reflex
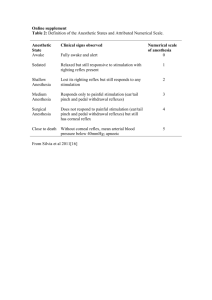
advertisement

Principles of anatomical structures and function of nervous system. Unconditioned reflexes. Active movements system (symptomatic and topical diagnostics of movement disturbances) Prof. S.І. Shkrobot Neurology as science Neuropathology (from Greek neuro – nerve, pathos – disease, logos – science) – is a part of clinical medicine, which is involved in nervous diseases and its role in pathology of other organs and systems of human body Functions of nervous system The main function of nervous system is unification and regulation of different physiological processes. That means that nervous system unites, integrates and subordinates all the parts of human body and provides its connection with environment. Functions of nervous system The base of nervous system activity is reflex principle Reflex – is a reaction of our organism to various outside and inside effects. It is provided by nervous system. Reflex consists of: afferent part (which accepts information) central part (that keeps information) efferent part (that creates response). As a result we have a circle – like structure receptor (primary information centre) – programme centre – executive apparatus. Reflex arche Reflexes are divided into: simple and complex inborn and trained conditioned and unconditioned Unconditioned reflexes: They are inborn ones They are phylogenetically old, that means they were formed in course of phylogenesis They are based on certain anatomic structures (segments of spinal cord or brain stem) They exist even without brain cortex influence They are inherited They can be regulated by brain cortex They are basis for the conditioned reflexes Conditioned reflexes: They are the result of the individual experience and are formed during ontogenesis They are unstable, that means they need constant support They aren’t based on certain anatomic structures They are fixed in brain cortex There are such conditioned reflexes as speaking, writing, reading, calculation, practice Unconditioned reflexes are divided into: Superficial and deep Simple and complex Unconditioned reflexes are divided into: Proprioceptive (stretch, periosteal, joint) Exteroceptive (dermal, from mucouse membrane) Interoceptive (from mucouse membrane of internal organs – for example urination in case of internal sphincter irritation) In clinical practice we evaluate the following reflexes: Reflex The group reflex Subeyesbrow Deep, reflex Corneal (lid) Nerves Segments periostal M. orbicularis N. trigeminus ( V ) Medulla oculi – N.facialis (VII) oblongata pons Superficial, mucose membrane Jaw Jerk Deep, (mandibular, chin, reflex masseter) reflex (Bechterev’s) of Muscles from M. orbicularis N. trigeminus ( V ) Medulla oculi – N.facialis (VII) oblongata pons periostal M.masseter N. trigeminus ( V ) Medulla – N.mandibularis oblongata (sensory and motor pons ) Pharyngeal Superficial, mucose membrane from Mm. constrictores pharyngis and others N.glossoMedulla pharyngeus, oblongata n.vagus (sensory and motor), 9th and 10th pair of CCN Palatal (palatine) Superficial, mucose membrane from Mm. levatores N.glossoMedulla velli palatini pharyngeus, oblongata n.vagus (sensory and motor) and and and Biceps Deep, reflex stretch M.biceps brachii N.musculocutaneus C5-C6 Triceps Deep, reflex stretch M.triceps brachii C7-C8 Radial (carporadial, Deep, periostal Mm.pronatores brachioradial) reflex flexores, digitorum, brachioradialis, biceps N.radialis N.medianus, N. C5-C8 radialis, N. musculocutaneus Scapulo- humeral Deep, periostal Mm. teres N. (scapuloperiosteal) reflex major, subscapularis reflex (Bechterev’s) subscapularis C5-C6 Upper superficial Superficial, abdominal dermal Mm. N.intercostales transversus, obliquus, rectus abdominis D7-D8 Middle superficial Superficial, abdominal dermal Mm. N.intercostales transversus, obliquus, rectus abdominis D9-D10 Lower superficial Superficial, abdominal dermal Mm. transversus, obliquus, rectus abdominis N.intercostale s D11-D12 Cremasteric M.cremaster N.genitofemoralis L1-L2 Knee jerk, or Deep, stretch M.quadriceps patellar reflex reflex femoris (quadriceps stretch reflex) N.femoralis L3-L4 Achilles jerk) N.tibialis (n.ischiadicus S1-S2 Superficial, dermal (ankle Deep, stretch M.triceps reflex surae Plantar (sole) Superficial, dermal Mm. flexores N.ischiadicus digitorum pedis and others L5-S1 Anal Superficial, dermal M.sphinter ani Nn. externus anococcygei S4-S5 Motor system Provides conduction of nervous impulse from brain cortex to muscles. The way of this impulse is known as motorway or tractus corticomuscularis. It consists of two neurons: central peripheral Upper and lower extremities, neck, trunk and perineum muscles’ innervation The first (central) neuron is called tractus corticospinalis. The second (peripheral) neuron is called tractus spinomuscularis. The first (central) neuron The first (central) neuron tractus corticomuscularis tractus corticomuscularis Spinal nerve gives 4 branches: ramus anterior ( together they form plexus – cervical, brachial, lumbar and sacral) ramus posterior (it is spinal nerve, which innervates posterior trunk muscles) ramus meningeus ramus comunicante albi Conclusions: The muscles of upper and lower extremities have unilateral cortical innervation from contralateral hemisphere The muscles of neck, trunk and pelvic organs have bilateral innervation from both hemispheres. In case of unilateral pathologic focus these structures do not suffer Face, tongue and pharynx muscles innervation This way is called tractus corticomuscularis. The first central neuron is called tractus corticonuclearis. The second peripheral one is called tractus nucleomuscularis. Face, tongue and pharynx muscles innervation We can make the following conclusions: 1. The face muscles have bilateral cortex innervation except the mimic muscles and tongue muscles that have unilateral innervation from the opposite hemisphere. 