight individuals [1] • Central obesity appears to be more important than generalised • Although not as powerful as diabetes or hypertension as a risk factor for kidney disease, obese subjects may be more likely to develop albuminuria and proteinuria • Obesity leads to greater difficulty in achieving tight glycaemic control and BP control [1] Wang Y et al. Association between obesity and kidney disease: a systematic review and meta-analysis. Kidney Int. 2008;73:19-33. CKD risk factors – NSAID use Q1e: Does Larry’s occasional NSAID use increase his risk of CKD? Probably not! • Chronic use of NSAIDs have not been proven to lead to CKD in humans • However, NSAID ingestion can aggravate underlying kidney disease and hypertension and risk of vascular events • Should be avoided in this setting CKD risk factors – Chest infection Q1f: Will Larry’s chest infection contribute to his likelihood of CKD? FALSE • Chest infection by itself has no relationship to CKD • Recurrent chest infections are more common in smokers • With this history of smoking Larry is highly likely to develop COPD in the future Checking for kidney damage Larry is at increased risk of kidney disease and you decide to test him for evidence of kidney damage. Q2: How would you test Larry for evidence of kidney damage? ? ? ? ? ? ? urine dipstick for blood and protein spot urine albumin/creatinine ratio (ACR) 24 hour urine protein serum creatinine eGFR renal ultrasound (kidney outline and size) Checking for kidney damage Answer: ? urine dipstick for blood and protein spot urine albumin/creatinine ratio (ACR) ? 24 hour urine protein serum creatinine eGFR ? renal ultrasound (kidney outline and size) Urine albumin /creatinine ratio (ACR) • The preferred urine test in all diabetics is to look for microalbuminuria • This is best tested by a urine albumin:creatinine ratio (ACR) • Preferably 1st morning void but a random sample can also be used ACR Result Test Results Range Recommended Follow -up Normal Females <3.5 mg/mmol Males <2.5 mg/mmol Re-test annually Microalbuminuria Females 3.5 – 35 mg/mmol Males 2.5 – 25 mg/mmol Repeat 2 times over 3 months Confirm microalbuminuria if 2 out of 3 tests are positive Macroalbuminuria Females >35 mg/mmol Males >25 mg/mmol Do a protein:creatinine ratio (PCR) or 24 hour urine protein (to quantify protein excretion) (also called proteinuria) NHMRC Guidelines 2009 Serum Creatinine & eGFR • The serum creatinine result (taking allowance for age and sex) is converted to an eGFR automatically by all Australian path labs and reported as numerical value or >90mL/min/1.73m2. • eGFR is accurate at values <60, but tends to underestimate true GFR in those with diabetes with true GFR>60. • Creatinine alone will commonly under-estimate the degree of reduction in kidney function, particularly in small elderly women. Comparing eGFR and Creatinine CKD 1&2 Serum creatinine CKD 3 120 90 Albuminuria 60 GFR mL/min CKD 4 CKD 5 30 Normal Serum Creatinine Level Actual Serum Creatinine Level 0 Dialysis Who should be tested for kidney disease? Risk Factor Recommended Tests Frequency Urine ACR eGFR Blood Pressure Every 1-2 years* Smoker Diabetes Hypertension Obesity Established cardiovascular disease Family history of kidney failure Aboriginal or Torres Strait Islander origin aged over 30 years *yearly for people with diabetes or hypertension If an individual has multiple risk factors, follow the more frequent regime Summary of tests for kidney disease Kidney Health Check Blood Test Urine Test Creatinine & eGFR Albumin / Creatinine Ratio (ACR) to check for albuminuria BP Check Blood Pressure should be consistently below 130/80 mmHg for people with diabetes or albuminuria Case study - Larry You identified Larry as being at increased risk for CKD and requested he be recalled for further tests. Larry’s tests results show the following: Test Creatinine Result 135 µmol/L eGFR Urine ACR HbA1c Blood Pressure 46 mL/min/1.73m2 44 mg/mmol (macroalbuminuria) 9.6% / 81 mmol/mol 160/90 mmHg Larry - kidney damage Q3: What do you do about Larry’s high blood pressure? Hypertension control in diabetes Answer a) Lifestyle approaches are the first consideration in all people with diabetes and high blood pressure - the key elements are: ‘SNAP’ (smoking, nutrition, alcohol, physical activity) A low salt diet An exercise program A low calorie diet to reduce his BMI A reduction in his alcohol intake Stop smoking Lifestyle modification effects on BP Modification Recommendation Approx SBP reduction Weight reduction BMI 18-24.9 kg/m2 5-20 mmHg / 10kg lost Dietary salt restriction <100 mmol/day 2-8 mmHg DASH* diet Fruit, vegies, low saturated and total fat 8-14 mmHg Physical activity Aerobic activity for 30mins most days 4-9 mmHg Moderate alcohol consumption only 1-2 standard drinks/day 2-4 mmHg * Dietary Approaches to Stop Hypertension Hypertension in diabetes Answer b) Medications may be needed to lower blood pressure to target levels The preferred anti-hypertensive agents in diabetes are an ACE-inhibitor or ARB These agents may also slow progression of CKD Any other anti-hypertensive agent that lowers blood pressure down to target will improve the patient’s future. As Larry has diabetes and albuminuria, his blood pressure should be maintained consistently below 130/80 Larry’s management plan Q4: How could you improve Larry’s diabetes control? Good glycaemic control slows progression of kidney failure* • Prescribe exercise and diet • 44% of patients are on a sulphonylurea • Metformin okay to use in reduced doses when eGFR is between 30 and 60 mL/min - avoid use if GFR below 30 mL/min, due to risk of acidosis • Consider referral to endocrinologist and diabetes education centre See Diabetes Australia website for guidelines: www.diabetes.com.au *UKPDS. Lancet 1998;352:837-53 How to incorporate CKD into your systems? • Annual cycle of care • Quarterly nursing review • Annual nursing review • GP management plans • Team Care Arrangements Diabetes - Annual cycle of care Diabetes