Chapter 21 General Embryology
advertisement

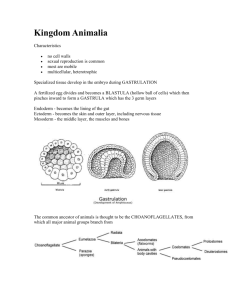
Chapter 21 General Embryology ---a science which study the processes and regulations of development of human fetus.(from 1 cell(zygote) to (5-7)X1012 cells ) ---total 38 weeks: preembryonic period: before 2 weeks embryonic period: 3-8 weeks fetal period: after 9 weeks *perinatal stage: 26 weeks to birth *Teratology: abnormal development of fetus 1.Fertilization ---definition: the process by which the male and female gametes(sperm and ovum) unite to give rise to zygote ---place: in the ampullary region of the fallopian tube ---conditions: 1) maturation of oocyte 2) maturation of spermatozoon: /ductus epididymus: 2-3 weeks, forward motility protein 3) capacitation of spermatozoa: decapacitation factor: exist in epididymus, to inhibit the release of acrosome enzymes capacitation factor: secreted by epi. cells of oviduct, capacity of releasing acrosome enzymes 4) quality and quantity of spermatozoa: 2-6 ml, 100,000,000/ml, <1.5 ml; or <10,000,000; abnormal sperm >30%; or capacity for mobile< 70% 5) meeting of sperm and ovum sperm: 20-24h ovum: 15-18h(1-3ds) ---processes of fertilization: 1) acrosome reaction: /hyaluronic acidase: dissolve corona radiate * interact with ZP3(receptor glycoprotein, exist in zona pellucide) molecules, release /acrosin: dissolve zona pellucide /enter perivitelline space 2) spermatozoa fuse with the membrane of ovum: nucleus enter cytoplasm of ovum 3) monospermy: cortical reaction: cortical granules(located in cytoplasm of ovum) are released into perivitelline space, and cause zona reaction: change of ZP3 molecules in zona pellucide 4) formation of zygote(fertilized ovum) secondary meiosis complete: form second polar body male pronucleus fuse with female pronucleus, to restore the 2n chromasome ---significance of fertilization: 1) a new life begin(initiation of cleavage) 2)restoration of the diploid number of chromosomes: cross-over 3) determination of the sex of the new individual: ova(22+X) + X-bearing spermatozoon = girl ova(22+X) + Y-bearing spermatozoon = boy *klinefelter’s syndrome: 47XXY, 48XXXY 2. Blastocyst formation and implantation 1) cleavage and blastocyst formation ①cleavage ---blastomere: cells formed by cleavage /30h: 2 /40h: 4 /72h: 12-16- morula ②formation of blastocyst: by 5th day, blastomere reach to 107, small space appear between them ---blastocoele: filled with liquid ---trophoblast ---inner cell mass ---polar trophoblast 2) Implantation ---definition: the process by which the blastocyst is embedded in endometrium ---time: 5th –6th day begin; 11th –12th day complete ---processes: zona pellucide disappear → polar trophoblast touch the endometrium→secrete proteolytase →dissolve the endometrium → embedded into endometrium→coagulation plug seal the space * trophoblast become into two layers when blastocyst is embedding into endometrium syncytiotrophoblast cytotrophoblast ---place: /posterior wall of fundus and body of uterus placenta praevia ectopic pregnancy ---decidual response of endometrium /stroma cell→predecidual cell→decidual cell(cell become larger and rich in glycogen and lipid droplet) /endometrium →decidua: -decidua basalis -decidua capsularis -decidua parietalis ---conditions: /endometrium is in secretory phase /morula reach the cavity of uterus on time /zona pellucide disappears in time 3. Formation and differentiation of trilaminar germ disc 1) formation of endoderm and ectoderm: early of 2 weeks, inner cell mass differentiate into two layers of cells ---bilaminar germ disc: epiblast(columnar) +hypoblast(cuboidal) ---epiblast: primary ectoderm /amniotic membrane: amnioblast /amniotic cavity /amniotic fluid /amnion ---hypoblast: primary endoderm /extraembryonic endoderm→exocoelomic membrane→primary yolk sac → exocoelomic vesicle /extraembryonic mesoderm: → extraembryonic cavity: chorionic cavity -visceral layer -parietal layer /secondary yolk sac: yolk sac ---body stalk: formed by extraembryonic mesoderm 2) formation of mesoderm: early of 3 weeks ---primitive streak: cells of epiblast proliferate to form a longitudinal arranged cell cord ---primitive groove ---primitive node ---primitive pit ---mesoderm: intraembryonic mesoderm ---endoderm: hypoblast cells are replaced by epiblast cells ---ectoderm: epiblast changed the name into ectoderm * trilaminar germ disc: endoderm + mesoderm + ectoderm * determination of head and tail of germ disc ---head process→notochordal tube → notochord ---buccopharyngeal membrane ---cloacal membrane 3)differentiation of trilaminar germ disc: 4th –8th weeks ---differentiation: same cells which are primordial and inmuture differentiate into different cells which have specific structure and function ---induction: some tissues effect the differentiation, and determine the differentiating orientation of another tissue ① differentiation of ectoderm: from 18th –19th days ---neural plate: neuro-epithelium(neural ectoderm): pseudostratified columnar epi. ---neural fold ---neural groove ---neural tube: →CNS /anterior neuropore: closed by 25th days /posterior neuropore: closed by 27th days ---neural crest(mesoectoderm): two lines of cell cords→ganglion ②differentiation of mesoderm: 17th days ---paraxial mesoderm somite: 20th days, 3 pairs/per day, 42-44 pairs by the end of 5th weeks -sclerotome: →bone, cartilage -myotome: →skeletal muscle -dermatome: dermis and hypodermis ---intermediate mesoderm: →kidney and reproductive gland nephrotome: segmentation nephrogenic cord: ---lateral mesoderm: intraembryonic coelom: →body cavity somatic or parietal mesoderm: →muscle, CT, parietal layer of pleura, peritoneum and pericardium splanchnic or visceral mesoderm: →muscle, CT of digestive tract, visceral layer of pleura, peritoneum and pericardium ---mesenchyme: →cardiovascular and lymph system ③differentiation of endoderm: ---primitive gut: →digestive, respiratory and urinary system 4. The development of fetal membrane and placenta 1) chorion: ---formed by trophoblast and extraembryonic mesoderm ---primary stem villus: projections of cytotrophoblast and syncytiotrophoblast ---secondary stem villus: extraembryonic mesoderm enter the primary stem villus * chorionic plate: trophoblast + extraembryonic mesoderm * chorion: secondary stem villus + chorionic plate ---tertiary stem villus: extraembryonic mesoderm differentiate into CT and BV free villus: branches anchoring villus ---cytotrophoblastic cell column: →cytotrophoblastic shell ---chorion leave: 6 weeks later ---chorion frondosum ---hydatidiform mole ---chorion carcinoma 2) yolk sac: ---blood island: primitive blood cell- derived from extraembryonic mesoderm on the wall of yolk sac ---primordial germ cell: derived from endoderm of yolk sac 3) amnion: ---amniotic membrane: amniotic extraembryonic mesoderm epi. + ---amniotic fluid: /secrete by amniotic epi. /slight basic fluid: 500-1000ml -polyhydramnios: >2000 ml, abnormal digestive system or CNS -oligohydramnios: <500 ml, abnormal urinary system /function: -intraenvironment -protecting -preventing from adherence -wash germ tract 4) allantois ---allantoic A: paired, →umbilical A ---allantoic V: paired right: degenerate left: umbilical V 5) umbilical cord ---cylindrical structure ---surface: amniotic membrane ---cord: mucous CT, umbilical A,V, yolk sac and allantois ---40-60 cm long, 1.5-2.0 cm in D ---> 80 cm, or < 35 cm 6) placenta: ---the structure by which exchange of material between fetus and mother takes place ---size: round, disc-shaped, 15-20 cm in D, 2.5 cm thickness, 500g in weight fetal surface: smooth, covered by amniotic membrane mother surface: rough, 15-30 cotyledons ---structure: /chorionic plate /chorion and chorion space -chorion: 60 chorion stalks→branches -chorion space: space between chorion, filled with mother blood /basal plate: cytotrophoblastic shell + deciduas -placental septa: separate the chorion into cotyledon ---blood circulation of placenta fetus: umbilical A →cap. of chorion →umbilical V mother: spiral A → chorion space → uterus V * placental barrier: /the structure between fetal and maternal blood /components: -endothelium of chorion capillary and its basal lamina -CT in the core of the villus -trophoblast epithelium and its basal lamina ---function: a. the exchange of material between the maternal and fetal blood streams b. defense barrier c. the production of hormones: /human chorionic gonadotropin, HCG: -begin: end of 2nd week -highest lever: 9th –11th week -lowest lever: 20th week, until birth /human placental lactogen, HPL -similar to HGH -highest lever: 36th –37th week /human placental progesterone, HPP and human placental estrogen, HPE -begin: 4th month /other hormones: human chorionic thyrotropin, HCT; human chorionic adrenocorticotrophic hormne, HCATH; prostaglandin