Blepharitis types, diagnosis & managment
advertisement

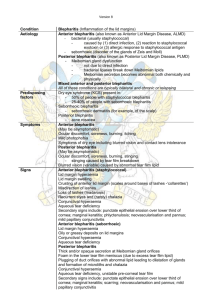
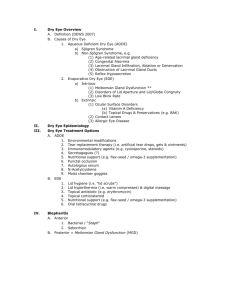
Mahmood J Showail Blepharitis is inflammation or infection of the eyelid margins . it is one the most common ophthalmological complications as well as one of the most difficult conditions to treat. I will discuss blepharitis according to its predominant anatomic location, as anterior or posterior. 1. Anterior Staphylococcal• Seborrhoeic• 2. Posterior Meibomianitis• Meibomian seborrhoea• Anterior blepharitis is characterized by inflammation at the base of the eyelashes . Patients with anterior blepharitis, compared to those with posterior blepharitis, are more likely to be female and younger * * McCulley, JP, Dougherty, JM, Deneau, DG. Classification of chronic blepharitis. Ophthalmology 1982; 89:1173. Two variants of anterior blepharitis are identified: staphylococcal and seborrheic. In staphylococcal anterior blepharitis, colonization of the eyelids by staphylococci leads to formation of fibrinous scales and crust around the eyelashes. The seborrheic variant is characterized by dandruff-like skin changes around the base of the eyelids, resulting in greasy scales around the eyelashes. The pathophysiology of blepharitis is not completely understood. A role for lid-colonizing staphylococcal bacteria was first noted in 1946 . Several mechanisms by which staphylococci may alter meibomian gland secretion and cause blepharitis are supported by many studies . Direct infection of the lids Evoke reaction to staphylococcal exotoxin Provoke allergic response to staphylococcal antigens . It is likely that a combination of these is responsible for the clinical manifestations of staphylococcal blepharitis. symptoms burning , grittiness and mild photophobia with remission and exacerbation is characteristic . Symptoms are usually worse in the morning , although in patients with dry eye they may increase during the day . note : because of poor correlation between the severity of symtpmos and clinical signs it can be difficult to objectivley assess the benefit of treatment . A. Staphylococcal blepharitis Hard scales and crusing mainly located around the bases of the lashes esp. collorette chronic conjunctival hyperemia with mild papillary conjunctivitis . Staphylococcal blepharitis Chronic irritation worse in morning• Scales around base of lashes • (collarettes) Hyperaemia and telangiectasia of • anterior lid margin Scarring and hypertrophy if • longstanding scarring and notching (tylosis) of the lid margin , trichiasis (misdirected eyelashes), madarosis (loss of lashes) or poliosis (loss of pigmentation of lashes) in sever long standing cases secondary changes include stye formation , marginal keratitis and occasionally phlyctenulosis (Corneal nodulesthat developed near the limbus and then spread onto the cornea, carrying behind them a leash of vessels) . associated with tear film instability and dry eye . Hyperemic and greasy anterior lid margin with sticking together of lashes the scales are mainly scruf , and located any where on the lid margin and lashes . Seborrhoeic blepharitis Shiny anterior lid margin• Hyperaemia of lid margin• Greasy scales • Lashes stuck together• The diagnosis of blepharitis is clinical, based on the patient's history and physical examination findings. There are no confirmatory diagnostic tests or laboratory investigations. The history should include questions about symptom duration, smoking, allergens, contact lenses, and use of retinoids which may provoke or exacerbate symptoms. A history of acne, rosacea, or eczema should be evaluated . The patient's facial and scalp skin should be examined for findings typical of seborrheic dermatitis (itching and flaking scalp or facial skin) or acne rosacea (facial flushing, broken or swollen blood vessels on cheeks and nose, and a red or swollen nose). There is little evidence to support any particular protocol for anterior blepharitis . Patient should be advised that lifelong treatment may be necessary and that permenent cure is unlikely . But control of symptoms is usually possible . Lid hygiene 1. • warm compresses applied for several minutes to soften crusts at the bases of the lashes . • Lid cleaning to mechanically remove crusts involve scrubbing of the lid margins once or twice daily with a cotton dipped in a dilute solution of baby shampoo or NaHCO3 . • Commercially produced soap/alcohol impregnated pads for lids scrubs are available . 2.Antibiotics *Topical sodium fucidic acid , bicarbonate or chlormaphinicol : used to treat acute folliculitits but is of limited value for long standing cases Azithromycin (500mg daily for 3 days ) may be helpful to control ulcerative lid margin disease . *Oral 3. Weak topical steroids Such as flurometholone 0.1 % QID for 1 week is usful for patients with sever papillary conjunctivitis , marginal keratitis and phlyctenulosis . 4. Tear substitutes Required for associted tear film instability and dryness Posterior blepharitis, the more common condition, is characterized by inflammation of the inner portion of the eyelid, at the level of the meibomian glands . It is often described as meibomian gland dysfunction. MG are modified sebaceous glands located within the tarsal plates . These holocrine glands are responsible for secretion of the oily layer of the tear film. This oily layer prevents tear evaporation and reduces the surface tension of the tear layer, thereby facilitating the spread of tears over the ocular surface . It is critical for normal ocular surface lubrication. Posterior blepharitis is caused by meibomian gland dysfunction and alteration in miebomian gland secretion . Bacterial lipase may result in the formation of free fatty acid . This increase in the melting point of meibum preventing its expression from the glands, contributing to occular surface irritation