Management in General Practice 11/12 Quarterly Nursing Review Quarterly Nursing Review – Routine Visit Ask About: Check: Review: • • • • • Smoking Nutrition Alcohol intake How much exercise and how often Any problems with medication • • • • Weight / Waist Height (children & adolescents) Blood Pressure Feet examination without shoes, if new symptoms or at risk (eg neuropathy+- peripheral vascular disease) • Goals with patient to identify specific areas of focus for doctor consultations Diabetes Management in General Practice 11/12 Annual Nursing Review Yearly Nursing Review – More detailed assessment Ask About: • • • • • • • • • • • • Smoking Nutrition (last contact with dietician or diabetes educator) Alcohol intake How much exercise and how often Any problems with medication Any changes in medication (by doctor / pharmacist or patient) Chest pain Vision (when last checked) Any foot discomfort When was last podiatry check Immunisations (include Flu and Pneumovax) Family history and update Check: • • • • • • • Weight / Waist Height (children & adolescents) Blood Pressure Feet examination without shoes, pulses, monofilament check Blood glucose at examination Urinalysis Visual Activity Review: • Goals with patient to identify specific areas of focus for doctor consultations • Last care plan to identify timely referrals Diabetes Management in General Practice 11/12 GP Management Plans (GPMP) Medicare Australia has provided remuneration for chronic disease management by the following item numbers: • 721, 732, 729 & 732 for patient & GP Management of a single or multiple chronic conditions that incorporate the patient’s needs, goals, details of achievement & references to any resources. Electronic templates are available via medical software and Medicare Locals. • 723, 732 & 10997 for involving other Health Professionals in the Management Plan, including the Practice Nurse. • For more information visit www.health.gov.au Item 10997 - Practice Nurse & Aboriginal Health Worker monitoring & support For provision of monitoring & support to people with a chronic disease by a practice nurse or registered Aboriginal Health Worker, on behalf of a GP. • Available for people who have a GPMP / TCA • A maximum of 5 services can be claimed per patient per calendar year. • The item may be used to provide: • Checks on clinical progress (eGFRs, ACR, BP) • Monitoring medication compliance (BP medication(s)) • Self management advice (BMI target, exercise, diet) and • Collection of information to support GP reviews of Care Plans. www.health.gov.au Role of the practice nurse Assist in the Management of CKD by • Promote self management strategies (lifestyle modification) • Assist with adherence to treatment to slow progression of CKD • Screen and manage diabetes and hypertension • Assessment of Absolute Cardiovascular Risk www.cvdcheck.org.au • Monitor for nephrotoxic medications (e.g. NSAIDs) • Assess and manage symptoms (e.g. anaemia, nausea/vomiting) • Monitoring and support under current Medicare Item Number(s) Larry – GPMP Q5: Which other health professionals could you involve in your management of Larry through a Team Care Arrangement? Multidisciplinary Team May include, but is not limited to: • • • • • Practice Nurse • General Practitioner • Dietitian • Family Members / Carers • Community Health (weight & • diet programs specific to local • community) • • Exercise Physiologist • • Quitline • • • Nephrologist Optometrist/ Ophthalmologist Endocrinologist Diabetes Specialist Renal Nurse Nurse Practitioner Pharmacist Podiatrist Social Worker Vascular/ Transplant Surgeon Cardiologist Larry’s management plan Q6: GPMPs recommend review every 3-6 months. What will you review when Larry returns for his next visit? Quarterly Nursing Review – Routine Visit Ask About: Check: Review: GPMP reviews assist behavioural change. Set up a recall / reminder system • • • • • Smoking Nutrition Alcohol intake How much exercise and how often Check medications (prescribed & OTC) • • • • Weight / Waist Height (children & adolescents) Blood Pressure Feet examination without shoes, if new symptoms or at risk (eg neuropathy+- peripheral vascular disease • Goals with patient to identify specific areas of focus for doctor consultations Systems to identify patients with diabetes and CKD • Practice nurses have opportunities to screen high risk patients in the primary care setting • Web based tools: • eGFR calculator (www.kidney.org.au) • Absolute CVD calculator (www.cvdcheck.org.au) • Data extraction tools for general practice • Pen Clinical Audit Tool (CAT), Canning Tool • Link to most GP desktop systems • Medicare Locals can provide access and support Summary: CKD and diabetes All people with diabetes should have an annual kidney health check The targets of therapy (blood pressure, glycaemia etc) may differ in those with DKD Major role for practice nurse in coordinating a multidisciplinary approach Kidney disease an integral part of chronic disease management Marked overlap with CVD risk reduction and diabetic strategies Encourage self management wherever possible Potential to halve the number of patients presenting with kidney failure Further Resources… CKD Management in General Practice 2012 Guidelines booklet Diabetic Kidney Disease patient fact sheet Available along with other kidney health fact sheets at www.kidney.org.au > For Patients > Health Fact Sheets Kidney Health Information Service Free call information service for people living with / affected by kidney disease Join the Kidney Community… KIDNEY COMMUNITY members receive a monthly newsletter from KHA allowing you to access: Information and invitations to KHA's education and support activities Updates on medical research in kidney disease Updates on clinical trials and research opportunities Information on advocacy opportunities and government relations issues Information on community and corporate events held by Kidney Health Australia To join the kidney community, email community@kidney.org.au