2. The muscles of upper and lower extremities, lower mimic muscles and tongue muscles have unilateral cortical innervation. 3. All the other muscles (the muscles of neck, trunk, perineum, m. oculomotorial, m. masseter, pharyngeal and palatal muscles) have bilateral cortical innervation. Paralysis Paralysis (plegia) - means the absence of active movements. It occurs in case of complete lesion of motor way (tractus corticomuscularis) . Paresis occurs in case of incomplete lesion of motor way. That means disorders of active movements Clinically can be – hemi-, tetra-, mono-, triand paraparesis. Paralysis is divided into: Central (spastic) Peripheral (flaccid) Central or spastic paralysis is caused by the lesion of central neuron and its fibers (tr. corticospinalis or tr. corticonuclearis). Peripheral or flaccid paralysis is caused by the lesion of peripheral neuron (tractus spinomuscularis or tractus nucleomuscularis). Features of central (spastic) paralysis are: 1. It is a diffuse paralysis 2. There is spastic hypertonus of muscles 3. Hyperreflexion of stretch and periostal reflexes 4. There are pathologic reflexes. They are considered to be reliable signs of central paralysis 5. Protective reflexes (the reflexes of spinal automatism) 6. Pathologic synkinesis is involuntary movements in paralysed extremity Paresis Paresis Spastic hypertonus features: Tonus is increased in the group of flexors in upper extremities and in the group of extensors in lower extremities “clasp – knife“ symptom in course of evaluation tonus decreases Flexing pathological reflexes Bechterev’s sign Jukovski sign Rossolimo (Venderovych) reflex Rossolimo (Venderovych) reflex Jukovski sign Extension pathological reflexes Extension pathological reflexes Pathologic reflexes on upper extremities: Bechterev’s sign. This is simply a musclestretch reflex of bending of fingers obtained by tapping the back of hand with a reflex hammer. Jukovski sign. This is caused by hammer impact on a palm under fingers; response is reflex flexing of II-V fingers. Rossolimo (Venderovych) reflex: This is simply a muscle-stretch reflex obtained by tapping the palmar surfaces of the fingers with a reflex hammer; the response is reflex flexing of II-V fingers. Pathologic reflexes on upper extremities: Tremner reflex. This is simply a muscle-stretch reflex obtained by tapping the palmar surfaces of the nail-phalax of II – V fingers. The response is fingers flexing. Jakobson – Laske reflex. This is caused by hammer impact on processus styloideus; the response is reflex flexing of II-V fingers. Klipel – Veil reflex. This is caused by passive bending of II – V fingers. The response is thumb flexing Protective reflexes (the reflexes of spinal automatism ) They also are one of signs of lesion of motor way. They are especially clearly expressed at cross lesion of a spinal cord (dissociation of underlaying segments of the last from a brain). The result is squeezing of foot, and also an injection or sharp plantar flexion of toes (V.M.Bechterev). The response reflex flexion of paralyzed extremities, flexion in femoral, knee and talocrural joints (shortly reaction); opposite extremities thus straightens, being unbent in joints (long reaction). Serial putting irritations on one and the other leg, can result in imitation of automatisms of walking. Pathologic synkinesis - are involuntary movements in paralysed extremity . They are observed while moving by healthy extremity. Synkinesis are divided into: Global Coordinatory Imitating Central paralysis Features of peripheral paralysis 1. Areflexion or hyporeflexion 2. Atonia or hypotonia 3. Muscular atrophy 4. Fasciculation of muscles 5. It is limited paralysis 6. There is reaction of degeneration. Types of gate: Symptoms of motor way lesion 1. The lesion of anterior central gyrus monoplegia (or monoparesis) on the opposite side. If the focus is situated in upper part of anterior central gyrus, paralysis of lower extremity occurs. If it is in middle part of anterior central gyrus, we can observe paralysis of upper extremity. If it is in lower one, face suffers. In case of anterior central gyrus irritation Motor Jackson takes place. Motor Jackson is a set of local seizures that can cause generalized seizures. Symptoms of motor way lesion 2. The lesion of radiate crown central hemiplegia on the opposite side (that means that arm, leg, lower mimic muscles and tongue muscles are involved). Paralysis can dominates in lower extremity,in upper extremity or in face muscles Besides hemianesthesia can join hemiplegia. Symptoms of motor way lesion 3. The lesion of internal capsule part of motor way hemiplegia on the opposite side, central paresis of tongue muscles and lower mimic muscles Hemihypesthesia often joins all the other symptoms. Vernike – Mann posture is typical for this lesion. Hemianopsia Symptoms of motor way lesion 4. The lesion of brain stem alternating syndrome- central paralysis on the opposite side and peripheral paralysis of face muscles on the side of lesion. The last are divided into peduncle, pontine and bulbar ones. 5. The lesion of pyramidal decussation part of motor way central paralysis of upper extremity on the side of lesion and paralysis of lower extremity on the opposite side. Sometimes tetraplegia or triplegia is observed. Symptoms of motor way lesion 6. The lesion of motor way in lateral funiculus of spinal cord central paralysis below the level C1-C4, C5-Th1, Th1- Th12, L1-S2 7. The lesion of anterior horns or motor nucleus of CNs peripheral paralysis of certain muscles with fasciculation of muscles. Also there are early atrophy and degenerative reaction. 8. Anterior roots lesion peripheral paralysis. In most of cases it is observed only when several roots are damaged. Symptoms of motor way lesion 9. The lesion of nerve plexus peripheral paralysis , pain, sensory and autonomic disturbances 10. The lesion of peripheral nerve peripheral paralysis of the muscle , innervated by this nerve, pain, sensory and autonomic disturbances.