and possibly enabling growth of S. aureus . Loss of the tear film phospholipid that act as a surfactant result in increased tear evaporation and unstable tear film . there is poor correlation between severity of symptoms and the clinical signs . symptoms : Similar to anterior blepharitis Signs : * Excessive and abnormal meibomian gland secretion which may manifest as capping of meibomian gland orifices with oil globule . pouting, recession or pulgging of the meibomian gland orifices with hyperemia and telangictasis of the posterior lid margin Inflamed and blocked meibomian gland orifices Plugging of meibomian gland orifices pressure on the lid margin result in expression of meibomian fliud that may be turbid or appear like tooth paste . In sever cases the secretions become so inspissated that expression is impossible . Toothpaste-like plaques from meibomian glands the tear film is oily and foamy and froth may accumelate on the lid margin or inner canthi . Oily and foamy tear film Foam in meibomian seborreha Chalazion Which maybe multiple and recurrent , is common particularly in patient with posterior blepharitis . Tear film instability and dry eye Is found in 30-50% of patients probably as aresult of imbalance between the aques and lipid components of the tear film allowing evaporation . Tear film break up tim eis typically reduced . Epithelial basement membrane defects Cutaneous acne rosacea is often ass. With MGD Seborrhoeic dermatitis is present >90% of patients with seborrhoeic blepharitis Acne vulgaris : due to treatment with isoretinoin Contact lens intolerance Long-term contact lens wear is associated with posterior lid margin disease . posterior blepharitis is often found in association with skin conditions such as rosacea and seborrheic dermatitis . Rosacea is associated with plugging and hypertrophy of the sebaceous glands. Since the meibomian glands are modified sebaceous glands, rosacea may lead directly to meibomian dysfunction . Seborrheic dermatitis is also associated with inflammation of the meibomian glands. Its very important to tell the patient that cure is unlikely although remession may be achived . 1.Lid hygine As in anterior blepharitis with emphasis on messaging the lid to express acumilated meibum, the messaging is toward the lid margin edge to “milk” meibum . 2. Systemic tetracycline Are the mainstay of treatment . It is used mainly to block staphylococcal lipase production . It is particularly idicated in patients with recurrent phlyctenulosis and margina keratitis . Note , tetracycline sohuld not be used in Children less than 12 yrs Pregnant women Lactating women due to “ staining of bone and teeth & dental hypoplasia Types of tetracycline : Oxytetracycline : 250mg BD for 6-12 wks Doxycycline : 100mg BD for1wk then daily for 6-12 wks Minocycline : 100mg daily for 6-12 wks Erythromycine : 250 mg daily or BD “ may be used in children “ 3. Topical glucocorticoids There may be a role for topical glucocorticoid use in the short term treatment of acute blepharitis exacerbations. Patients should generally be evaluated by an ophthalmologist prior to its initiation “ to adjust benefit VS S/E “ 4. Topical cyclosporine Topical cyclosporine 0.05 percent eye drops were approved for the treatment of dry eyes by the US FDA in 2002 . Several studies have investigated off-label use of these drops in the treatment of blepharitis with promising results. Topical cyclosporine use has led to reduction in symptoms , and improved clinical findings in patients with posterior blepharitis [1,2]. Its has a high cost , so it should be reserved to refractory cases only . (1) Rubin, M, Rao, SN. Efficacy of topical cyclosporin 0.05% in the treatment of posterior blepharitis. J Ocul Pharmacol Ther 2006; 22:47. (2) Perry, HD, Doshi-Carnevale, S, Donnenfeld, ED, et al. Efficacy of commercially available topical cyclosporine A 0.05% in the treatment of meibomian gland dysfunction. Cornea 2006; 25:171. Several topical medications are under evaluation as treatment for blepharitis. Topical metronidazole is a potential substitute for the use of systemic antibiotics, especially in cases of blepharitis related to rosacea * Cohen, EJ. Cornea and external disease in the new millennium. Arch Ophthalmol 2000; 118:979. Topical tacrolimus ointment has been used to treat severe refractory blepharitis with good results (1) Development of effective tear lipid substitutes may palliate the symptoms of blepharitis (2) 1 . Joseph, MA, Kaufman, HE, Insler, M. Topical tacrolimus ointment for treatment of refractory anterior segment inflammatory disorders. Cornea 2005; 24:417. 2. McCulley, JP, Shine, WE. Changing concepts in the diagnosis and management of blepharitis. Cornea 2000; 19:650. Allergic blepharitis — Allergic blepharitis is an acute inflammatory reaction of the skin of the eyelids, usually occurring as a reaction to a contact irritant . The skin of the eyelids will be typically very red, swollen and itchy. Treatment is aimed at identifying and eliminating use of the offending agent. Demodex folliculorum — Demodex is a parasite that commonly inhabits the eyelash follicle in patients with and without blepharitis . Although this parasite can cause some changes in the eyelash follicles esp. sleave scales , but still there is no evidence that it is directly associated with blepharitis Picture demonstrating thinning of eyelids secondary to corticosteroid use. Note sleeves and scurf Sebacous gland carcinoma — Blepharitis is nearly always bilateral. A malignant tumor of the lid skin (ie, sebaceous cell carcinoma) should be suspected in a patient with persistent unilateral eyelid inflammation Other symptoms of malignancy include failure to respond to treatment, a nodular mass, ulceration, extensive scarring, or conjunctival nodules surrounded by inflammation www.UptoDate.com Ophthalmology Hyper guide Kanski, Clininal Ophthalmology